Blank Ca Rfa PDF Template
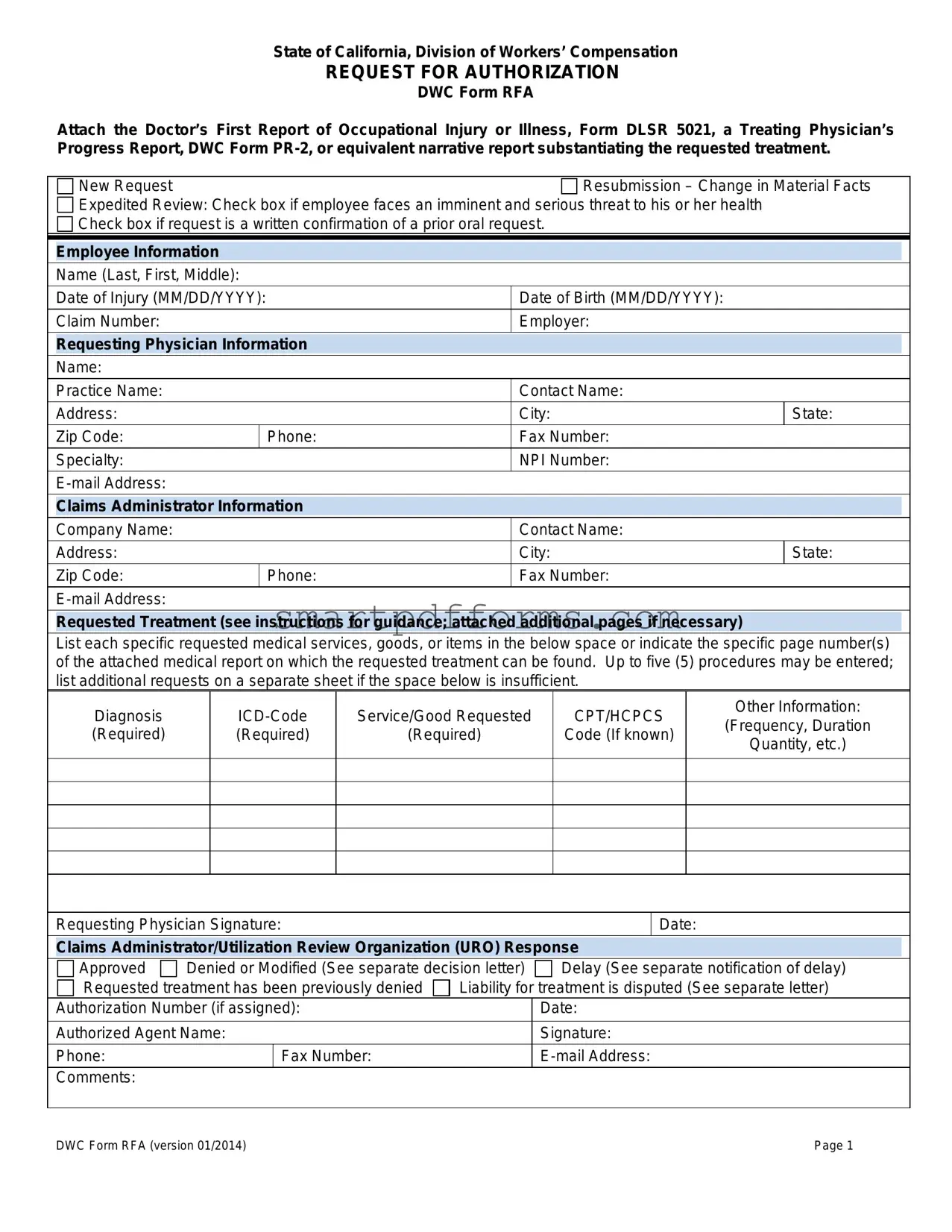
In the realm of workers' compensation in California, ensuring that an injured employee receives timely and appropriate medical treatment is paramount. The DWC Form RFA, standing for Request for Authorization, serves as a critical tool within this process. Crafted by the State of California’s Division of Workers' Compensation, this form is an essential document that facilitates communication between the treating physician and the claims administrator. It signifies the formal request for authorization of medical services, goods, or items deemed necessary for the employee's recovery from an occupational injury or illness. Along with the DWC Form RFA, relevant documentation such as the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, or a Treating Physician’s Progress Report must be attached to substantiate the need for the requested treatment. The form offers options for new treatment requests, resubmissions due to changes in material facts, and expedited reviews in cases where the employee’s health is in imminent danger. Furthermore, it meticulously captures detailed information concerning the employee, the requesting physician, and the claims administrator to streamline the review process. The response segment of the form, completed by the claims administrator or Utilization Review Organization (URO), communicates the decision regarding the treatment authorization clearly and efficiently. The DWC Form RFA exemplifies the structured approach adopted by the Division of Workers’ Compensation to manage and facilitate the delivery of healthcare services to injured workers, underscoring the interconnected roles of documentation, compliance, and timely communication in the realm of workers’ compensation.
