Blank 1915 C Assessment PDF Template
The 1915(c) Independent Behavioral Health Assessment form is a comprehensive tool designed to gather detailed information on an individual's mental and behavioral health status. This meticulously structured document covers a wide array of aspects crucial in understanding the unique needs and challenges faced by those seeking behavioral health services. Starting with demographic details, it extends to in-depth inquiries regarding behavioral health history, including chief complaints, presenting problems, and relevant history to paint a clear picture of the client's current situation. It delves into past psychiatric and placement history, substance use history, and physical health conditions, providing a holistic view of the individual's health. Legal status, family history, trauma experiences, living situation, and educational or employment status are thoroughly assessed to ensure all factors contributing to the client's well-being are considered. The form also evaluates social history, community integration, and current mental status through detailed examinations. Risk assessment, cultural and language preferences, principal diagnoses, and an interpretive summary further enrich the data collected, guiding the development of personalized treatment plans. This assesses not only the immediate needs but also outlines the client's recovery preferences and recommended services, emphasizing a tailored approach to behavioral health support.
Preview - 1915 C Assessment Form
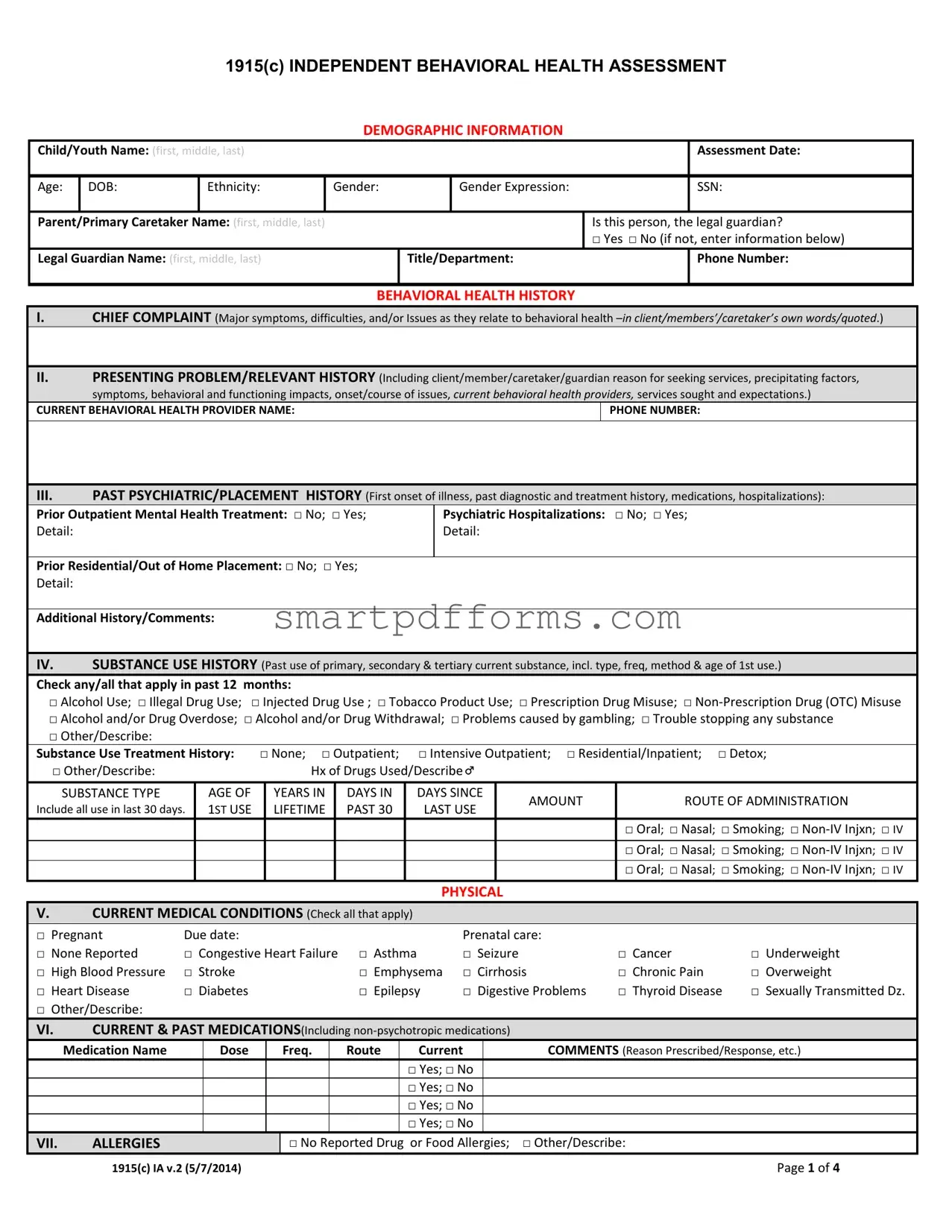
1915(C) INDEPENDENT BEHAVIORAL HEALTH ASSESSMENT
DEMOGRAPHIC INFORMATION
Child/Youth Name: (first, middle, last) |
|
|
Assessment Date: |
||
|
|
|
|
|
|
Age: |
DOB: |
Ethnicity: |
Gender: |
Gender Expression: |
SSN: |
|
|
|
|
|
|
Parent/Primary Caretaker Name: (first, middle, last)
Legal Guardian Name: (first, middle, last)
|
Is this person, the legal guardian? |
|
|
□ Yes □ No (if not, enter information below) |
|
Title/Department: |
|
Phone Number: |
|
|
|
BEHAVIORAL HEALTH HISTORY
I.CHIEF COMPLAINT (Major symptoms, difficulties, and/or Issues as they relate to behavioral health
 II. PRESENTING PROBLEM/RELEVANT HISTORY (Including client/member/caretaker/guardian reason for seeking services, precipitating factors, symptoms, behavioral and functioning impacts, onset/course of issues, current behavioral health providers, services sought and expectations.)
