Blank Aetna International Claim PDF Template
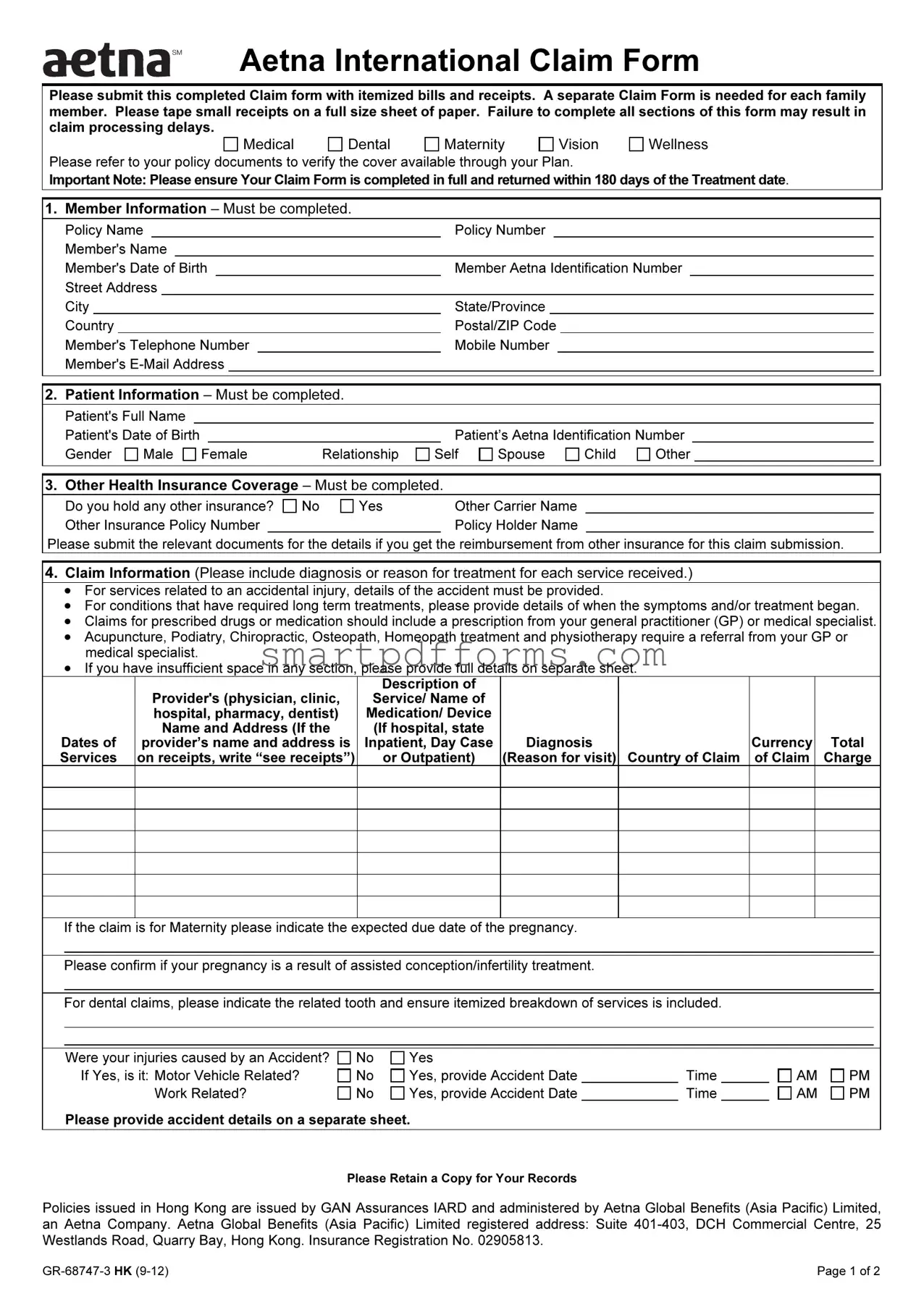
Submitting a claim with Aetna International necessitates a comprehensive understanding of the Aetna International Claim Form, designed to streamline the reimbursement process for medical, dental, maternity, vision, and wellness services. Clients are required to meticulously fill out the form, ensuring that separate forms are utilized for each family member and that all necessary documentation, such as itemized bills and receipts, is attached. A key instruction is the adherence to the 180-day submission deadline post-treatment, emphasizing the necessity of timely action to avoid delays. The claim form is divided into sections that gather member and patient information, details on other health insurance coverage, and specific claim information including diagnoses, reasons for treatment, and details regarding any accidents involved. It allows for the indication of preferred payment methods and currencies for reimbursements, making it essential for members to provide accurate and complete bank details when opting for bank transfer options. Additionally, declarations signed by the claimant affirm the truthfulness of the provided information and consent to Aetna’s use of this data in the claim process. The form’s completion and submission methods underscore Aetna’s flexibility in accommodating clients’ preferences, offering several avenues for claim submission, including postal, online, fax, and email, thus ensuring that the process is as convenient as possible for its members. However, it’s crucial to understand that the form’s issuance doesn't imply an admission of liability by Aetna International, and incomplete submissions may lead to delays in processing, emphasizing the importance of a thorough and accurate completion of all sections of the form.