Preview - Ca Rfa Form
State of California, Division of Workers’ Compensation
REQUEST FOR AUTHORIZATION
DWC Form RFA
Attach the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form
|
New Request |
|
Resubmission – Change in Material Facts |
|||
|
Expedited Review: Check box if employee faces an imminent and serious threat to his or her health |
|
|
|||
|
Check box if request is a written confirmation of a prior oral request. |
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Employee Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
Name (Last, First, Middle): |
|
|
|
|
|
|
Date of Injury (MM/DD/YYYY): |
|
Date of Birth (MM/DD/YYYY): |
|
|
|
|
Claim Number: |
|
Employer: |
|
|
|
|
Requesting Physician Information |
|
|
|
||
|
|
|
|
|
|
|
|
Name: |
|
|
|
|
|
|
Practice Name: |
|
Contact Name: |
|
|
|
|
Address: |
|
City: |
State: |
||
|
Zip Code: |
|
Phone: |
Fax Number: |
|
|
|
Specialty: |
|
NPI Number: |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
Claims Administrator Information |
|
|
|
||
|
|
|
|
|
|
|
|
Company Name: |
|
Contact Name: |
|
|
|
|
Address: |
|
City: |
State: |
||
|
Zip Code: |
|
Phone: |
Fax Number: |
|
|
Requested Treatment (see instructions for guidance; attached additional pages if necessary)
List each specific requested medical services, goods, or items in the below space or indicate the specific page number(s) of the attached medical report on which the requested treatment can be found. Up to five (5) procedures may be entered; list additional requests on a separate sheet if the space below is insufficient.
Diagnosis (Required)
Service/Good Requested
(Required)
CPT/HCPCS
Code (If known)
Other Information:
(Frequency, Duration
Quantity, etc.)
Requesting Physician Signature:
Date:
Claims Administrator/Utilization Review Organization (URO) Response
Approved |
Denied or Modified (See separate decision letter) |
Delay (See separate notification of delay) |
||
Requested treatment has been previously denied |
Liability for treatment is disputed (See separate letter) |
|||
Authorization Number (if assigned): |
|
Date: |
||
|
|
|
|
|
Authorized Agent Name: |
|
Signature: |
||
Phone: |
|
Fax Number: |
|
|
Comments: |
|
|
|
|
|
|
|
||
DWC Form RFA (version 01/2014) |
|
Page 1 |
||

Instructions for Request for Authorization Form
Warning: Private healthcare information is contained in the Request for Authorization for Medical Treatment, DWC Form RFA. The form can only go to other treating providers and to the claims administrator.
Overview: The Request for Authorization for Medical Treatment (DWC Form RFA) is required for the employee’s treating physician to initiate the utilization review process required by Labor Code section 4610. A Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form
Checkboxes: Check the appropriate box at the top of the form. Indicate whether:
This is a new treatment request for the employee or the resubmission of a previously denied request based on a change in material facts regarding the employee’s condition. A resubmission is appropriate if the facts that provided the basis for the initial utilization review decision have subsequently changed such that the decision is no longer applicable to the employee’s current condition. Include documentation supporting your claim.
Review should be expedited based on an imminent and serious threat to the employee’s health. A request for expedited review must be supported by documentation substantiating the employee’s condition.
The request is a written confirmation of an earlier oral request.
Routing Information: This form can be mailed, faxed, or
Requested Treatment: The DWC Form RFA must contain all the information needed to substantiate the request for authorization. If the request is to continue a treatment plan or therapy, please attach documentation indicating progress, if applicable.
List the diagnosis (required), the ICD Code (required), the specific service/good requested (required), and applicable CPT/HCPCS code (if known).
Include, as necessary, the frequency, duration, quantity, etc. Reference to specific guidelines used to support treatment should also be included.
