Blank Clinical Incident Report Sample PDF Template
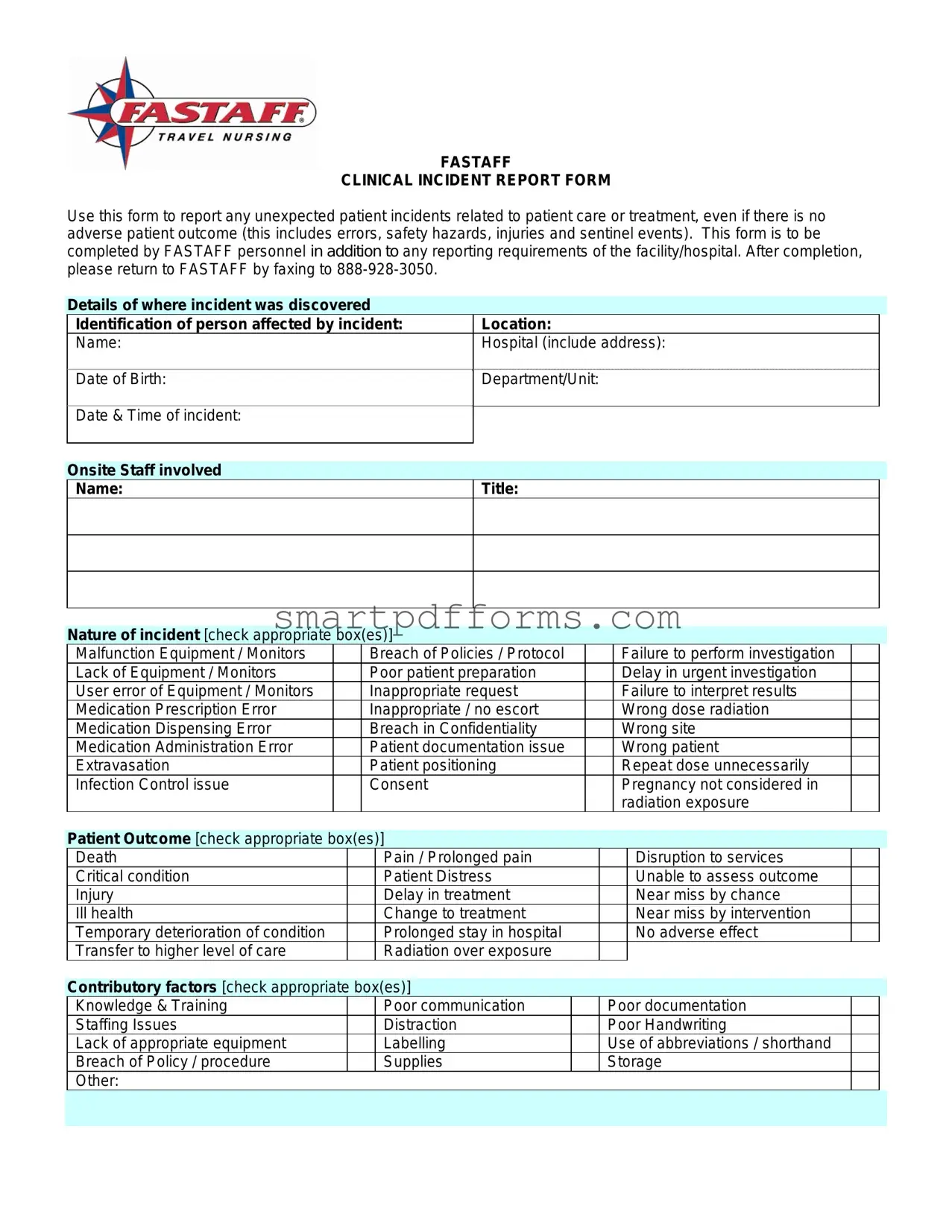
In healthcare settings, ensuring patient safety and care quality is paramount. The FASTAFF Clinical Incident Report Form is an essential tool designed for FASTAFF personnel to meticulously document any unexpected incidents related to patient care or treatment. These incidents may range from errors, safety hazards, and injuries to sentinel events, irrespective of whether they lead to adverse patient outcomes or not. This comprehensive form necessitates the recording of various details, such as the incident's specifics, location, the person affected, the date and time of the incident, and the onsite staff involved. It elaborates on the nature of the incident with options to specify issues like equipment malfunctions, breaches of policies, medication errors, and many other potential problems that can arise in a clinical setting. Significantly, it prompts the reporter to consider the outcome for the patient, contributory factors for the incident, and a summary of the event. Furthermore, it underscores the importance of actions taken in response to the incident to support affected individuals and prevent future occurrences. Finally, the form includes sections for employee acknowledgment and internal use by the FASTAFF Director of Credentialing, ensuring that every report is thoroughly reviewed and acted upon. This form not only serves as a critical incident management tool but also as a catalyst for continuous improvement in patient care standards.