Preview - Aetna International Claim Form
Aetna International Claim Form
Please submit this completed Claim form with itemized bills and receipts. A separate Claim Form is needed for each family member. Please tape small receipts on a full size sheet of paper. Failure to complete all sections of this form may result in claim processing delays.
Medical
Dental
Maternity
Vision
Wellness
Please refer to your policy documents to verify the cover available through your Plan.
Important Note: Please ensure Your Claim Form is completed in full and returned within 180 days of the Treatment date.
1. Member Information – Must be completed.
Policy Name |
|
Policy Number |
|
||||||||
Member's Name |
|
|
|
|
|
||||||
Member's Date of Birth |
|
Member Aetna Identification Number |
|
|
|||||||
Street Address |
|
|
|
|
|
||||||
City |
|
State/Province |
|
||||||||
Country |
|
Postal/ZIP Code |
|
||||||||
Member's Telephone Number |
|
Mobile Number |
|
|
|||||||
Member's |
|
|
|
|
|||||||
|
|
|
|
|
|||||||
|
|
|
|
|
|||||||
2. Patient Information – Must be completed. |
|
|
|
|
|||||||
Patient's Full Name |
|
|
|
Patient's Date of Birth |
|
|
|
Gender |
Male |
Female |
Relationship |
Patient’s Aetna Identification Number
Self |
Spouse |
Child |
Other |
3. Other Health Insurance Coverage – Must be completed.
Do you hold any other insurance? |
No |
Yes |
Other Carrier Name |
|
Other Insurance Policy Number |
|
|
|
Policy Holder Name |
Please submit the relevant documents for the details if you get the reimbursement from other insurance for this claim submission.
4.Claim Information (Please include diagnosis or reason for treatment for each service received.)
•For services related to an accidental injury, details of the accident must be provided.
•For conditions that have required long term treatments, please provide details of when the symptoms and/or treatment began.
•Claims for prescribed drugs or medication should include a prescription from your general practitioner (GP) or medical specialist.
•Acupuncture, Podiatry, Chiropractic, Osteopath, Homeopath treatment and physiotherapy require a referral from your GP or medical specialist.
•If you have insufficient space in any section, please provide full details on separate sheet.
|
|
Description of |
|
|
|
|
|
Provider's (physician, clinic, |
Service/ Name of |
|
|
|
|
|
hospital, pharmacy, dentist) |
Medication/ Device |
|
|
|
|
|
Name and Address (If the |
(If hospital, state |
|
|
|
|
Dates of |
provider’s name and address is |
Inpatient, Day Case |
Diagnosis |
|
Currency |
Total |
Services |
on receipts, write “see receipts”) |
or Outpatient) |
(Reason for visit) |
Country of Claim |
of Claim |
Charge |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
If the claim is for Maternity please indicate the expected due date of the pregnancy.
Please confirm if your pregnancy is a result of assisted conception/infertility treatment.
For dental claims, please indicate the related tooth and ensure itemized breakdown of services is included.
Were your injuries caused by an Accident? |
No |
Yes |
|
|
If Yes, is it: Motor Vehicle Related? |
No |
Yes, provide Accident Date |
|
Time |
Work Related? |
No |
Yes, provide Accident Date |
|
Time |
Please provide accident details on a separate sheet.