For requested treatment that is: (a) inconsistent with the Medical Treatment Utilization Schedule (MTUS) found at California Code of Regulations, title 8, section 9792.20, et seq.; or (b) for a condition or injury not addressed by the MTUS, you may include scientifically based evidence published in
Requesting Physician Signature: Signature/Date line is located under the requested treatment box. A signature by the treating physician is mandatory.
Claims Administrator/URO Response: Upon receipt of the DWC Form RFA, a claims administrator must respond within the timeframes and in the manner set forth in Labor Code section 4610 and California Code of Regulations, title 8, section 9792.9.1. To communicate its approval on requested treatment, the claims administrator may complete the lower portion of the DWC Form RFA and fax it back to the requesting provider. (Use of the DWC Form RFA is optional when communicating approvals of treatment; a claims administrator may utilize other means of written notification.) If multiple treatments are requested, indicate in comments section if any individual request is being denied or referred to utilization review.
DWC Form RFA (version 01/2014) |
Page 2 |
Form Data
| Fact Name | Description |
|---|---|
| Form Purpose | The Request for Authorization for Medical Treatment (DWC Form RFA) is designed to initiate the utilization review process as required by California Labor Code section 4610. |
| Required Attachments | A Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form PR-2, or an equivalent narrative report must be attached to substantiate the requested treatment. |
| Governing Laws | The form and its use are governed by provisions in the California Labor Code section 4610 and California Code of Regulations, title 8, section 9789.10 et seq. |
| Response from Claims Administrator/URO | Upon receipt of the DWC Form RFA, the claims administrator must respond within the timeframes and manner dictated by Labor Code section 4610 and California Code of Regulations, title 8, section 9792.9.1. |
Instructions on Utilizing Ca Rfa
Filling out the Request for Authorization (RFA) Form for medical treatment in California involves a series of steps designed to streamline the process of getting necessary medical services approved for workers who have been injured on the job. It’s important to carefully complete each section to ensure a swift review and response from the claims administrator. Below are the detailed instructions to guide you through each part of the form.
- Begin by identifying the type of request at the top of the form. You must check whether this is a New Request, a Resubmission – Change in Material Facts, or if an Expedited Review is necessary. You should also indicate if the form is a written confirmation of a prior oral request.
- Fill in the Employee Information section with the employee’s full name, date of injury, date of birth, claim number, and the employer's name.
- Under Requesting Physician Information, provide the name of the doctor, their practice name, contact name (if any), and contact details including address, phone number, fax number, specialty, NPI number, and email address.
- In the Claims Administrator Information section, record the company name, contact name, and their contact information similarly to how you documented the physician's details.
- For the Requested Treatment section, list each specific medical service, good, or item being requested. Make sure to include the diagnosis with its required ICD code, the service/good requested, and the CPT/HCPCS code if known. Also, detail any pertinent information such as frequency, duration, and quantity.
- The requesting physician must sign and date the form under the requested treatment section to validate the request.
- Attach the necessary supporting documentation, such as a Doctor’s First Report of Occupational Injury or Illness (Form DLSR 5021), a Treating Physician’s Progress Report (DWC Form PR-2), or an equivalent narrative report that substantiates the requested treatment.
- Finally, review the form to ensure all information provided is accurate and complete. Then, send the form and attachments via mail, fax, or email to the claims administrator as directed by the routing information provided by them.
After submitting the Request for Authorization Form, the claims administrator's office will review the request in line with the Labor Code section 4610 and California Code of Regulations. They are required to respond within specific timeframes, communicating their decision on whether the requested treatment has been approved, modified, delayed, or denied. If approved, the authorization number and details will be sent back to the requesting provider, completing the process of authorization for the necessary medical treatment.
Obtain Answers on Ca Rfa
-
What is the DWC Form RFA?
The DWC Form RFA, or Request for Authorization for Medical Treatment, is used by a worker's treating physician to initiate the utilization review process as required by Labor Code section 4610. It includes details about requested medical treatments, diagnoses, and the medical justification for each treatment.
-
What documentation must accompany the DWC Form RFA?
The form must be accompanied by the Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, a Treating Physician’s Progress Report, DWC Form PR-2, or an equivalent narrative report that substantiates the requested treatment.
-
Can this form be submitted for both new requests and resubmissions?
Yes, the form can be used for both new treatment requests and the resubmission of previously denied requests if there has been a change in material facts about the employee's condition. It's important to include supporting documentation for resubmissions.
-
When is an expedited review required?
