Blank Braden Scale PDF Template
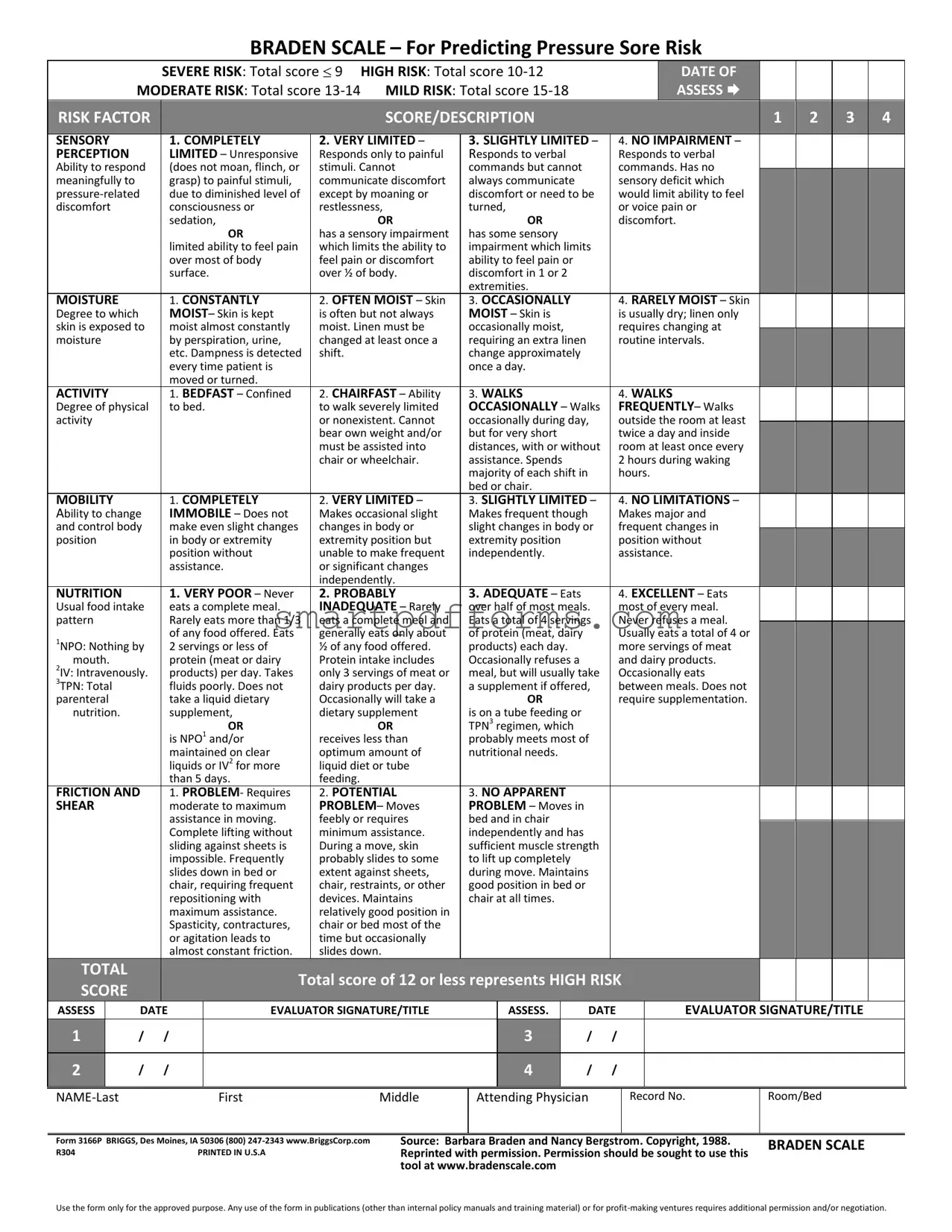
In the realm of patient care and safety, ensuring that individuals who are immobilized or have limited mobility are assessed for the risk of developing pressure ulcers is critical. The Braden Scale form serves as an essential tool for healthcare professionals to evaluate this risk. This comprehensive tool divides risk factors into several categories including sensory perception, moisture, activity, mobility, nutrition, and friction and shear, each scored from 1 (indicating highest risk) to 4 (indicating lowest risk). The total score then places the patient in a risk category ranging from severe to mild. The structured assessment provided by the Braden Scale enables caregivers to identify patients at risk promptly, leading to early intervention strategies. Since its inception by Barbara Braden and Nancy Bergstrom in 1988, the Braden Scale has been widely adopted in healthcare settings, making it a cornerstone for preventive care in the fight against pressure ulcers. Proper usage of the scale not only aligns with best practices in patient care but also necessitates adherence to guidelines regarding its application and any modifications for public or commercial use, ensuring that the tool's integrity and reliability remain intact.