II. PRESENTING PROBLEM/RELEVANT HISTORY (Including client/member/caretaker/guardian reason for seeking services, precipitating factors, symptoms, behavioral and functioning impacts, onset/course of issues, current behavioral health providers, services sought and expectations.)
CURRENT BEHAVIORAL HEALTH PROVIDER NAME: |
PHONE NUMBER: |
|
|
III.PAST PSYCHIATRIC/PLACEMENT HISTORY (First onset of illness, past diagnostic and treatment history, medications, hospitalizations):
Prior Outpatient Mental Health Treatment: □ No; □ Yes; |
Psychiatric Hospitalizations: □ No; □ Yes; |
Detail: |
Detail: |
|
|
Prior Residential/Out of Home Placement: □ No; □ Yes; |
|
Detail: |
|
|
|
Additional History/Comments: |
|
IV. SUBSTANCE USE HISTORY (Past use of primary, secondary & tertiary current substance, incl. type, freq, method & age of 1st use.)
Check any/all that apply in past 12 months:
□ Alcohol Use; □ Illegal Drug Use; □ Injected Drug Use ; □ Tobacco Product Use; □ Prescription Drug Misuse; □
□Alcohol and/or Drug Overdose; □ Alcohol and/or Drug Withdrawal; □ Problems caused by gambling; □ Trouble stopping any substance
□Other/Describe:
Substance Use Treatment History: |
□ None; □ Outpatient; |
□ Intensive Outpatient; □ Residential/Inpatient; □ Detox; |
|||||
□ Other/Describe: |
|
|
Hx of Drugs Used/Describe |
|
|
||
|
|
|
|
|
|
|
|
SUBSTANCE TYPE |
AGE OF |
|
YEARS IN |
DAYS IN |
DAYS SINCE |
|
|
|
AMOUNT |
ROUTE OF ADMINISTRATION |
|||||
Include all use in last 30 days. |
1ST USE |
|
LIFETIME |
PAST 30 |
LAST USE |
||
|
|
|
|||||
|
|
|
|
|
|
|
□ Oral; □ Nasal; □ Smoking; □ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
□ Oral; □ Nasal; □ Smoking; □ |
|
|
|
|
|
|
|
□ Oral; □ Nasal; □ Smoking; □ |
PHYSICAL
V.CURRENT MEDICAL CONDITIONS (Check all that apply)
□ Pregnant |
Due date: |
|
Prenatal care: |
|
|
□ None Reported |
□ Congestive Heart Failure |
□ Asthma |
□ Seizure |
□ Cancer |
□ Underweight |
□ High Blood Pressure |
□ Stroke |
□ Emphysema |
□ Cirrhosis |
□ Chronic Pain |
□ Overweight |
□ Heart Disease |
□ Diabetes |
□ Epilepsy |
□ Digestive Problems |
□ Thyroid Disease |
□ Sexually Transmitted Dz. |
□ Other/Describe:
|
VI. |
CURRENT & PAST MEDICATIONS(Including |
|
|
||||||
|
|
|
||||||||
|
|
Medication Name |
Dose |
|
Freq. |
Route |
Current |
|
COMMENTS (Reason Prescribed/Response, etc.) |
|
|
|
|
|
|
|
|
□ Yes; □ No |
|
|
|
|
|
|
|
|
|
|
□ Yes; □ No |
|
|
|
|
|
|
|
|
|
|
□ Yes; □ No |
|
|
|
|
|
|
|
|
|
|
□ Yes; □ No |
|
|
|
|
VII. |
ALLERGIES |
|
|
□ No |
Reported Drug |
or Food Allergies; |
□ Other/Describe: |
|
|
1915(c) IA v.2 (5/7/2014) |
Page 1 of 4 |
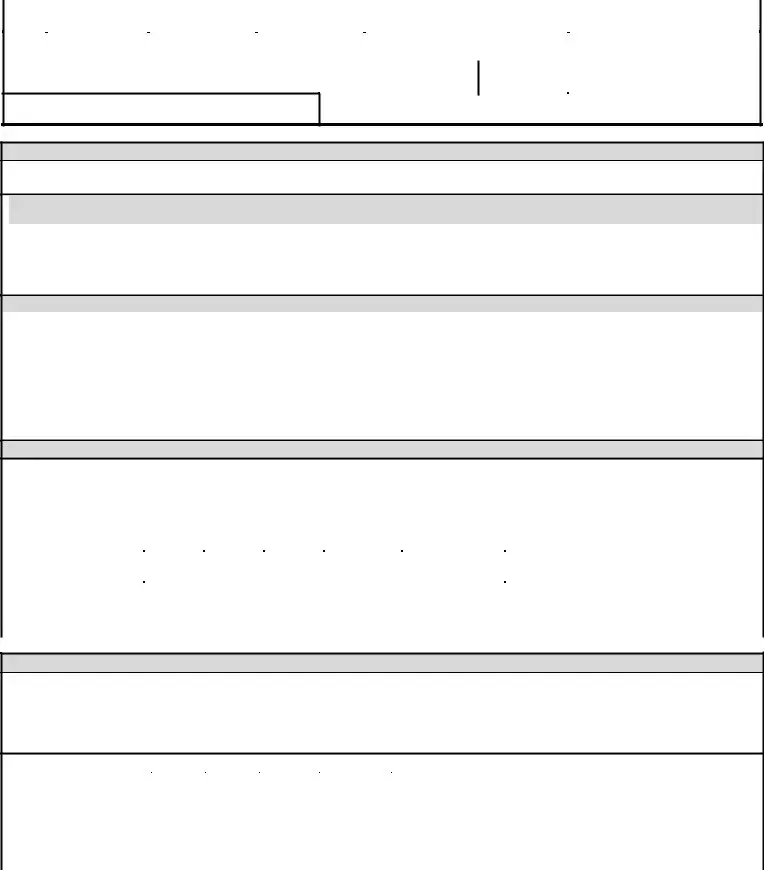
1915(C) INDEPENDENT BEHAVIORAL HEALTH ASSESSMENT
VIII. |
PRIMARY CARE PHYSICIAN |
NAME |
PHONE |
|
FAX |
|
|
|
|
|
|
IX. |
ADDITIONAL SIGNIFICANT MEDICAL HISTORY (Diagnosis, Hospitalizations, Surgery, labs values, status of conditions, etc.) |
|
|||
|
|
|
|
|
|
SOCIAL
X.LEGAL STATUS