An expedited review is necessary when the employee faces an imminent and serious threat to their health. Documentation supporting the urgency must be attached to the form.
-
How can the DWC Form RFA be submitted?
This form can be routed via mail, fax, or email to the address, fax number, or email provided by the claims administrator specifically for this purpose.
-
What information is required on the DWC Form RFA?
The form must include comprehensive details about the employee, the requesting physician, and the claims administrator. It should list the diagnosis, ICD code, specific requested treatment(s), and, if known, the CPT/HCPCS codes. Additionally, it should outline the treatment’s frequency, duration, quantity, etc., and reference the guidelines used to support the treatment.
-
What if the requested treatment does not align with the Medical Treatment Utilization Schedule?
If the treatment is inconsistent with the Medical Treatment Utilization Schedule (MTUS) or for a condition not addressed by the MTUS, include evidence from peer-reviewed journals that supports the request.
-
Is a physician’s signature required?
Yes, a signature from the treating physician is mandatory on the DWC Form RFA.
-
How will the Claims Administrator/Utilization Review Organization (URO) respond?
Upon receipt of the form, the Claims Administrator must respond within the timeframes and manner outlined in Labor Code section 4610 and California Code of Regulations, title 8, section 9792.9.1. They may use the DWC Form RFA or other means of written notification to communicate their approval.
-
Is there a specific way to communicate multiple treatment requests?
Yes, if multiple treatments are requested, the response section of the form should indicate if any individual request is being denied or referred to utilization review.
Common mistakes
Filling out the Request for Authorization (RFA) form in the state of California is a critical step for workers seeking approval for medical treatments due to a workplace injury. However, errors can occur during this process, leading to delays or denials of necessary medical care. Here are seven common mistakes to avoid:
-
Not attaching the required medical reports: The form necessitates attaching either a Doctor’s First Report of Occupational Injury or Illness (Form DLSR 5021), a Treating Physician’s Progress Report (DWC Form PR-2), or an equivalent narrative. Failure to attach these documents can result in the immediate rejection of the request.
-
Incorrect or incomplete employee information: Employee details, including their full name, the date of injury, birth date, and claim number, must be accurately filled out. Errors or omissions can cause confusion and delays.
-
Missing physician's details and signature: It's essential to complete all sections relating to the requesting physician, including their name, contact information, and signature. The physician’s signature is mandatory and signifies the authenticity of the request.
-
Omitting details about the requested treatment: The form requires specific information about the diagnosis, ICD code, and the services or goods requested. Neglecting to provide comprehensive details or failing to reference the attached medical report can hinder the review process.
-
Forgetting to check the appropriate boxes at the top: The form provides options to indicate if the request is new, a resubmission based on changed facts, or if expedited review is necessary. Overlooking these options may not convey the urgent needs or the revised circumstances surrounding the request.
-
Not using the provided space efficiently: While the form allows for the listing of up to five procedures, additional pages can be attached if the space below is insufficient. Failing to utilize this option when more treatments are needed can restrict the completeness of the request.
-
Ignoring instructions for routing information: The completed form can be mailed, faxed, or emailed directly to the address or contact information specified by the claims administrator. Bypassing these detailed instructions could mean the request never reaches the intended recipient.
To help facilitate a smoother review process and promote a quicker response, ensure that all elements of the DWC Form RFA are meticulously completed and that no critical information or attachments are omitted. Avoiding these common mistakes can potentially lead to a more favorable outcome for those seeking medical treatment authorization.
Documents used along the form
When working with the California Request for Authorization (Ca RFA) form, it is common practice for several other documents and forms to be used in conjunction, ensuring a comprehensive approach to requesting medical treatment authorization. These documents play a critical role in substantiating the need for the requested treatment, detailing the employee's condition and the medical necessity of the proposed services. Below is a list of documents frequently used alongside the Ca RFA form:
- Doctor's First Report of Occupational Injury or Illness (Form DLSR 5021): This form initiates the claim process by documenting the initial injury or illness that occurred at the workplace. It provides crucial details that support the medical treatment request.
- Treating Physician's Progress Report (DWC Form PR-2): Utilized to report the progress of an injured or ill employee under treatment. It serves as an update to the claims administrator on the employee's condition and the effectiveness of the ongoing treatment.
- Permanent and Stationary Report (DWC Form PR-3 or PR-4): A detailed report prepared when the employee's condition has stabilized and is not expected to improve significantly. It outlines the permanent impacts of the injury and any future treatment that might be needed.