Preview - Braden Scale Form
BRADEN SCALE – For Predicting Pressure Sore Risk
|
SEVERE RISK: Total score 9 |
HIGH RISK: Total score |
DATE OF |
|
MODERATE RISK: Total score |
MILD RISK: Total score |
ASSESS |
|
|
|
|
|
|
|
|
|
RISK FACTOR |
|
|
|
|
|
SCORE/DESCRIPTION |
|
|
|
|
|
|
|
1 |
2 |
3 |
4 |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SENSORY |
|
|
|
1. COMPLETELY |
2. VERY LIMITED – |
3. SLIGHTLY LIMITED – |
|
4. NO IMPAIRMENT – |
|
|
|
|||||||||||
|
|
PERCEPTION |
|
|
|
LIMITED – Unresponsive |
Responds only to painful |
Responds to verbal |
|
|
Responds to verbal |
|
|
|
||||||||||
|
|
Ability to respond |
|
|
(does not moan, flinch, or |
stimuli. Cannot |
commands but cannot |
|
|
commands. Has no |
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
meaningfully to |
|
|
|
grasp) to painful stimuli, |
communicate discomfort |
always communicate |
|
|
sensory deficit which |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
due to diminished level of |
except by moaning or |
discomfort or need to be |
|
would limit ability to feel |
|
|
|
|
||||||||||||
|
|
discomfort |
|
|
|
consciousness or |
restlessness, |
turned, |
|
|
or voice pain or |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
sedation, |
OR |
|
OR |
|
|
discomfort. |
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
OR |
has a sensory impairment |
has some sensory |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
limited ability to feel pain |
which limits the ability to |
impairment which limits |
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
over most of body |
feel pain or discomfort |
ability to feel pain or |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
surface. |
over ½ of body. |
discomfort in 1 or 2 |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
extremities. |
|
|
|
|
|
|
|
|
|
|
|
||
|
|
MOISTURE |
|
|
|
1. CONSTANTLY |
2. OFTEN MOIST – Skin |
3. OCCASIONALLY |
|
|
4. RARELY MOIST – Skin |
|
|
|
||||||||||
|
|
Degree to which |
|
|
|
MOIST– Skin is kept |
is often but not always |
MOIST – Skin is |
|
|
is usually dry; linen only |
|
|
|
||||||||||
|
|
skin is exposed to |
|
|
moist almost constantly |
moist. Linen must be |
occasionally moist, |
|
|
requires changing at |
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
moisture |
|
|
|
by perspiration, urine, |
changed at least once a |
requiring an extra linen |
|
|
routine intervals. |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
etc. Dampness is detected |
shift. |
change approximately |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
every time patient is |
|
once a day. |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
moved or turned. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
ACTIVITY |
|
|
|
1. BEDFAST – Confined |
2. CHAIRFAST – Ability |
3. WALKS |
|
|
4. WALKS |
|
|
|
||||||||||
|
|
Degree of physical |
|
|
to bed. |
to walk severely limited |
OCCASIONALLY – Walks |
|
FREQUENTLY– Walks |
|
|
|
||||||||||||
|
|
activity |
|
|
|
|
|
|
or nonexistent. Cannot |
occasionally during day, |
|
outside the room at least |
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
bear own weight and/or |
but for very short |
|
|
twice a day and inside |
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
must be assisted into |
distances, with or without |
|
room at least once every |
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
chair or wheelchair. |
assistance. Spends |
|
|
2 hours during waking |
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
majority of each shift in |
|
hours. |
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
bed or chair. |
|
|
|
|
|
|
|
|
|
|
|
||
|
|
MOBILITY |
|
|
|
1. COMPLETELY |
2. VERY LIMITED – |
3. SLIGHTLY LIMITED – |
|
4. NO LIMITATIONS – |
|
|
|
|||||||||||
|
|
Ability to change |
|
|
IMMOBILE – Does not |
Makes occasional slight |
Makes frequent though |
|
Makes major and |
|
|
|
||||||||||||
|
|
and control body |
|
|
make even slight changes |
changes in body or |
slight changes in body or |
|
frequent changes in |
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
position |
|
|
|
in body or extremity |
extremity position but |
extremity position |
|
|
position without |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
position without |