AM AM
PM PM
Please Retain a Copy for Your Records
Policies issued in Hong Kong are issued by GAN Assurances IARD and administered by Aetna Global Benefits (Asia Pacific) Limited, an Aetna Company. Aetna Global Benefits (Asia Pacific) Limited registered address: Suite
Page 1 of 2 |
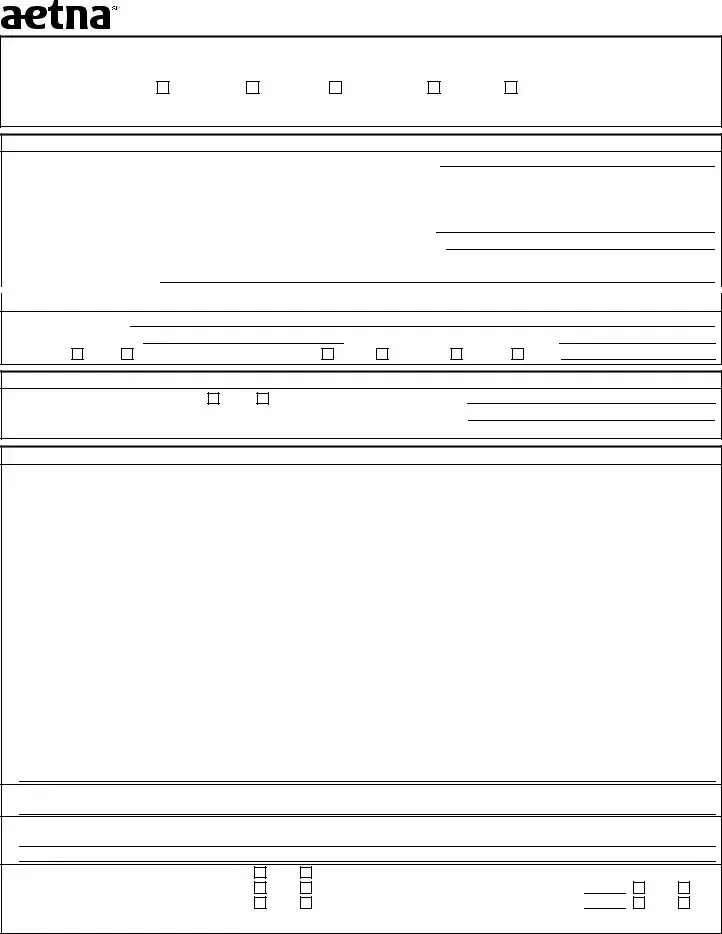
Member’s Name (For faxing purpose):
5. Summary of Payment Details – Must be completed.
Recurring Reimbursement Election – Please check one of the following options if you want to:
Receive future payments using the details provided below
Use the payment information provided below for this claim only
Use the payment details that we already have on file for you
Payment Information
|
Please select your preferred reimbursement method: |
Bank Transfer |
Cheque |
|
|
|
|
|||||||||
|
(If no selection is made, the default method is cheque issued in the member’s name.) |
|
|
|
|
|||||||||||
|
Please indicate your preferred payment currency (If none is indicated, the default currency is US Dollar.) |
|
|
|
||||||||||||
|
Payee Name |
|
|
|
|
Specify if: |
Member |
Provider |
Employer |
|
||||||
|
Claim Settlement Address (if different to Section 1): |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Street |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
City |
|
|
State/Province |
Country |
|
|
|
||||||||
|
If you have selected Bank Transfer as your preferred payment method, the following information is required: |
|
|
|||||||||||||
|
Bank Account Holder Name (as per Bank Statement) |
|
|
|
|
|
|
|
|
|
|
|
||||
|
Bank Account Number |
|
|
|
Sort Code/Branch Code |
|
|
|
|
|
||||||
|
IBAN Code* |
|
|
|
Swift/BIC Code |
|
|
|
|
|
||||||
|
IFSC/ABA/ US Routing Code |
|
|
|
|
|
|
|
|
|
|
|
||||
|
Bank Name |
|
|
|
|
|
|
|
|
|
|
|
|
|||
Bank Address (include Country)
Bank Telephone Number (include Country Code)
*The IBAN is mandatory for bank transfer claim payment transactions in certain countries, such as the United Arab Emirates (UAE). This must be supplied if you are using a bank account in one of these countries. Members should check with their bank to confirm any IBAN requirements.