Preview - Clinical Incident Report Sample Form
FASTAFF
CLINICAL INCIDENT REPORT FORM
Use this form to report any unexpected patient incidents related to patient care or treatment, even if there is no adverse patient outcome (this includes errors, safety hazards, injuries and sentinel events). This form is to be completed by FASTAFF personnel in addition to any reporting requirements of the facility/hospital. After completion, please return to FASTAFF by faxing to
|
Details of where incident was discovered |
|
|
|
Identification of person affected by incident: |
Location: |
|
|
Name: |
Hospital (include address): |
|
|
Date of Birth: |
Department/Unit: |
|
|
|
||
|
Date & Time of incident: |
|
|
|
|
|
|
|
|
|
|
Onsite Staff involved Name:
Title:
|
Nature of incident [check appropriate box(es)] |
|
|
|
|
|
|
|||||
|
Malfunction Equipment / Monitors |
|
|
Breach of Policies / Protocol |
|
|
Failure to perform investigation |
|
|
|||
|
Lack of Equipment / Monitors |
|
|
Poor patient preparation |
|
|
Delay in urgent investigation |
|
|
|||
|
User error of Equipment / Monitors |
|
|
Inappropriate request |
|
|
Failure to interpret results |
|
|
|||
|
Medication Prescription Error |
|
|
Inappropriate / no escort |
|
|
Wrong dose radiation |
|
|
|||
|
Medication Dispensing Error |
|
|
Breach in Confidentiality |
|
|
Wrong site |
|
|
|||
|
Medication Administration Error |
|
|
Patient documentation issue |
|
|
Wrong patient |
|
|
|||
|
Extravasation |
|
|
Patient positioning |
|
|
Repeat dose unnecessarily |
|
|
|||
|
Infection Control issue |
|
|
Consent |
|
|
Pregnancy not considered in |
|
|
|||
|
|
|
|
|
|
|
|
|
radiation exposure |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Patient Outcome [check appropriate box(es)] |
|
|
|
|
|
|
|||||
|
Death |
|
|
|
Pain / Prolonged pain |
|
|
|
Disruption to services |
|
|
|
|
Critical condition |
|
|
|
Patient Distress |
|
|
|
Unable to assess outcome |
|
|
|
|
Injury |
|
|
|
Delay in treatment |
|
|
|
Near miss by chance |
|
|
|
|
Ill health |
|
|
|
Change to treatment |
|
|
|
Near miss by intervention |
|
|
|
|
Temporary deterioration of condition |
|
|
|
Prolonged stay in hospital |
|
|
|
No adverse effect |
|
|
|
|
Transfer to higher level of care |
|
|
|
Radiation over exposure |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
Contributory factors [check appropriate box(es)] |
|
|
|
|
|
|
|||||
|
Knowledge & Training |
|
|
|
Poor communication |
|
|
Poor documentation |
|
|
||
|
Staffing Issues |
|
|
|
Distraction |
|
|
Poor Handwriting |
|
|
||
|
Lack of appropriate equipment |
|
|
|
Labelling |
|
|
Use of abbreviations / shorthand |
|
|
||
|
Breach of Policy / procedure |
|
|
|
Supplies |
|
|
Storage |
|
|
||
|
Other: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

Summary of what happened: (please state facts only and not opinion – attach separate sheet if necessary) Ensure that all necessary steps have been taken to support and treat anyone injured and prevent injury to others. Ensure medical records are factual and up to date.