unable to make frequent |
independently. |
|
|
assistance. |
|
|
|
|
||||||||
|
|
|
|
|
|
|
assistance. |
or significant changes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
independently. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NUTRITION |
|
|
|
1. VERY POOR – Never |
2. PROBABLY |
3. ADEQUATE – Eats |
|
|
4. EXCELLENT – Eats |
|
|
|
||||||||||
|
|
Usual food intake |
|
|
eats a complete meal. |
INADEQUATE – Rarely |
over half of most meals. |
|
most of every meal. |
|
|
|
||||||||||||
|
|
pattern |
|
|
|
Rarely eats more than 1/3 |
eats a complete meal and |
Eats a total of 4 servings |
|
Never refuses a meal. |
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
1NPO: Nothing by |
|
|
of any food offered. Eats |
generally eats only about |
of protein (meat, dairy |
|
|
Usually eats a total of 4 or |
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
2 servings or less of |
½ of any food offered. |
products) each day. |
|
|
more servings of meat |
|
|
|
|
|||||||||||
|
|
mouth. |
|
|
|
protein (meat or dairy |
Protein intake includes |
Occasionally refuses a |
|
|
and dairy products. |
|
|
|
|
|||||||||
|
|
2IV: Intravenously. |
|
|
products) per day. Takes |
only 3 servings of meat or |
meal, but will usually take |
|
Occasionally eats |
|
|
|
|
|||||||||||
|
|
3TPN: Total |
|
|
|
fluids poorly. Does not |
dairy products per day. |
a supplement if offered, |
|
between meals. Does not |
|
|
|
|
||||||||||
|
|
parenteral |
|
|
|
take a liquid dietary |
Occasionally will take a |
|
OR |
|
|
require supplementation. |
|
|
|
|
||||||||
|
|
nutrition. |
|
|
|
supplement, |
dietary supplement |
is on a tube feeding or |
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
OR |
OR |
TPN3 regimen, which |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
is NPO1 and/or |
receives less than |
probably meets most of |
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
maintained on clear |
optimum amount of |
nutritional needs. |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
liquids or IV2 for more |
liquid diet or tube |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
than 5 days. |
feeding. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
FRICTION AND |
|
|
1. PROBLEM- Requires |
2. POTENTIAL |
3. NO APPARENT |
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
SHEAR |
|
|
|
moderate to maximum |
PROBLEM– Moves |
PROBLEM – Moves in |
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
assistance in moving. |
|
feebly or requires |
bed and in chair |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
Complete lifting without |
|
minimum assistance. |
independently and has |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
sliding against sheets is |
|
During a move, skin |
sufficient muscle strength |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
impossible. Frequently |
|
probably slides to some |
to lift up completely |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
slides down in bed or |
|
extent against sheets, |
during move. Maintains |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
chair, requiring frequent |
|
chair, restraints, or other |
good position in bed or |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
repositioning with |
|
devices. Maintains |
chair at all times. |
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
maximum assistance. |
|
relatively good position in |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Spasticity, contractures, |
|
chair or bed most of the |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
or agitation leads to |
|
time but occasionally |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
almost constant friction. |
|
slides down. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TOTAL |
|
|
|
|
Total score of 12 or less represents HIGH RISK |
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
SCORE |
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
ASSESS |
|
DATE |
|
EVALUATOR SIGNATURE/TITLE |
|
ASSESS. |
|
DATE |
|
EVALUATOR SIGNATURE/TITLE |
|
|||||||||||
|
1 |
|
/ |
/ |
|
|
|
|
|
3 |
|
/ |
/ |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
2 |
|
/ |
/ |
|
|
|
|
|
4 |
|
/ |
/ |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
First |
Middle |
Attending Physician
Record No.