The most efficient method of receiving your benefits reimbursement is via Bank Transfer. Please check with your bank for help with providing the appropriate instructions to Aetna International.
6.Declaration – Must be completed.
I declare that, to the best of my knowledge, all the information provided on this claim form is truthful and correct. I understand that Aetna will rely on the information provided as such. I agree and accept that this declaration gives Aetna, and its appointed representatives, the right to request past, present, and future medical information in relation to this claim, or any other claim related to the member/covered individual, from any third party, including providers and medical practitioners. I declare and agree
that personal information may be collected, held, disclosed, or transferred (worldwide) to any organization within the Aetna group, its suppliers, providers and any affiliates.
Patient's Signature |
|
Date |
(If patient is under 18 years of age, Parent or Guardian must sign.) |
|
|
Important Note: Please ensure Your Claim Form is completed in full and returned within six months (180 days) of the Treatment date. Failure to complete your form in full will result in the form being returned to you and will delay the processing of your claim. Please note Aetna International is not responsible for any costs associated with the completion of this form or for any further information/ document requested by Us to assess Your claim. The issuing of this Claim Form is in no way an admission of liability.
Please refer to your Member Handbook under General Claims Information for
7. Additional Information
How to submit a Claim
Aetna International provides alternative methods of submitting a claim form to make it easier for our members, below are the listed options:
• Postal Submission |
• Online Claim Submission for our members via our |
Aetna Global Benefits (Asia Pacific) Limited |
secure portal |
Suite |
www.AetnaInternational.com |
DCH Commercial Centre |
• Submit your claim via Fax attaching receipts and |
25 Westlands Road |
referrals from your Medical Practitioner |
Quarry Bay |
|
Hong Kong |
• Email Submission with copies of your receipts and |
|
referrals from your Medical Practitioner |
|
AsiaPacServices@aetna.com |
|
• For claim related queries please contact our 24 hour |
|
Member Services helpline |
|
Please Retain a Copy for Your Records
Policies issued in Hong Kong are issued by GAN Assurances IARD and administered by Aetna Global Benefits (Asia Pacific) Limited, an Aetna Company. Aetna Global Benefits (Asia Pacific) Limited registered address: Suite
Page 2 of 2 |
Form Data
| Fact Name | Description |
|---|---|
| Submission Requirement | Completed claim form must be submitted with itemized bills and receipts within 180 days of the treatment date. |
| Form Completeness | Failure to complete all sections may result in claim processing delays. |
| Separate Forms for Family Members | A separate Claim Form is required for each family member. |
| Specification for Small Receipts | Small receipts should be taped on a full-size sheet of paper. |
| Claim Types Covered | Medical, Dental, Maternity, Vision, and Wellness claims are supported. |
| Governing Law for Policies Issued in Hong Kong | Issued by GAN Assurances IARD and administered by Aetna Global Benefits (Asia Pacific) Limited, governed by Hong Kong law. |
| Alternative Submission Methods | Claims can be submitted via postal mail, online, fax, or email to Aetna International. |
Instructions on Utilizing Aetna International Claim
Filling out the Aetna International Claim Form is an essential step in ensuring you are reimbursed for medical, dental, maternity, vision, and wellness services under your plan. Timely submission of a properly completed form, alongside all necessary documentation like itemized bills and receipts, is crucial to avoid any delays in the processing of your claim. Remember, a separate form is required for each family member, and be aware that adhering to the submission deadline of 180 days from the treatment date is key. Follow these outlined steps to complete your claim form accurately.
- Member Information: Fill in the policy name, policy number, member's name, date of birth, Aetna identification number, complete address, telephone number, mobile number, and email address.
- Patient Information: Provide the patient’s full name, date of birth, gender, relationship to the member, and the patient's Aetna identification number.
- Other Health Insurance Coverage: Indicate whether the patient holds any other insurance. If yes, include the other carrier's name, policy number, and policyholder's name. Attach documents for other insurance reimbursements related to this claim.