Current Legal Status: □ None; □ Probation; □ Charges Pending; □ DCFS;
□OJJ; □ Other
Comment/Detail:
Past Legal Status: □ None; □ DCFS; □ OJJ; □ Other
Comment/Detail:
|
XI. |
FAMILY HISTORY (relationship status with relatives, family involvement in treatment, and living status of significant relatives): |
|
|
|
|
|||
|
Custodial Status: □ Independent Adult; □ Biologic Father; □ Biologic Mother; □ Joint Biologic Parents; □ Gov’t/Judicial; □ Other: |
|
||
|
|
|
|
|
|
Adverse Circumstances in Family of Origin: |
□ N/A; □ Poverty; □ Criminal Behavioral; □ Mental Illness; □ Substance Use; □ Abuse; □ Neglect; |
|
|
|
|
|
□ Domestic Violence; □ Violence; □ Trauma; □ Other/Describe: |
|
Summarize family history and
XII. |
TRAUMA HISTORY |
|
History of Trauma: □ None; □ Experienced; □ Witnessed; □ Abuse; □ Neglect; □ Violence; □ Sexual Assault;
□Other/Describe:
Summarize trauma history:
XIII. |
LIVING SITUATION (Current status and functioning) |
|
a.Primary Residence: □ Parent/Guardian Home; □ Relative’s Home; □ Out of Home placement; □ Homeless; □ Other/Describe:
How long at current residence? Family/Household Composition:
b.Summarize current living situation:
|
XIV. |
EDUCATIONAL/EMPLOYMENT STATUS |
|
|
|
a. |
Current Educational Placement/Employer: |
|
|
|
Current or Highest Grade Completed/Degree: |
|
|
|
|
|
Difficulties with Reading/Writing: □ No; □ Yes; |
Estimated Literacy Level: |
|
b. Summarize educational history and status:
.
XV. |
SOCIAL HISTORY AND COMMUNITY INTEGRATION |
|
a.Current status and functioning (Involvement in the community, social supports and activities, social barriers)
Does Client/Member feel supported by friends or family? □ Yes; □ No;
Recreational Activities:
b.Summarize social and community involvement:
CURRENT STATUS
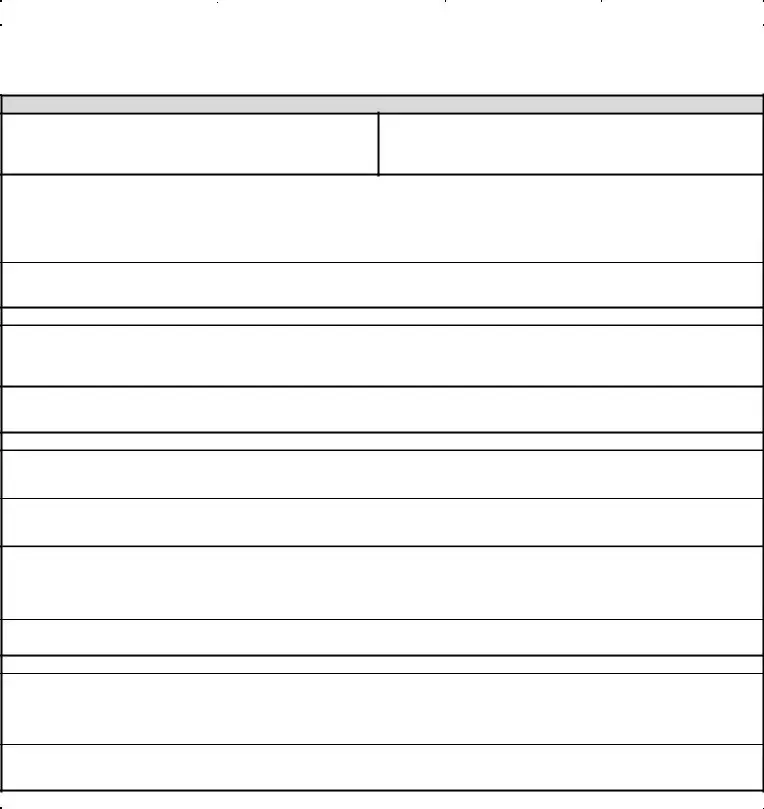
XVI. |
MENTAL STATUS EXAMINATION |
|
(Circle or Check all that apply.) |
|
|
|
|
a. GENERAL APPEARANCE |
□ Healthy; □As stated Age; |
□ Older Than Stated Age; □ |
□ Tattoos; |
□ Disheveled; □ Unkempt; |
|||
|
□ Malodorous; □ Thin; |
□ Overweight; |
□Obese; □ Other/Describe: |
|
|
|
|
b. BEHAVIOR & PSYCHOMOTOR ACTIVITY |
□ Normal; |
□ Overactive; □ Hypoactive; |
□ Catatonia; |
□ Tremor; |
□ Tics; □ Combative; |
||
|
□ Other/Describe: |
|
|
|
|
|
|
c. |
ATTITUDE □ Optimal; |
□ Constructive; □ Motivated; |
□ Obstructive; □ Adversarial; |
□ Inaccessible; |
□ Cooperative; □ Seductive; □ Defensive; |
||
|
1915(c) IA v.2 (5/7/2014) |
|
|
|
|
Page 2 of 4 |
|
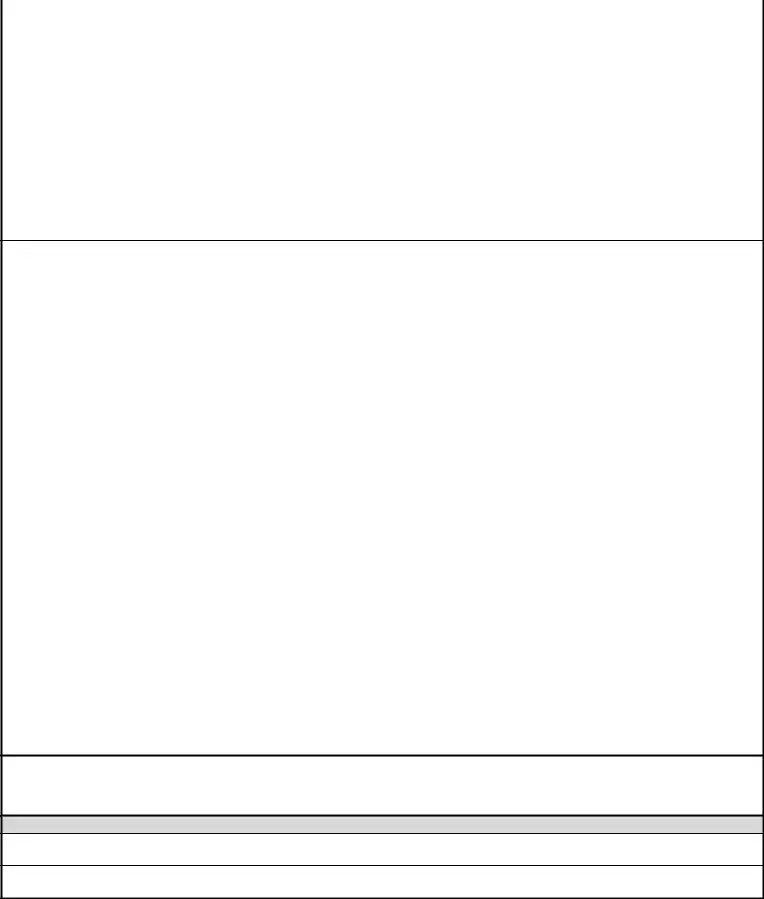
1915(C) INDEPENDENT BEHAVIORAL HEALTH ASSESSMENT
|
□ Hostile; |
□ Guarded; |
□ Apathetic; |
□ Evasive; |
□ Other/Explain: |
|
|
|
|
|
|
|
|
|||||
d. SPEECH |
□ Normal; |
□ Spontaneous; □ Slow; |
□ Impoverished; |
□ Hesitant; □ Monotonous; |
□ Soft/Whispered; □ Mumbled; □ Rapid; |
|||||||||||||
|
□ Pressured; □ Verbose; □ Loud; □ Slurred; □ Impediment; |
□ Other/Describe: |
|
|
|
|
|
|||||||||||
e. |
MOOD: |