Room/Bed
Form 3166P BRIGGS, Des Moines, IA 50306 (800)
R304 |
PRINTED IN U.S.A |
Source: Barbara Braden and Nancy Bergstrom. Copyright, 1988. |
BRADEN SCALE |
Reprinted with permission. Permission should be sought to use this |
|
tool at www.bradenscale.com |
|
Use the form only for the approved purpose. Any use of the form in publications (other than internal policy manuals and training material) or for
Form Data
| Fact | Detail |
|---|---|
| Purpose of the Braden Scale | For Predicting Pressure Sore Risk |
| Risk Levels |
Severe Risk: Total score ≤ 9 High Risk: Total score 10-12 Moderate Risk: Total score 13-14 Mild Risk: Total score 15-18 |
| Risk Factors Assessed | Sensory Perception, Moisture, Activity, Mobility, Nutrition, Friction and Shear |
| Scoring System | Scores range from 1 (least favorable) to 4 (most favorable) for each risk factor |
| Total Score Interpretation | A total score of 12 or less represents high risk for pressure sores |
| Assessment Requirements | Form must be completed by a qualified evaluator |
| Form Identification | Form 3166P by BRIGGS, Des Moines, IA |
| Usage Permission | Permission required for use outside of internal policy manuals and training material. Commercial use requires additional permission. |
| Source | Developed by Barbara Braden and Nancy Bergstrom, 1988 |
Instructions on Utilizing Braden Scale
Filling out the Braden Scale form is an essential step in assessing the risk of pressure sore development in patients. The process involves evaluating multiple risk factors including sensory perception, moisture, activity, mobility, nutrition, friction, and shear. Each category is scored based on the patient's condition, contributing to a total that predicts the severity of risk. Having a structured approach to completing this form ensures a thorough and accurate assessment. Below are the steps needed to correctly fill out the Braden Scale form.
- Start by noting the date of assessment at the top of the form. This is crucial for tracking changes over time.
- Assess Sensory Perception. Determine the patient's ability to respond to pressure-related discomfort. Score from 1 (completely limited) to 4 (no impairment).
- Evaluate the Moisture level. Consider how often the skin is exposed to moisture, which can influence sore risk. Score from 1 (constantly moist) to 4 (rarely moist).
- Consider the patient's Activity level. Assess how much the patient moves, since immobility increases risk. Score from 1 (bedfast) to 4 (walks frequently).
- Determine Mobility. Evaluate the patient's ability to change and control body positions. Score from 1 (completely immobile) to 4 (no limitations).
- Assess Nutrition. Evaluate the patient's usual food intake pattern. Scores range from 1 (very poor) to 4 (excellent).
- Assess Friction and Shear. Consider the degree to which the patient is at risk due to friction and shear. Score from 1 (problem) to 3 (no apparent problem).
- Add up the scores from each section to get the Total Score. Refer to the risk categories at the top of the form to determine the patient's risk level (severe, high, moderate, or mild risk).
- Fill in the assessment date below the Total Score section to complete the risk assessment section.
- Ensure the Evaluator Signature/Title section is signed by the person completing the assessment. This verifies the assessment's authenticity and accuracy.
- Document the patient's details, including their name, attending physician, record number, and room/bed number, at the bottom of the form. This helps in identifying the assessed patient and tracking their progress over time.
Once the Braden Scale form is fully completed, it should be submitted as part of the patient's medical record. This will allow healthcare professionals to develop a care plan that addresses the identified risks. Monitoring and reassessment should be conducted as per the healthcare facility's protocols or whenever the patient's condition changes.
Obtain Answers on Braden Scale
What is the Braden Scale for Predicting Pressure Sore Risk?
The Braden Scale is a tool used by healthcare professionals to evaluate a patient's risk of developing pressure sores. It assesses six areas related to skin integrity and pressure sore risk: sensory perception, moisture, activity, mobility, nutrition, and friction and shear. Each area is scored from 1 to 4, with a lower score indicating greater risk. The total score helps categorize a patient’s risk level as severe (9 or less), high (10-12), moderate (13-14), or mild (15-18).
How often should the Braden Scale be used on patients?
The frequency of Braden Scale assessments can vary based on the patient's condition and the healthcare setting. In general, an initial assessment is recommended upon admission to a healthcare facility to establish baseline risk. Regular reassessments should follow based on the patient's changing condition or as per the facility's policy, often ranging from daily in acute care settings to weekly in long-term care settings.
Who is qualified to perform assessments using the Braden Scale?