- Claim Information: Include diagnosis or reason for treatment for each service received, details of any accidental injuries, long-term treatment commencements, prescriptions for medication, and referrals for specific treatments like acupuncture or physiotherapy. Use an additional sheet if necessary.
- For maternity claims, note the expected due date and whether the pregnancy is a result of assisted conception. For dental claims, detail the related tooth and provide an itemized breakdown.
- Indicate whether injuries were accident-related, and if so, whether it was motor vehicle or work-related, providing dates and times. Attach a separate sheet for accident details.
- Summary of Payment Details: Choose your recurring reimbursement election and preferred reimbursement method (bank transfer or cheque). Select your preferred payment currency, providing detailed bank information if you opt for bank transfer.
- Declaration: Sign the form to declare that all information provided is truthful and correct. If the patient is under 18 years old, a parent or guardian must sign instead.
Once the form is complete, retain a copy for your records. Submission can be made through postal service, online via the Aetna Global Benefits secure portal, fax, or email, including all necessary documentation as instructed. Following these detailed steps helps ensure that your claim is processed efficiently and accurately.
Obtain Answers on Aetna International Claim
FAQs about the Aetna International Claim Form
Do I need to fill out a separate claim form for each family member?
Yes, a separate claim form is required for each family member to ensure that claims are processed accurately and efficiently. This helps in keeping the records organized and speeds up the claim processing time.
What documents are required to submit along with the claim form?
When submitting the claim form, you must include itemized bills and receipts for the claimed services. For smaller receipts, it's advised to tape them onto a full-size sheet of paper for better visibility. Incomplete submissions may cause delays in processing your claim.
For which types of coverage can I use the claim form?
The form covers a variety of claims, including Medical, Dental, Maternity, Vision, and Wellness. Always refer to your policy documents to confirm the coverage available through your plan.
How long do I have to submit the claim form after treatment?
The claim form should be completed in full and returned within 180 days of the treatment date. Submitting your claim within this timeframe ensures your request is considered without unnecessary delays.
What if I hold another insurance policy?
If you have other health insurance coverage, it's important to indicate this on the form and provide the relevant documents. This information helps Aetna process your claim efficiently, especially if you're seeking reimbursement from another insurance provider as well.
Is there a specific section for claims related to accidents?
Yes, if your claim is related to an accidental injury, you need to provide detailed information about the accident. This includes whether the injury was motor or work-related and requires attaching any additional sheets if necessary for a comprehensive account.
How should claims for prescribed drugs or specialist treatments like acupuncture or chiropractic be handled?
For prescribed drugs and specific treatments such as acupuncture or chiropractic, it's necessary to include a prescription or referral from your general practitioner (GP) or medical specialist. This documentation is essential for the claim to be processed.
What are the payment options for reimbursements?
You can choose between receiving payments via bank transfer or check. If you prefer a bank transfer, ensure to provide all required banking details. If no preference is indicated, the default payment method is a check issued in the member's name.
How can I submit my completed claim form?
Aetna International offers multiple submission methods for your convenience, including postal submission, online via secure portal, fax, and email. Choose the method that best suits your needs for efficient claim processing.
What if I need assistance or have questions about my claim?
For any claim-related queries or if you need assistance in filling out your form, you can contact Aetna's 24-hour Member Services helpline. Their trained staff can provide the support and guidance you need.
Common mistakes
Not submitting a separate form for each family member is a common mistake. The instructions clearly state that a distinct Claim Form is necessary for every individual in the family seeking reimbursement. This ensures that each claim is processed accurately and without confusion.
Failing to include itemized bills and receipts with the claim form is another error. The instructions emphasize the importance of submitting these documents alongside the completed form. This documentation is crucial for validating the services received and the amounts to be reimbursed. It's also advised to tape small receipts on a full-size sheet of paper for better organization and legibility.
Leaving sections of the form incomplete can significantly delay the claim process. Every section of the form collects essential information needed to process the claim successfully. Missing details can lead to a request for additional information or even result in the form being returned, which delays processing times.
Ignoring the submission deadline is a critical oversight. The form must be returned within 180 days of the treatment date. Overlooking this timeline could result in the claim being denied. This strict timeframe underscores the importance of organizing and submitting healthcare documents promptly.