- Utilization Review (UR) Decision Letter: This document communicates the outcome of the UR process, indicating whether the requested medical treatment has been approved, modified, or denied based on medical necessity.
- Request for Second Opinion: If treatment is denied or modified, an employee may seek a second opinion from another physician within the medical provider network (MPN) or, in certain situations, outside of it.
- Appeal Forms: Should there be a dispute over the UR decision, various appeal forms are available, including the Request for Independent Medical Review (IMR) or the Application for Adjudication of Claim, to challenge the decision and seek a resolution.
The integration and appropriate use of these documents and forms alongside the Ca RFA form are essential for navigating the complexities of workers’ compensation claims and ensuring that employees receive the required medical treatment in a timely manner. Coordinating these forms effectively streamlines the process for both the requesting physician and the claims administrator, ultimately facilitating better outcomes for the injured or ill employee.
Similar forms
The Doctor’s First Report of Occupational Injury or Illness, Form DLSR 5021, is similar because it initiates the process of documenting an injury or illness that occurred at the workplace, similar to how the Ca RFA form is used to request authorization for treatment of such injuries or illnesses.
Treating Physician’s Progress Report, DWC Form PR-2, also shares similarities, as it provides updated information on the employee's condition and the effectiveness of the treatment, akin to updates that might be needed for the Ca RFA form during a course of treatment.
Utilization Review Request Form is akin to the Ca RFA form since both are used in the process of reviewing requested medical treatments to ensure they are medically necessary according to established guidelines.
The Prior Authorization Request Form (PAR) used by health insurers is similar because it's also a mechanism to seek approval before administering a specific treatment, ensuring the treatment is covered under the patient’s health insurance policy.
Application for Adjudication of Claim, although more legal in nature, is similar in its function of initiating a process, in this case, a legal review of a workers’ compensation claim, similar to how the Ca RFA form initiates the review for medical treatment authorization.
Medical Treatment Utilization Schedule (MTUS) Application Form has parallels with the Ca RFA form because it is used to determine if a requested treatment aligns with California’s evidence-based treatment standards for workers’ compensation cases.
Return-to-Work (RTW) Form, while focused on the employee’s ability to resume work, relates to the Ca RFA form by focusing on the treatment and recovery process after a workplace injury or illness, affecting decisions around the employee’s work capacity.
Dos and Don'ts
When filling out the Request for Authorization (RFA) form for workers' compensation claims in California, precision and thoroughness are key to ensure a smooth utilization review process. Abiding by specific guidelines can significantly influence the approvability of requested medical treatments for injured employees. Here is a comprehensive list of dos and don'ts:
- Do ensure all necessary reports are attached. The RFA form requires the Doctor’s First Report of Occupational Injury or Illness, a Treating Physician’s Progress Report, or an equivalent narrative report that substantiates the requested treatment. It’s essential to check these documents for completeness and relevance to the current request.
- Don't leave out critical information. Every section of the DWC Form RFA serves a purpose. Not providing detailed information, such as the diagnosis with the required ICD code and the specific service or good requested, including CPT/HCPCS Codes if known, can lead to delays or denials.
- Do clearly indicate the type of request. Identify whether the form is for a new treatment request, a resubmission based on change in material facts, or an expedited review due to an imminent and serious threat to the employee's health. The appropriate box must be checked, and any necessary supporting documentation should be included.
- Don't assume prior communication suffices as documentation. If the request is a written confirmation of a prior oral request, it's crucial to highlight this on the form. However, do not rely exclusively on past communications; ensure all requisite details are current and properly documented within the RFA form itself.
- Do use additional pages if necessary. When the space provided on the form is insufficient to list all requested medical services, goods, or items, attach additional pages with the remaining requests. Ensure these annexes are clearly labeled and referenced in the main form to prevent any oversight or loss during processing.
- Don't forget to sign and date the form. A signature from the requesting physician is mandatory and signifies the authenticity and completion of the request. The absence of a signature can immediately invalidate the form, leading to unnecessary delays in treatment authorization.
Adhering to these guidelines not only facilitates the efficiency of the utilization review process but also supports the timely approval and provisioning of necessary medical treatment for injured workers, ultimately contributing to their rehabilitation and return to work.
Misconceptions
Understanding the California Request for Authorization (RFA) form for medical treatment in workers’ compensation cases is crucial for both healthcare providers and employees. Misconceptions about this form can lead to delays in treatment or misunderstandings about the process. Here are ten common misconceptions explained:
- The RFA form is the only document needed for treatment authorization: This is incorrect. The RFA form must be accompanied by relevant medical reports that substantiate the need for the requested treatment, such as the Doctor’s First Report of Occupational Injury or Illness, or a Treating Physician’s Progress Report.