□ Dysphoric; |
□ Euthymic; |
□ Expansive; □ Irritable; |
□ Labile; |
□ Elevated; □ Euphoric; |
□ Ecstatic; □ Depressed; □ Grief/mourning; |
|||||||||||
|
□ Alexithymic; □ Elated; |
□ Hypomanic; |
□ Manic; □ Anxious; □ Tense; |
□ Other/Describe: |
|
|
|
|||||||||||
|
|
|
|
|
|
|
||||||||||||
f. |
AFFECT |
□ Appropriate; |
□ Inappropriate; □ Blunted; □ Restricted; |
□ Flat; □ Labile; |
□ Tearful; □ Intense; |
□ Other/Describe: |
||||||||||||
|
|
|
|
|
|
|
||||||||||||
g. PERCEPTUAL DISTURBANCES □ None; |
Hallucinations: |
□ Auditory; |
□ Visual; |
□ Olfactory; |
□ Tactile; |
|
||||||||||||
|
□ Other/Describe: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
h. THOUGHT PROCESS |
□ Logical/Coherent; |
□ Incomprehensible; |
□ Incoherent; |
□ Flight of Ideas; |
□ Loose Associations; □ Tangential; |
|||||||||||||
|
□ Circumstantial; |
□ Rambling; |
□ Evasive; |
□ Racing Thoughts; |
□ Perseveration; |
□ Thought Blocking; |
□ Concrete; |
|||||||||||
|
□ Other/Describe: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
i. THOUGHT CONTENT |
|
□ Preoccupations; |
□ Obsessions; |
□ Compulsions; |
□ Phobias; |
□ Delusions; |
□ Thought Broadcasting; |
|||||||||||
|
□ Thought Insertion; |
□ Thought Withdrawal; □ Ideas of Reference; |
□ Ideas of Influence; |
□ Delusions; |
|
|
||||||||||||
|
□ Other/Describe: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
j. SUICIDAL/HOMICIDAL IDEATION □ Suicidal Thoughts; □ Suicidal Attempts; □ Suicidal Intent; □ Suicidal Plans; □ History of
|
|
□ Homicidal Thoughts; □ Homicidal Attempts; |
□ Homicidal Intent; |
□ Homicidal Plans; |
|
|
|
|
|
|
||||||
|
|
□ Other/Describe: |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
k. SENSORIUM/COGNITION |
□ Alert; |
□ Lethargic; □ Somnolent; |
□ Stuporous; |
Oriented to: □ Person; □ Place; □ Time; |
□ Situation; |
|||||||||
|
|
□ Normal Concentration; □ Impaired Concentration; |
□ Other/Describe: |
|
|
|
|
|
|
|||||||
|
|
l. MEMORY |
Remote Memory: □ Normal; □ Impaired; |
Recent Memory: □ Normal; □ Impaired; Immediate Recall: |
□ Normal; |
□ Impaired |
||||||||||
|
|
|
|
□ Other/Describe: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
m. INTELLECTUAL FUNCTIONING (Estimate) □ Above Avg.; □ Normal/Avg.; □ Borderline; |
Mental Retardation: □ Mild; □ Moderate; |
□ Severe |
||||||||||||
|
|
□ Other/Describe: |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
n. JUDGMENT |
□ Critical Judgment Intact; □ Impaired Judgment; |
□ Other/Describe: |
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|||||||||
|
|
o. INSIGHT |
□ True Emotional Insight; |
□ Intellectual Insight; □ Some Awareness of Illness/symptoms; □ Impaired Insight; □ Denial; |
|
|
|
|||||||||
|
|
□ Other/Describe: |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
p. IMPULSE CONTROL □ Able to Resist Impulses; |
□ Recent Impulsive Behavior; □ Impaired Impulse Control; □ Compulsions; |
|
|
|
||||||||||
|
|