Action Taken as a Result of Incident: (please give brief
Employee Acknowledgment |
|
Employee Name: |
Title/Position: |
Acknowledgment - I acknowledge that the facts and circumstances reported above are true and accurate to the best of my knowledge:
______________________________________________________
Employee Signature |
Date |
INTERNAL USE ONLY – COMPLETED BY FASTAFF DIRECTOR OF CREDENTIALING
Action Taken as a Result of Incident: (please give brief
____________________________________________________________________
Director of Credentialing |
Date |
Form Data
| Fact Number | Description |
|---|---|
| 1 | The FASTAFF Clinical Incident Report Form is designed to report unexpected patient incidents related to care or treatment. |
| 2 | Incidents can be reported even if there is no adverse patient outcome. |
| 3 | The form is intended for use by FASTAFF personnel, in addition to any reporting requirements of the facility or hospital. |
| 4 | Completed forms should be returned to FASTAFF by faxing to the number 888-928-3050. |
| 5 | The form requires the identification of the person affected by the incident, including details such as location, name, hospital address, department/unit, and date & time of incident. |
| 6 | It includes a section for detailing the nature of the incident, with checkboxes for various categories such as equipment malfunction, breach of policies, medication errors, and more. |
| 7 | There is a specific section to record the patient outcome, which could range from death, pain, or no adverse effect, to transfer to higher level of care. |
| 8 | Contributory factors that led to the incident can be indicated, covering aspects like knowledge & training, staffing issues, and lack of appropriate equipment. |
| 9 | Reports must include a summary of what happened, emphasizing that only facts should be stated, not opinions. A separate sheet can be attached if necessary. |
| 10 | There is a section for employee acknowledgment, requiring the employee's name, title, and signature to confirm the accuracy of the report. |
Instructions on Utilizing Clinical Incident Report Sample
When an unexpected patient incident occurs, it's crucial to document every detail accurately to ensure proper follow-up and to prevent future incidents. The fast response can significantly impact patient care and safety. The Clinical Incident Report Form provided by FASTAFF is designed for such situations. This guide will walk you through the process of completing this form, ensuring that all relevant information is captured and communicated effectively.
- Start by noting the details of where and when the incident was discovered, including the Location and Hospital Address.
- Identify the person affected by the incident: fill in their Name, Date of Birth, Department/Unit, and the Date & Time of the incident.
- Record the Name and Title of any Onsite Staff involved in the incident.
- Next, describe the Nature of the incident by checking the appropriate box(es) that best describe what happened, such as Equipment Malfunction or Medication Prescription Error.
- Outline the Patient Outcome by checking the appropriate box(es) to indicate how the patient was affected, ranging from No adverse effect to Death.
- Identify any Contributory factors by checking the relevant box(es), like Knowledge & Training or Staffing Issues, which could have played a role in the incident.
- In the Summary section, clearly state the facts of what happened without including any opinion. Attach a separate sheet if more space is needed.
- Detail any Action Taken as a Result of the Incident immediately following the event, including efforts to support and treat anyone injured and measures taken to prevent future incidents. Attach additional pages if necessary.
- Under the Employee Acknowledgment section, the employee should print their Name, Title/Position, provide their signature, and date the form to confirm that the information reported is true and accurate.
- Finally, the completed form should be returned to FASTAFF by faxing it to the provided number: 888-928-3050. The Director of Credentialing at FASTAFF will then fill in the internal use section, detailing any further action taken as a result of the incident.
By carefully following these steps, staff can ensure that all essential details of the incident are accurately reported and available for review. This proactive approach not only aids in addressing the immediate situation but also contributes to the continuous improvement of patient care and safety protocols.
Obtain Answers on Clinical Incident Report Sample
Who should complete the Clinical Incident Report Form?
The Clinical Incident Report Form is designed to be completed by FASTAFF personnel. These individuals are required to report any unexpected patient incidents that are related to patient care or treatment. It's essential to note that this requirement remains regardless of whether there is an adverse patient outcome. Such incidents could include errors, safety hazards, injuries, and sentinel events. Completing this form is in addition to any reporting obligations the personnel may have towards the facility or hospital where the incident occurred.