Assessments using the Braden Scale should be performed by healthcare professionals who have received training in the use of the tool. This can include nurses, physical therapists, and other skilled nursing staff. Proper training ensures accurate scoring and effective risk assessment, which is crucial for preventing pressure sores.
Can the Braden Scale be used in all healthcare settings?
Yes, the Braden Scale is versatile and can be used across various healthcare settings, including hospitals, long-term care facilities, and in-home care situations. Its purpose is to provide a uniform method of assessing pressure sore risk that can be easily communicated among healthcare professionals, contributing to preventative care plans tailored to the patient’s needs.
Common mistakes
Not accurately assessing the patient's sensory perception capabilities, often due to a lack of thorough evaluation or misunderstanding of the patient's responses to stimuli. This might lead to an incorrect score that either underestimates or overestimates the risk of pressure sore development.
Failing to properly evaluate and record the degree of moisture to which the patient's skin is exposed. This mistake can occur if the assessor does not check the patient's skin frequently enough or fails to account for factors like incontinence or excessive sweating.
Incorrectly gauging the patient's level of activity. Sometimes, assessors might overlook occasional movements or overestimate the patient's ability to move based on optimistic observations, leading to an inaccurate activity score.
Misjudging the patient's mobility. An assessor might not take into account all forms of slight or occasional movements the patient can make, which might result in either an overestimation or underestimation of the mobility score.
Overlooking the patient's nutritional status or not considering the quality and quantity of food intake and the impact of IV fluids or tube feeding, if applicable. This can lead to either a higher or lower nutrition score than appropriate.
Not correctly assessing the patient's risk related to friction and shear. This often happens when there's a failure to observe the patient's movements in bed or chair and the resulting interaction with sheets or other materials.
Errors in totaling scores or misinterpreting the risk category. Sometimes, even when individual scores are accurately recorded, mistakes in addition or misunderstanding the scale can misclassify the patient's risk level.
Neglecting to regularly reassess and update the Braden Scale for a patient whose condition changes. Continuous assessment is vital since a patient's risk factors for pressure sore development can change rapidly.
It is crucial that healthcare providers receive proper training on using the Braden Scale accurately and ensure that assessments are conducted meticulously and reviewed regularly, to significantly improve patient outcomes and prevent pressure sores.
Documents used along the form
When caring for individuals with the potential for developing pressure ulcers, healthcare professionals frequently turn to the Braden Scale for Predicting Pressure Sore Risk. This crucial tool helps in assessing a patient's risk level by evaluating different factors that influence skin integrity. However, the Braden Scale does not exist in isolation. To create a comprehensive care plan, other forms and documentation are often used in conjunction to provide a holistic view of the patient’s health status and specific care needs.
- Nutritional Assessment Forms: Given that nutrition plays a significant role in skin health and recovery, nutritional assessment forms complement the Braden Scale by detailing a patient's dietary intake, preferences, restrictions, and nutritional status. This information is key in determining if dietary modifications or supplementation is needed to support wound healing and prevention.
- Incident Report Forms: When pressure ulcers develop or worsen, incident report forms are filled out. These documents capture the circumstances leading to the incident, current wound status, and immediate actions taken. They serve as a critical communication tool among healthcare providers and as a record for quality improvement efforts.
- Patient Turn Charts: To prevent pressure ulcers, patients at risk need to be repositioned regularly. Patient turn charts are used alongside the Braden Scale to schedule and document repositioning, ensuring that the care team consistently implements preventive measures. This documentation helps in tracking compliance with care protocols and identifying any gaps in care.
- Wound Assessment Tools: For patients with existing pressure ulcers or those at high risk, wound assessment tools are utilized for regular monitoring. These documents record the location, stage, size, appearance, and treatment of wounds over time. They provide a detailed history that is crucial for evaluating treatment effectiveness and making necessary adjustments.
Together with the Braden Scale, these documents create a multi-faceted approach to preventing and managing pressure ulcers. By assessing a wide range of factors—from nutritional status to the necessity of repositioning and the treatment of existing wounds—healthcare teams can offer more targeted and effective care. This not only enhances the quality of life for those at risk but also supports a culture of safety and continuous improvement within healthcare settings.
Similar forms
Norton Scale – Similar to the Braden Scale, the Norton Scale also assesses the risk of pressure ulcers in patients but with a focus on five factors: physical condition, mental state, activity, mobility, and incontinence. Just like the Braden Scale, it categorizes patients into risk levels based on a total score, aiding caregivers in identifying those who need increased preventive measures.