□ Other/Describe: |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
XVII. |
RISK ASSESSMENT: Assess potential risk of harm to self or others, including patterns of risk behavior and/or risk due to personality factors, substance use, |
|
|
|||||||||||
|
|
|
criminogenic factors, exposure to elements, exploitation, abuse, neglect, suicidal or homicidal history, |
|
|
|
||||||||||
|
|
a. |
a. Risk of Harm to Self: |
□ Prior Suicide Attempt; |
□ Stated Plan/Intent; □ Access to means (weapons, pills, etc.); |
□ Recent Loss; |
||||||||||
|
|
|
□ Presence of Behavioral Cues (isolation, giving away possessions, rapid mood swings, etc.); |
□ Family History of Suicide; □ Terminal Illness; |
||||||||||||
|
|
|
□ Substance Abuse; □ Marked lack of support; □ Psychosis; |
□ Suicide of friend/acquaintance; □ Other/Describe: |
|
|
|
|
||||||||
|
|
b. |
b. Risk of Harm to Others: □ Prior acts of violence; □ Destruction of property; □ Arrests for violence; □ Access to means (weapons); |
|||||||||||||
|
|
|
□ Substance use; □ Physically abused as child; □ Was physically abusive as a child; □ Harms animals; □ Fire setting; |
□ Angry mood/agitation; |
||||||||||||
|
|
|
□ Prior hospitalizations for danger to others; □ Psychosis/command hallucinations; |
|
|
|
|
|
|
|||||||
|
|
|
□ Other/Describe: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c. |
Client/Member Safety & Other Risk Factors: □ Feels unsafe in current living environment; □ Feels currently being |
|
|
|
|
|||||||||
|
|
|
harmed/hurt/abused/threatened by someone; □ Engages in dangerous sexual behavior; □ Past involvement with Child or Adult Protective |
|||||||||||||
|
|
|
Services; □ Relapse/decompensation triggers; |
|
|
|
|
|
|
|
|
|
||||
|
|
|
□ Other/Describe: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
d. |
□ Inappropriate sexual behaviors |
□ Sex offender status |
□ Pending sex offense charge |
□ Report or Investigation □ Other: _ |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
e. |
Additional Risk Factors |
|
|
|
|
|
|
|
|
|
|
|
|
|
f.Describe recipient’s preferences and desires for addressing risk factors, including any Mental Health Advance Directives or plan of response to periods of decompensation/relapse (Ex. Resources recipient feels comfortable reaching out to for assistance in a crisis.):
XVIII. CULTURAL AND LANGUAGE PREFERENCES (Language, Customs/Values/Preferences)
a.Spiritual Beliefs/Preferences:
b.Cultural Beliefs/Preferences:
1915(c) IA v.2 (5/7/2014) |
Page 3 of 4 |
1915(C) INDEPENDENT BEHAVIORAL HEALTH ASSESSMENT
|
XIX. |
PRINCIPAL DIAGNOSES |
|
|
|
|
AXIS I |
|
|
|
|
|
|
|
|
|
|
|
AXIS II |
|
|
|
|
|
|
|
|
|
|
|
AXIS III |
|
|
|
|
|
|
|
|
|
|
|
AXIS IV |
|
|
|
|
|
|
|
|
|
|
|
AXIS V |
|
Current: |
Highest Past Year: |
|
XX.INTERPRETIVE SUMMARY: Briefly describe client/member’s global preferences/hopes for recovery, your clinical summary, and recommended treatments/assessments, level of care, duration.