How should the form be submitted after completion?
Once the Clinical Incident Report Form is filled out, it should be returned to FASTAFF by faxing the completed form to the designated fax number: 888-928-3050. This process ensures a timely and secure submission of the report, allowing FASTAFF to take any necessary follow-up actions regarding the reported incident. It is crucial to follow through with this step promptly to ensure the health and safety of patients and to adhere to both FASTAFF and facility reporting protocols.
What information is required on the form?
The form requires detailed information to accurately document the incident. This includes the location and identification of the person affected by the incident—name, hospital address, date of birth, department/unit, and the date and time when the incident occurred. The onsite staff involved must also be identified by name and title. The nature of the incident needs to be described by checking the appropriate box(es) that best describe the incident such as equipment malfunction, medication errors, patient documentation issues, etc. The patient outcome and any contributory factors to the incident should also be described in detail. Lastly, a summary of the incident, action taken as a result, and an employee acknowledgment section must be completed to provide a comprehensive overview of the situation.
What actions should be taken after reporting an incident?
After reporting an incident using the Clinical Incident Report Form, there are several steps FASTAFF personnel should take to ensure the safety and well-being of patients and staff. Firstly, immediate steps must be taken to support and treat anyone injured and to prevent further injuries. Medical records should be updated to reflect factual, accurate, and up-to-date information regarding the incident. Any necessary follow-up actions detailed on the form should be carried out, such as additional reports or corrective measures to prevent future incidents. The Director of Credentialing at FASTAFF will review the submitted report and take further actions as necessary, which might include internal reviews, additional training, or changes in policies or procedures to improve safety and care standards.
Common mistakes
When filling out the Clinical Incident Report Sample form, individuals often make several common mistakes. Recognizing and avoiding these errors can ensure accurate and efficient incident reporting, essential for improving patient care and safety. Here are seven mistakes to be mindful of:
Not providing complete details of the incident location. It's crucial to include the full address of the hospital and the specific department or unit where the incident occurred to facilitate a prompt response and thorough investigation.
Omitting information about the person affected by the incident. Full identification including name, date of birth, and any relevant patient identifiers ensures the correct individual is linked to the report and any necessary follow-up actions.
Skipping details about the onsite staff involved. Identifying the staff on duty by name and title at the time of the incident helps in understanding the situational context and determining accountability.
Incomplete description of the nature of the incident. Checking the appropriate box(es) is helpful, but providing a detailed summary of the events leading to the incident, without personal opinions, is essential for a thorough investigation.
Failing to record the patient outcome accurately. Understanding the short and long-term effects on the patient's health can guide improvements in care and protocol adjustments.
Overlooking contributory factors. Acknowledging elements like knowledge and training deficiencies, poor communication, or equipment issues can help in identifying systemic problems and prevent future incidents.
Not specifying actions taken in response to the incident. Documenting the immediate and corrective actions taken not only demonstrates an undertaking of responsibility but also aids in the development of strategies to prevent recurrence.
By ensuring these aspects are thoroughly and accurately completed, personnel can contribute to a culture of safety and continuous improvement within healthcare settings.
Documents used along the form
In healthcare settings, the completion and submission of a Clinical Incident Report form reflect a critical step in addressing unexpected patient incidents but are just one part of a comprehensive approach to incident management. To ensure thorough documentation, analysis, and follow-up, several other forms and documents are commonly utilized in conjunction with the Clinical Incident Report. These documents play a pivotal role in facilitating a deeper understanding of the incident, fostering a culture of safety, and promoting continuous improvement in patient care.
- Patient Consent Form: This document records the patient’s agreement to undergo the proposed care or treatment. It’s essential when investigating incidents where there may have been a misunderstanding or lack of informed consent.
- Medication Administration Record (MAR): An MAR is crucial when a medication error is involved. It provides a complete record of all medicines administered to the patient, which can be cross-referenced with the Clinical Incident Report.