Waterlow Score – This tool is used for assessing the risk of developing a pressure ulcer, taking into account factors such as build/weight for height, visual assessment of the skin, sex/age, and continence. The assessment criteria are broader, but, akin to the Braden Scale, it provides a quantitative score to guide intervention strategies.
Morse Fall Scale – While the Morse Fall Scale focuses on the likelihood of a patient falling rather than developing pressure ulcers, it is similar to the Braden Scale in that it evaluates risk based on multiple weighted factors, including history of falling, secondary diagnoses, use of ambulatory aids, and types of mobility. Both tools are used to enhance patient care through risk assessment.
Malnutrition Universal Screening Tool (MUST) – MUST is employed to screen for malnutrition or the risk of malnutrition in adults. It considers BMI, unintentional weight loss, and effect of acute disease on intake for more than 5 days. Like the Braden Scale, it provides a score that dictates the level of risk and recommends a course of action based on that risk.
Mini Nutritional Assessment (MNA) – The MNA is a detailed nutritional screening and assessment tool that helps identify geriatric patients at risk of malnutrition. While it focuses on nutritional status rather than pressure ulcer risk, it shares the Braden Scale's goal of early identification of individuals who need targeted intervention.
Barthel Index – The Barthel Index measures the performance of activities of daily living (ADLs), providing a score based on the individual's degree of independence in ten areas of daily life. Similar to the Braden Scale, this scoring helps in planning care by identifying areas where the patient needs assistance or intervention.
Glasgow Coma Scale – This scale is used to assess the consciousness level of patients after a head injury but shares the concept of using a scoring system with the Braden Scale. The Glasgow Coma Scale scores eye, verbal, and motor responses, which then inform medical professionals about the patient’s condition and prognosis similarly to how the Braden Scale informs about ulcer risk.
Functional Independence Measure (FIM) – The FIM scores an individual's level of disability based on how independently they can perform a set of 18 ADLs. Its purpose is akin to the Braden Scale in that both are used to evaluate a patient's condition to aid in creating a care plan that addresses their specific needs.
Spinal Cord Injury Pressure Ulcer Scale (SCIPUS) – Specifically designed for individuals with spinal cord injury, SCIPUS assesses risk factors associated with pressure ulcer development in this population. Like the Braden Scale, it recognizes the importance of early risk identification to prevent the occurrence of pressure ulcers.
Dos and Don'ts
When utilizing the Braden Scale for Predicting Pressure Sore Risk, accuracy and attentiveness are paramount. Below are essential dos and don'ts to ensure the form is completed effectively and accurately. Understanding these guidelines can significantly impact the predictive quality of the assessment, thereby influencing the care and preventative strategies deployed for those at risk of pressure sores.
- Do ensure that all sections of the form are completed thoroughly. The Braden Scale is comprehensive, designed to cover various factors that contribute to pressure sore risk. Incompletely filled sections can skew the risk assessment, potentially jeopardizing patient care.
- Don't rush through the assessment. Each category requires a thoughtful evaluation of the patient's current condition. Speeding through the form without proper consideration can lead to inaccuracies and misrepresentations of the patient's true risk level.
- Do familiarize yourself with the scoring system before beginning the assessment. Understanding the significance of each score within the context of the Braden Scale allows for a more accurate reflection of the patient's condition and risks.
- Don't assume without verifying. For instance, when assessing nutrition or mobility, direct observation or consultation with caregiving staff can provide insight into usual patterns and any recent changes. Assumptions based on incomplete information may lead to incorrect scoring.
- Do use the latest version of the Braden Scale. Healthcare practices evolve, and tools like the Braden Scale are periodically updated to reflect current best practices and research findings. Utilizing the most recent version ensures the assessment aligns with the latest standards in pressure sore risk evaluation.
- Don't forget to seek clarification if you're unsure about how to score an observation. Consult with colleagues or refer to official guidelines for the Braden Scale if a situation falls into a gray area. It's vital that the application of the scale is both consistent and accurate across assessments.
By adhering to these guidelines, healthcare professionals can improve the quality of the Braden Scale assessments they perform. This not only enhances the care provided to individuals at risk of developing pressure sores but also contributes to the broader effort of pressure sore prevention in healthcare settings.