a. Recommended Services: (Check all that apply.) |
□ Family Therapy; □ Individual Therapy; □ Group Therapy; □ Alcohol/Drug Assessment; |
|
Alcohol/ Drug Individual Therapy; |
□ PSR; |
□ CPST; □ Other/Describe: |
b.Other Services/Linkages Needed: □ Vocational Services; □ Social Services; □ Educational Services; □ Medical Services/PCP; □ Self help Groups; □ Other/Describe:
c.Additional Comments:
SIGNATURE
PRINTED NAME OF ASSESSOR
SIGNATURE
LMHP STATUS
DATE
1915(c) IA v.2 (5/7/2014) |
Page 4 of 4 |
Form Data
| Fact Name | Description |
|---|---|
| Form Purpose | The 1915(c) Independent Behavioral Health Assessment form is designed to collect comprehensive demographic, behavioral health history, and social information about a child or youth for the purposes of assessing their behavioral health needs. |
| Demographic Information | Includes basic information such as the child/youth name, assessment date, age, date of birth (DOB), ethnicity, gender, gender expression, and Social Security Number (SSN). |
| Legal Guardian Information | Details about the parent/primary caretaker and legal guardian, including their name, relationship to the child/youth, and contact information. |
| Behavioral Health History | Covers the child/youth's chief complaint, presenting problem/relevant history, past psychiatric/placement history, and a detailed substance use history. |
| Physical Health Information | Includes questions about current medical conditions, medication history, allergies, and the name and contact information of the primary care physician. |
| Social and Legal Status | Explores the child/youth's legal status, family history, trauma history, living situation, educational/employment status, and social history/community integration. |
| Risk Assessment | Assessment of the potential risk to self or others, covering suicidal or homicidal ideation, patterns of risk behavior, and other personal safety risk factors. |
| Cultural and Language Preferences | Information on the child/youth's cultural background, spiritual beliefs, and language preferences to ensure culturally competent care. |
Instructions on Utilizing 1915 C Assessment
The process of completing the 1915(c) Assessment form can be seen as a roadmap to accessing necessary behavioral health services. This comprehensive form captures a wide array of crucial information, ranging from demographic details to a nuanced understanding of the individual's behavioral health history, current status, and future needs. This structured outline ensures a holistic and person-centered approach to identifying and addressing the unique needs of each individual. Following the steps below will guide you through filling out the form efficiently and effectively.
- Start with the Demographic Information section by entering the child or youth's full name, assessment date, age, date of birth (DOB), ethnicity, gender, gender expression, and social security number (SSN). Also, include the parent or primary caretaker's name and contact information. If applicable, note the legal guardian's details and clarify their guardianship status.
- Move to the Behavioral Health History portion.
- For section I, describe the chief complaint as expressed in the words of the client, member, or caretaker.
- In section II, detail the presenting problem or relevant history, including reasons for seeking services and any expectations.
- Provide the current behavioral health provider's name and contact info.
- Section III asks for past psychiatric, placement history, and substance use. Check the applicable boxes and provide details where necessary.
- Under the Physical heading, mark all current medical conditions that apply, including any information on allergies and current or past medications with reasons for prescriptions and responses.
- In the Social section, record legal status, family history, trauma, living situation, educational/employment status, and social history with attention to community integration.
- For the Current Status area, you'll assess the individual through observations and checklists related to general appearance, behavior, psychomotor activity, attitude, speech, mood, affect, and other mental status examination details.
- Complete the Risk Assessment, evaluating potential risks to self or others, and identifying any safety or risk factors present.
- Address Cultural and Language Preferences, ensuring the individual's cultural beliefs, spiritual preferences, and language needs are noted for a person-centered care plan.
- In the Interpretive Summary section, offer a comprehensive clinical summary and outline recommended treatments, required services, and additional comments for a treatment plan that aligns with the client or member's recovery goals and preferences.
- Conclude by providing the Signature of the assessor, along with their printed name, LMHP (Licensed Mental Health Professional) status, and the date of assessment.
Following these steps with attention to detail and empathy will ensure that the assessment is both thorough and reflective of the individual's needs and circumstances. This approach facilitates a supportive path forward, tailored to fostering recovery and promoting holistic well-being.
Obtain Answers on 1915 C Assessment
What is a 1915(c) Independent Behavioral Health Assessment?
A 1915(c) Independent Behavioral Health Assessment is a comprehensive evaluation designed to gather detailed information about a child or youth's behavioral health history, current status, and needs. The form covers a wide range of areas including demographic information, behavioral health and substance use history, physical health, legal status, family history, trauma history, living situation, education and employment status, social history, and mental status examination. This assessment aids in identifying an individual’s needs for treatment and support services.
Who should complete the 1915(c) assessment form?
This form should be completed by a licensed mental health professional (LMHP) who is conducting an assessment of the client/member. The professional gathers information through interviews with the client/member and, if applicable, the parent or primary caretaker, as well as through review of relevant records and documentation.
What purpose does the 1915(c) assessment serve?
The primary purpose of the 1915(c) assessment is to provide a structured and thorough review of an individual's behavioral health needs to inform a treatment and support plan. It identifies areas where the client/member may need support, including mental health services, substance use treatment, medical care, educational or vocational assistance, and social or recreational support. The assessment also helps in identifying risks and designing a safety plan if needed.
How is substance use history evaluated in the assessment?
Substance use history is evaluated through a detailed section within the form where the individual's use of primary, secondary, and tertiary substances is documented, including type, frequency, method of administration, and age of first use. The assessment also inquires about any history of substance use treatment, overdose, withdrawal, and the presence of problems related to substance use, offering a holistic view of the individual’s substance-related challenges.
What information is gathered about the individual's family history and living situation?
The assessment collects comprehensive data regarding the client’s family history, including relationships with relatives, family involvement in treatment, living status of significant relatives, and any adverse circumstances in the family of origin like poverty, criminal behavior, or substance use. The living situation section covers the client’s current residence, how long they have been living there, and the composition of the household, providing insights into the environmental and relational context of the individual's life.
How does the assessment address the client/member's educational and employment status?
The form includes sections that explore the client's current educational placement or employer, highest grade completed or degree obtained, difficulties with reading and writing, and an estimated literacy level. It also seeks to summarize the individual’s educational history, status, and any employment-related information, which can play a crucial role in understanding their social integration and functional status.
What does the mental status examination include?
The mental status examination is a detailed evaluation of the client's current mental functioning. It includes observations and assessments of general appearance, behavior and psychomotor activity, attitude, speech, mood, affect, perceptual disturbances, thought process and content, as well as suicidal or homicidal ideation. This examination provides valuable information on the individual's psychological state and helps in identifying areas that require intervention.
How is the assessment used to develop a treatment plan?