- Treatment Plan: This outlines the planned care and interventions for a patient. In the context of an incident report, the treatment plan can help identify deviations or failures to follow the planned care pathway.
- Staff Shift Roster: When staffing issues or fatigue are contributory factors in an incident, the shift roster can be reviewed to identify patterns or issues with staffing levels or workloads.
- Equipment Maintenance Log: For incidents involving malfunctioning equipment, this log provides records of maintenance, repairs, and inspections, which can help identify if equipment failure contributed to the incident.
- Patient Care Record: This comprehensive document details all aspects of patient care and interactions. It is vital for cross-referencing with the Clinical Incident Report to get a full picture of the patient's care trajectory.
- Incident Investigation Report: Following the initial reporting via the Clinical Incident Report form, an in-depth investigation report may be compiled, offering detailed analysis and recommendations for preventing future occurrences.
- Quality Improvement Documentation: This documentation captures the resultant actions taken to improve processes and prevent reoccurrence of similar incidents. It may include training records or policy updates.
Each of these documents contributes to a holistic approach to incident management, offering various perspectives and data that, together, enable healthcare providers to mitigate risks, enhance patient safety, and improve the overall quality of care. Careful and systematic documentation not only supports individuals affected by the incident but also underpins an organization's commitment to transparency, accountability, and continuous improvement.
Similar forms
The Clinical Incident Report Sample form is crucial in healthcare settings for documenting any unforeseen patient care incidents, underscoring the importance of accurate and thorough reporting. Here are nine documents that share similarities with the Clinical Incident Report form, each playing a vital role in various professional and operational contexts:
Incident Report Forms in Non-Healthcare Settings: Like the Clinical Incident Report, these forms are used in workplaces outside the healthcare sector to document accidents, injuries, or any unusual incidents. They share the objective of recording the immediate facts and initiating a response to prevent future occurrences.
Medication Error Reporting Forms: These are specialized forms used by healthcare providers to report errors in prescribing, dispensing, or administering medication. Similar to the Clinical Incident Report, they contribute to improving patient safety by identifying and analyzing medication errors.
Safety Hazard Reporting Forms: Often found in industrial or construction settings, these forms document potential safety hazards. Like clinical incident reports, they aim to preemptively address conditions that could lead to accidents or injuries.
Quality Assurance Reports: These reports are used across various industries to document issues that affect the quality of products or services, including healthcare. They similarly focus on identifying and correcting systemic problems to enhance outcomes.
Patient Complaint Forms: These forms allow patients to report dissatisfaction with healthcare services. While their primary focus is on service rather than clinical errors, they similarly trigger a review process aimed at resolving issues and improving patient satisfaction.
Equipment Failure Reports: Specifically used for documenting malfunctions in medical (or other industry) equipment, these reports share similarities with incident reports by detailing an equipment issue, its impact, and the steps taken to resolve it.
Compliance Violation Reports: These forms document instances where policies or regulations are not followed. Much like Clinical Incident Reports, they are essential for maintaining standards and preventing harm in healthcare settings and beyond.
Emergency Response Forms: Used by first responders and emergency medical technicians (EMTs), these forms record the details of emergency incidents and the response provided. They share the Clinical Incident Report’s goal of documenting critical information for immediate action and future review.
Radiation Exposure Incident Forms: Specific to areas where radiation is used, such as radiology departments or nuclear facilities, these forms document incidents of unintended exposure. Their usage parallels the Clinical Incident Report in focusing on immediate documentation to inform corrective actions and protect patient or worker safety.
Dos and Don'ts
When filling out the Clinical Incident Report Sample form, there are several key practices to ensure the report is accurate, complete, and contributes to the improvement of patient care and safety. Here is a list of things you should and shouldn't do:
Do:- Report promptly: Fill out the form as soon as possible after the incident to ensure that details are accurate and not forgotten.
- Be factual: Describe exactly what happened, sticking to the facts without including personal opinions or assumptions.
- Include specifics: Provide detailed information about the location, date and time of the incident, persons involved, and the nature of the incident.
- Use clear language: Write in clear, straightforward language to ensure that anyone reading the report can understand the circumstances and actions taken.