- Any medical treatment can be requested on the RFA form without justification: This is not true. The form requires detailed information about the diagnosis, the specific service or good requested, and any applicable codes. Additionally, the treatment request must be supported by medical documentation.
- The RFA form guarantees immediate approval of requested treatments: Unfortunately, this is not the case. The response to an RFA can be an approval, denial, or modification, and the decision is typically based on a utilization review process that evaluates the medical necessity and appropriateness of requested treatments.
- The RFA form is only for new treatment requests: This is a misunderstanding. The form can be used for new treatment requests and for resubmissions based on a change in material facts concerning the employee's condition or as a written confirmation of prior oral requests.
- Expedited review is automatically granted if checked on the form: Expedited review is only granted if there is an imminent and serious threat to the employee's health, and this claim must be substantiated with documentation.
- Any physician can request treatment using the RFA form: In fact, the request must come from the employee's treating physician, who provides care under the workers’ compensation system.
- Personal healthcare information on the RFA form can be shared freely: This is false. The RFA form contains private healthcare information and should only be shared with treating providers and the claims administrator handling the worker’s compensation claim.
- The RFA form is a reimbursable document: This is incorrect. The RFA form itself is not separately reimbursable under the Official Medical Fee Schedule for workers’ compensation.
- Approval of treatment via RFA form is final and cannot be disputed: This is not accurate. If treatment is denied or modified, there are procedures in place for appeals or reconsideration based on additional or new medical evidence.
- There is no need to follow up after submitting an RFA form: On the contrary, it's crucial for the requesting physician or the employee to follow up on the request, especially if they have not received a response within the expected timeframe, to ensure timely access to needed medical care.
It's essential for all parties involved in the workers' compensation process to have a clear understanding of the RFA form's purpose, requirements, and processes to ensure timely and appropriate medical treatment for injured employees.
Key takeaways
When seeking authorization for medical treatment in California under the Division of Workers’ Compensation, the Request for Authorization (RFA) form plays a crucial role. Here are key takeaways regarding filling out and using the CA RFA form:
- Required documentation must be attached to the RFA form. This includes a Doctor’s First Report of Occupational Injury or Illness, a Treating Physician’s Progress Report (DWC Form PR-2), or an equivalent narrative report that substantiates the requested treatment.
- The RFA form facilitates new treatment requests or the resubmission of previously denied requests due to a change in material facts regarding the employee’s condition. It’s vital to include supporting documentation if changes in the employee's condition make previous decisions inapplicable.
- If an employee faces an imminent and serious threat to their health, the requesting physician can request an expedited review by checking the appropriate box on the form. This must be supported by the necessary medical documentation.
- All essential information regarding the employee, the claims administrator, and the requesting physician needs to be accurately and completely filled out to avoid any delays in the Utilization Review process.
- The specifics of the requested treatment, including diagnosis, ICD Code, the service or good requested, and if known, the CPT/HCPCS Code, must be clearly listed on the form. Details such as frequency, duration, and quantity, among others, should also be included.
- In cases where the requested treatment does not align with the Medical Treatment Utilization Schedule (MTUS) or pertains to a condition not addressed by the MTUS, the submission should be supported with evidence published in peer-reviewed, nationally recognized journals.
- The requesting physician’s signature is crucial for the form’s submission, emphasizing the importance of the treating physician’s agreement with and justification for the recommended treatment.
- Upon receipt of the RFA, a claims administrator must respond within the allotted time frames and in the manner outlined in Labor Code section 4610 and the California Code of Regulations, title 8, section 9792.9.1, indicating approval, denial, or modification of the requested treatment.
The completion and submission of the RFA form are foundational steps in ensuring that injured employees receive the necessary medical treatment promptly and efficiently, through a process that considers both the medical necessity of treatments and the regulatory requirements set forth by the State of California.
Popular PDF Forms
Purpose of Purchase Requisition Form - Acts as a formal record of the intent to buy, which can be referenced in future for budgeting and audit purposes.
State of Florida School Entry Health Exam - Information on any health condition that may require emergency action at school is highlighted, ensuring proper care.
Hcfa 487 - Assures patients that their treatment plans are being reviewed and modified as necessary by authorized medical personnel.