Based on the comprehensive information gathered through the 1915(c) assessment, mental health professionals can design a personalized treatment plan that addresses the specific needs of the child or youth. This plan may recommend various services such as family, individual, or group therapy, substance use assessment, psychosocial rehabilitation services, and links to vocational, educational, social, or medical services. The assessment's findings enable professionals to prioritize interventions and support the client/member in their recovery journey.
Common mistakes
Filling out the 1915(c) Independent Behavioral Health Assessment form requires attention to detail and careful consideration. Below are seven common mistakes that people often make when completing this form:
- Overlooking Demographic Details: Each section under Demographic Information holds crucial relevance. Failing to accurately complete details such as the Child/Youth Name, DOB (Date of Birth), Ethnicity, Gender, and Gender Expression can lead to discrepancies in identifying the beneficiary and affect the accuracy of the assessment.
- Incomplete Behavioral Health History: The Behavioral Health History section is essentially the backbone of the assessment. Skipping details about the Chief Complaint, Presenting Problem/Relevant History, and Past Psychiatric/Placement History can result in an incomplete evaluation of the individual's needs.
- Skimming Over Substance Use History: The Substance Use History provides insights into the individual's past and current substance use that hugely impacts the overall behavioral health assessment. Neglecting to check applicable boxes or provide detailed information can omit critical context for the assessment.
- Ignoring Physical Health Conditions: Physical health conditions can significantly affect an individual's behavioral health. Neglecting to accurately report Current Medical Conditions can lead to missed connections between physical and behavioral health issues.
- Misreporting Educational/Employment Status: The section concerning Educational and Employment Status gives valuable context about the individual's daily life and challenges. Overlooking or misrepresenting this information can mislead those planning the beneficiary's care and support.
- Omission of Legal and Social History: Legal Status and Social History and Community Integration sections are critical for understanding the individual in a broader social and legal context. Failing to accurately report past and current legal statuses, family history, or level of community integration can disrupt the formulation of an adequate care plan.
- Underestimating Risk Assessment: Possibly one of the most crucial sections, the Risk Assessment determines the immediate safety needs of the individual. Not judiciously assessing or reporting potential risks of harm to self or others, including suicidal or homicidal ideations, can have serious, immediate consequences.
It's vital for everyone involved in completing the 1915(c) form to approach it with diligence and a comprehensive understanding of the individual's current and past circumstances. Accurate and thorough information ensures the assessment leads to appropriate and effective support services.
Documents used along the form
Completing the 1915(c) Independent Behavioral Health Assessment is a crucial step in ensuring individuals receive the comprehensive care they need. However, to create a full picture of a person's needs and to facilitate appropriate care planning, this form is often used alongside other key documents. Each of these documents plays a vital role in collecting diverse information that contributes to a well-rounded assessment and care approach.
- Individualized Service Plan (ISP): This detailed plan outlines the specific services, supports, and resources required to meet the unique needs of the individual, as identified through the 1915(c) assessment and other evaluations.
- Medical History Form: Provides comprehensive details about the individual's past and current health conditions, surgeries, hospitalizations, allergies, and ongoing treatments.
- Consent Forms: Essential for legal compliance, these forms document the individual's or guardian's consent for assessment, sharing of information, and implementation of recommended services.
- Behavioral Support Plan: Developed for individuals with challenging behaviors, this plan outlines strategies and interventions aimed at promoting positive behaviors while addressing and minimizing harmful or disruptive behaviors.
- Emergency Contact Information: A simple yet critical form that lists contacts to be reached in case of an emergency, ensuring quick response and conveying crucial information to responders.
- Risk Assessment Form: Identifies potential risks to the individual or others, including self-harm, elopement, aggression, and other behaviors that may require special considerations or interventions.
- Mental Health Advance Directive: A document completed by the individual, detailing their preferences for mental health treatment and interventions, to be referred to if they are unable to make decisions in the future.
- Medication List: An up-to-date record of all medications the individual is taking, including dosages and frequency, critical for avoiding harmful interactions and duplications.
- Release of Information (ROI) Forms: These forms authorize healthcare providers to share the individual's health and treatment information with other necessary parties, facilitating coordinated care and support.
These documents, when used collectively with the 1915(c) Independent Behavioral Health Assessment, allow for a thorough understanding of the individual's current situation, history, and needs. This suite of documentation supports a holistic approach to care planning and ensures that individuals receive targeted, effective, and respectful support on their path to recovery and wellbeing.
Similar forms
The 1915(c) Independent Behavioral Health Assessment form closely resembles a Comprehensive Medical History Form used by healthcare providers. Both gather detailed patient information, including demographic data, medical conditions, medications, and allergies, to ensure a holistic view of the patient's health and needs.
Similar to a Psychosocial Assessment Form, this document collects extensive behavioral health history, family history, and social information, aiming to understand the individual's mental health, interpersonal relationships, and community integration.
It is akin to a Substance Use Disorder Assessment Form due to its detailed substance use history section, including type, frequency, method, and age of first use, which is crucial for diagnosing and planning treatment for substance-related disorders.
The form mirrors a Risk Assessment Tool in its evaluation of the client's potential risk of harm to self or others, assessing factors like suicide risk, history of violence, and substance abuse, to identify safety measures and prevent harm.
Resembling a Mental Status Examination (MSE) Form, it includes an assessment of general appearance, behavior, mood, thought processes, and cognition, which are essential elements in comprehensively evaluating a client's current mental state.
Like an Educational and Employment History Form, it gathers data on the client's educational background and employment status, which are important for understanding the client's daily functioning and potential areas of support.
It functions similarly to a Cultural and Language Preference Assessment, by recognizing the importance of language, customs, spiritual beliefs, and cultural preferences in tailoring healthcare services to meet the client's unique needs and ensure cultural competence in care delivery.