Documents used along the form
When submitting an Aetna International Claim Form, it's crucial to include specific forms and documents to ensure that your claim is processed efficiently and without delay. These documents provide detailed information required for the evaluation and reimbursement of your medical expenses. Below is a list of documents often used along with the Aetna International Claim form, which are pivotal in the claim submission process.
- Itemized Bills: These are detailed invoices from the healthcare provider that include each service provided, the cost of each service, and the total amount charged. They should show the patient's name, the date of service, and the healthcare provider's information.
- Receipts for Payments: Original or certified copies of receipts for payments made for medical services, devices, or prescriptions are needed. These are used to prove that the expenses claimed were paid by the claimant.
- Prescriptions: For claims related to prescribed drugs or medication, a copy of the original prescription from the general practitioner (GP) or medical specialist is required. This shows the medication was necessary and prescribed by a licensed medical professional.
- Referral Letters: For treatments such as acupuncture, chiropractic, osteopathy, homeopathy, and physiotherapy, a referral from a GP or medical specialist is often necessary to demonstrate the need for these specialized services.
- Accident Reports: If the claim involves treatment for injuries related to an accident, a detailed accident report must be included. This may include a police report or an employer’s report if it’s work-related, providing context and details about the incident.
- Medical Reports or Diagnostic Results: For conditions requiring long-term treatments, or for services leading to hospital admission, relevant medical reports or diagnostic results supporting the diagnosis and necessity of treatment should be submitted. These documents provide detailed medical justifications for the services received.
Include these documents carefully with your Aetna International Claim Form to facilitate a smooth processing experience. It's essential to check that each record is clear, accurate, and complete to prevent any delays or issues in the claim processing. Always retain copies for your records before submitting any original documents. Remember, these materials serve as evidence of the medical necessity and expenses incurred, which are vital for a successful claim reimbursement.
Similar forms
The Blue Cross Blue Shield International Claim Form shares similarities with the Aetna form in requiring detailed member and patient information, including policy numbers, names, dates of birth, and other health insurance coverage. Both forms also necessitate specifics about the treatment or service provided, diagnosis, and a breakdown of charges. Additionally, both insist on completing a declaration by the claimant affirming the truthfulness of the information provided.
The Cigna Global Health Claim Form is similar as it requires comprehensive member and patient information, specifics about the medical treatment or service received, and a detailed cost breakdown. Like Aetna's form, it requests information on any other health insurance coverage and requires the claimant's signature on a declaration asserting the accuracy of the provided information.
The UnitedHealthcare Global Claim Form closely matches the Aetna claim form by asking for thorough member and patient data, details of the claim including dates of service, diagnosis, and treatment information. It too mandates information on other health insurance coverages and involves a declaration section where the claimant must confirm the correctness and completeness of the information submitted.
The Allianz Worldwide Care Claim Form mirrors the Aetna form by necessitating detailed member/patient information, comprehensive claim information including diagnosis, treatment specifics, and a cost breakdown. Both forms include sections for declaring other health insurance coverages and feature a declaration by the claimant to verify the truthfulness and accuracy of all the information provided.
Bupa Global Claim Form is similar in its requirement for extensive member and patient details, in-depth information on the medical services received including provider details, diagnosis and treatment specifics, and a detailed account of expenses. Like Aetna, it also includes a section for the declaration of other health insurance coverages and a claimant's declaration affirming the correctness of the information.
The GeoBlue International Claim Form parallels the Aetna form in its detailed request for member and patient information, including health insurance coverage details, comprehensive service and treatment details along with a breakdown of costs. Additionally, both forms have a declaration section for the claimant to affirm the information's accuracy. Importantly, both emphasize the need for submitting all relevant documentation within a specified timeframe to avoid delays in processing.
Dos and Don'ts
When filling out the Aetna International Claim form, there are several key guidelines to follow to ensure your claim is processed efficiently and effectively. Below, find a list of do's and don'ts that can help guide you through the process.
- Do ensure that the claim form is completed in full. All sections must be filled out to avoid any delays in the claim processing. This includes member information, patient information, other health insurance coverage, claim information, summary of payment details, and the declaration section.