Misconceptions
There are several misconceptions surrounding the Braden Scale for Predicting Pressure Sore Risk, which is a tool used by healthcare professionals to help assess an individual's risk of developing pressure ulcers. These misconceptions can lead to misunderstandings about the scale’s purpose, its application, and the interpretation of its results.
Misconception 1: The Braden Scale is Only for Elderly Patients
While the Braden Scale is often associated with elderly patients, it is applicable to any patient who is at risk for pressure ulcers, regardless of age. The risk factors assessed by the scale, including sensory perception, moisture, activity, mobility, nutrition, and friction and shear, can affect patients of all ages in various healthcare settings.
Misconception 2: A Higher Score Always Means a Lower Risk of Pressure Ulcers
Although it's true that a higher total score on the Braden Scale indicates a lower risk of pressure ulcer development, interpreting these scores should always be done in the context of the individual patient's overall health condition and environment. Other factors not covered by the scale can also influence risk.
Misconception 3: The Braden Scale is a Standalone Tool
Some may believe that the Braden Scale is all that is needed for pressure ulcer prevention. However, it should be used as part of a comprehensive assessment and care plan. The Braden Scale helps identify risk, but preventing pressure ulcers also requires interventions tailored to the patient's specific needs.
Misconception 4: The Scale is Only Useful Upon Admission
While the Braden Scale is often completed upon a patient's admission to a facility, it should be reassessed periodically, especially if the patient's condition changes. Regular reassessment ensures that changes in risk factors are identified and addressed promptly.
Misconception 5: All Sections of the Braden Scale are Equally Weighted
Each section of the Braden Scale assesses different risk factors, and not all are equally weighted in determining the total score. Healthcare professionals must understand how each section contributes to the overall risk assessment to use the scale effectively.
Correcting these misconceptions is crucial for effectively utilizing the Braden Scale to assess and manage the risk of pressure ulcers in patients. By understanding the scale's design, purpose, and proper application, healthcare providers can better protect patients from these serious and potentially life-threatening injuries.
Key takeaways
The Braden Scale is a valuable tool for healthcare professionals, designed to help predict the risk level of patients developing pressure sores. Its effectiveness relies on a comprehensive evaluation of multiple factors. Below are five key takeaways about how to properly fill out and utilize the Braden Scale form:
- Be thorough with each risk factor assessment: The Braden Scale evaluates six primary areas: sensory perception, moisture, activity, mobility, nutrition, and friction & shear. Each area is scored based on the patient's current condition, so it's crucial to accurately assess every aspect to ensure a reliable risk calculation.
- Understand the scoring system: Scores on the Braden Scale range from 6 to 23, with lower scores indicating a higher risk of developing pressure sores. The risk categories are divided into severe (total score 9 or less), high (10-12), moderate (13-14), and mild (15-18) risk levels. It's important to calculate the total score correctly to assign the appropriate risk category to your patient.
- Regular reassessment is key: A patient's condition can change rapidly, influencing their risk level for pressure sores. Regular reassessments using the Braden Scale are necessary, especially if there's a significant change in a patient's mobility, nutritional status, or overall health. This ensures that preventive measures can be adjusted accordingly.
- Use the form as part of a comprehensive care plan: While the Braden Scale provides valuable insights into a patient's risk for pressure sores, it should be used in conjunction with a detailed care plan. This includes implementing preventive measures such as regular position changes, skin inspections, and the use of supportive surfaces, based on the patient's risk level.
- Ensure proper training for staff: Accurate assessment with the Braden Scale requires a good understanding of its components and the ability to evaluate patients effectively. Providing thorough training for all staff members involved in patient care ensures that the Braden Scale is used effectively and consistently across your healthcare facility.
Implementing these key takeaways will enhance the effectiveness of the Braden Scale as a preventative tool in your healthcare setting, ultimately improving patient care and reducing the incidence of pressure sores.
Popular PDF Forms
Florida Toll Exemption Permit - Streamlines the renewal experience for disabled permit holders, laying out a straightforward procedure for updating their exemption status.
Va Form 10-10cg - Financial disclosure on Form 10-10EC determines your extended care service copayment.
Pa 501 - Through this documentation, the government upholds the standards of employment on projects financed by taxpayers, ensuring fair treatment of workers.