Finally, this form is comparative to a Treatment Planning Tool utilized in behavioral health settings. It concludes with an interpretive summary and recommendations for treatment and assessments, specifying services needed like therapy, social services, or medical linkage, facilitating a client-centered approach to recovery.
Dos and Don'ts
When completing the 1915(c) Independent Behavioral Health Assessment form, it's important to approach this task with care and attention to detail. The following suggestions aim to provide guidance on how to fill out the form accurately and effectively.
Do:Ensure all information is complete and accurate, especially personal details like names, date of birth, and contact information. Missing or incorrect information can delay processing.
Provide detailed behavioral health history, including any past psychiatric diagnoses, treatments, and outcomes. Clarity and detail will help in making an accurate assessment.
List all current and past medications, including over-the-counter drugs, to avoid any potential drug interactions or misunderstandings regarding the patient's medical history.
Be honest about substance use, including the type, frequency, and onset of use. This information is crucial for developing an appropriate treatment plan.
Describe any legal statuses clearly, including any past or current legal issues or charges. This can impact the type of services and support available.
Accurately document the client's or member's current living situation, educational or employment status, and social history to aid in a comprehensive care approach.
Provide a thorough mental status examination and risk assessment. This includes observations of behavior, mood, thought processes, and potential risks to themselves or others.
Reflect the client’s or member's cultural and language preferences to ensure that services are provided in a culturally appropriate manner.
Sign and date the form. The signature of the assessor confirms the authenticity and accuracy of the information provided.
Leave sections blank unless they are truly not applicable. If a section does not apply, it's better to mark it as such (e.g., "N/A") rather than leaving it blank.
Forget to review the form for errors. Even small mistakes can create significant misunderstandings or delays in getting support.
Use technical jargon or acronyms without explanations. Assume the reader may not have a medical or psychological background.
Overlap information in different sections. Each section of the form serves a distinct purpose, and duplicating information can create confusion.
Underestimate the importance of providing a detailed account of the individual’s history and current situation. This assessment is foundational to their care plan.
Ignore or downplay the importance of listing current and past medications and allergies. This is critical for the safety of the individual.
Miss documenting any legal, educational, or social issues the individual is facing, as they are integral to understanding the full context of the individual’s needs.
Withhold information due to concerns about stigma or judgement. The assessment is a confidential document meant to assist in care.
Forget to list emergency contacts or other critical information that could be necessary in creating an effective and comprehensive care plan.
Misconceptions
There are several misconceptions about the 1915(c) Assessment form that need clarification to ensure understanding and proper use:
- It's only for mental health professionals. While the form is comprehensive and covers a wide range of behavioral health information, it is designed for use by a variety of professionals involved in the care of the individual, not solely mental health specialists. Its purpose is to provide a holistic view of the individual's needs.
- The form is only for assessing children and youth. Although the form includes sections specifically related to minors, such as family and educational status, it is also applicable to adults, particularly in sections regarding substance use, legal status, and risk assessment, reflecting its broad application across different age groups.
- It includes a diagnosis. The form provides a detailed framework for gathering information but does not itself provide a diagnosis. Diagnosis occurs after a thorough review of the completed assessment by a qualified health professional, who uses the collected data alongside clinical judgment and diagnostic criteria.
- Privacy is a concern due to detailed personal information. While the form requests detailed personal and medical information, its use complies with health information privacy regulations. The confidentiality of the person being assessed is protected, underscoring the form's adherence to privacy standards.
- It's a one-time assessment tool. The 1915(c) Assessment form is not intended for single use. Re-assessments are necessary to capture changes in the individual's condition, needs, and circumstances over time. These periodic evaluations help ensure that care plans remain relevant and effective.
Correcting these misconceptions fosters a clearer understanding of the 1915(c) Assessment form's purpose, scope, and procedures. This ensures that it is used effectively and appropriately, benefiting both professionals in their practice and individuals in receiving comprehensive care tailored to their needs.
Key takeaways
Understanding the 1915(c) Independent Behavioral Health Assessment form is essential for accurately capturing a client's or member's behavioral health needs and ensuring they receive appropriate care and services. Here are some key takeaways:
A thorough demographic section is the foundation. It includes basic information such as the child or youth's name, date of birth, gender, and legal guardian details. This ensures the individual is correctly identified and that services can be appropriately coordinated.
Behavioral health history is crucial for understanding the individual's needs. Documenting the chief complaint, presenting problems, and relevant history paints a picture of why services are sought, any precipitating factors, symptoms, and the impact on the individual's behavior and functioning.
A comprehensive review of substance use history is necessary. Understanding past and current substance use—including types, frequency, and methods of use—helps in assessing the need for specific interventions or treatment.
Details about current medical conditions and medication help evaluate the individual's overall health and how it may interact with their behavioral health needs.
Social and legal history provide context about the individual's environment, which can significantly impact their behavior and treatment needs.
The assessment of current functioning across various domains—such as living situation, education, employment status, and social history—is integral to planning and delivering effective services.
Mental status examination and risk assessment sections offer insights into the individual's psychological state and potential risks, guiding the urgency and type of interventions required.
Identifying cultural, spiritual, and language preferences tailors services to be respectful and responsive to the individual's background, promoting better engagement and outcomes.
In completing the 1915(c) Assessment form, it is vital to be as detailed and specific as possible, providing a comprehensive view of the individual's needs, preferences, and circumstances. This ensures that they receive the most appropriate and effective support available.
Popular PDF Forms
Printable Nfpa 25 Nfpa Fire Sprinkler Inspection Forms - Allows for specifying other types of battery backup systems, ensuring flexibility in accommodating various fire alarm setups.
Golds Gy - Acknowledge and comply with Gold's Gym Rules and Regulations for a safe and enjoyable fitness environment for everyone.