- Do submit the claim form within 180 days of the treatment date. It's crucial to submit your claim in a timely manner to ensure it is considered for reimbursement.
- Do include all itemized bills and receipts along with the claim form. Tape smaller receipts onto a full-size sheet of paper for clarity and ease of review.
- Do retain a copy of the claim form and all documents for your records. Keeping a copy ensures you have the necessary documents on hand should there be any questions or follow-up required.
- Don't forget to sign the declaration section. If the patient is under 18 years of age, a parent or guardian must sign the form. An unsigned claim form can lead to processing delays or outright denial.
- Don't leave sections incomplete. Incomplete forms may be returned to you, causing delays. If you don't have an answer for a section or it doesn't apply to you, mark it as "N/A" or provide a brief explanation.
- Don't assume all treatments are covered. Before submitting a claim, refer to your policy documents to verify the coverage available through your plan. This helps manage expectations and understand your benefits.
- Don't wait to submit your claim. Procrastination can lead to missing the 180-day submission deadline, resulting in a denied claim. Prompt submission ensures your claim is assessed in a timely manner.
Misconceptions
When handling an Aetna International Claim Form, people often have misunderstandings about the process and requirements. It's important to clear up these misconceptions to ensure smooth and timely processing of claims.
Every family member can use the same claim form. This is incorrect. A separate claim form is needed for each family member. This helps Aetna International process each person's claims accurately and efficiently.
Small receipts don’t need to be attached. In reality, all receipts, including small ones, should be attached to a full-size sheet of paper and submitted with the claim form. This ensures that all expenses are accounted for during the claims process.
It’s okay to leave some sections incomplete if they don’t apply. This is a common misconception. All sections of the form must be completed to avoid delays in claim processing. Incomplete forms can result in the claim being returned for additional information.
Claims do not require detailed information such as the diagnosis or reason for treatment. Contrary to this belief, providing a diagnosis or reason for each service received is crucial for Aetna to understand the nature of the treatment and process the claim appropriately.
You can submit the claim form at any time after receiving treatment. Actually, the claim form must be completed in full and returned within 180 days of the treatment date. Submitting the form within this timeframe is essential for the reimbursement process.
Submitting via postal mail is the only option. Aetna International offers multiple submission options, including online submission via their secure portal, fax, and email, in addition to postal submission. This flexibility ensures members can choose the method most convenient for them.
Clearing up these misconceptions can help ensure that your claim is processed smoothly and efficiently, reducing the likelihood of delays and ensuring you receive the reimbursements you are entitled to.
Key takeaways
Filling out the Aetna International Claim Form correctly and comprehensively is pivotal in ensuring timely processing and reimbursement of your claims. Here are key takeaways to assist you:
- Ensure that a separate claim form is filled out for each family member to streamline the processing of multiple claims.
- Attach itemized bills and receipts alongside the completed claim form. For smaller receipts, affix them onto a full-size sheet of paper to prevent them from being misplaced.
- Complete all sections of the form without omission. Incomplete forms may lead to delays in the processing of your claim.
- The form encompasses various types of claims, including medical, dental, maternity, vision, and wellness, making it crucial to indicate the specific type of claim you are submitting.
- Submission of the claim form must occur within 180 days from the date of treatment to be considered for reimbursement.
- For claims involving other health insurance coverage, it is essential to disclose this information and provide relevant documents for a seamless claim experience.
- Include comprehensive details for claim information, such as diagnosis or reason for treatment, especially for long-term treatments or accidental injuries, to support your claim effectively.
- Select your preferred method of reimbursement and ensure the payment details section is thoroughly completed to facilitate a smooth transaction.
- A declaration section must be signed to affirm that the information provided is truthful and accurate, granting Aetna the right to request additional medical information if necessary.
Adhering to these guidelines not only simplifies the claims process but also helps in expediting your reimbursement. Aetna International offers multiple methods to submit your claim, including postal, online, fax, and email submissions, providing flexibility and convenience for their members.
Popular PDF Forms
Are Medicaid and Medical the Same - Asks for information on non-medical individuals who can discuss the applicant's condition.
Bge Pay by Phone - Know the importance of having your building permit details ready when applying for BGE services.
Forwarding Mail - Exception clauses for address changes post-start date manage expectations.