- Review for accuracy: Before submitting, review the form for completeness and accuracy, ensuring all sections are filled out appropriately.
- Include action taken: Describe any immediate actions taken in response to the incident to address the situation and prevent further harm.
- Attach additional documentation if necessary: If more space is required to provide a thorough account, attach additional sheets clearly marked with the relevant section of the report they correspond to.
- Update medical records: Ensure relevant information about the incident is accurately reflected in the patient’s medical records.
- Use checked boxes appropriately: Make sure to mark the relevant boxes accurately to reflect the nature of the incident and the patient outcome.
- Sign and date the form: Ensure the form is signed and dated to authenticate the report.
- Delay reporting: Avoid waiting several days to fill out the form, as this can lead to inaccuracies or forgotten details.
- Include identifiers in summaries: Do not use names or other personal identifiers in the summary section; these should be included in the designated fields only.
- Use medical jargon or abbreviations: Avoid using medical jargon or abbreviations that might not be understood by all readers of the report.
- Assign blame: Steer clear of language that directly or indirectly assigns blame to individuals or groups.
- Forget to describe the outcome: Failing to check the appropriate boxes or describe the patient outcome can leave the report incomplete.
- Submit without reviewing: Never submit the report without thoroughly reviewing it for errors or omissions.
- Assume knowledge: Do not assume that the reader has prior knowledge about the incident; provide a comprehensive account.
- Use vague language: Avoid vague statements that do not adequately describe the incident or actions taken.
- Omit contributory factors: Forgetting to check boxes that identify contributory factors can result in an incomplete analysis of the incident.
- Leave sections blank: Do not leave sections unanswered unless they truly do not apply to the incident being reported.
Misconceptions
Misconceptions About the Clinical Incident Report Sample Form
Clinical Incident Report Forms are essential in healthcare settings, but there are several common misunderstandings about them. Below are seven misconceptions and explanations to clarify them.
It's only for reporting adverse patient outcomes: This form is not just for incidents with bad outcomes. It's for any unexpected incident related to patient care or treatment, even if no harm occurred.
Only medical errors need to be reported: Besides errors, the form covers a wide range of incidents, including safety hazards, injuries, equipment malfunctions, and breaches of policies or protocols.
Filled out only by doctors: The form should be completed by any FASTAFF personnel who witness or discover the incident, not just doctors. This includes nurses, technicians, and other staff members.
Reporting is optional: Reporting is not optional. The form states it must be completed in addition to any facility or hospital reporting requirements, emphasizing the importance of documenting every incident.
It's complicated to fill out: While it might seem daunting, the form clearly guides the reporter through documenting essential information, including details of the incident, the person affected, and any actions taken afterward.
Details about the incident are unnecessary: The form requires a factual summary of what happened without opinion. This detailed account is vital for understanding the incident fully and taking appropriate actions.
Submitting the form leads to negative consequences: The purpose of the form is not to assign blame but to improve patient safety and care. It helps identify areas for improvement and prevent future incidents.
Understanding the purpose and requirements of the Clinical Incident Report Sample Form is crucial for all healthcare personnel. It is a tool for learning and prevention, designed to enhance the safety and quality of patient care.
Key takeaways
Filling out the Clinical Incident Report Sample form correctly is essential for ensuring that patient care issues are addressed promptly and effectively. Here are seven key takeaways for using this form:
- It's vital to report any unexpected patient incidents related to patient care or treatment, regardless of the outcome. This includes errors, safety hazards, injuries, and sentinel events.
- The form must be completed by FASTAFF personnel, in addition to any reporting requirements mandated by the facility or hospital involved.
- To return the completed form to FASTAFF, it should be faxed to the number provided: 888-928-3050.
- When filling out the form, it's essential to include specific details about the incident, such as where it was discovered, the identification of the person affected, and the nature of the incident by checking the appropriate boxes provided.
- Ensure that the Patient Outcome section is selected accurately to reflect the result of the incident, helping FASTAFF to understand the severity and implications of the event.
- In the 'Action Taken as a Result of Incident' section, it is necessary to provide a brief description of the measures taken following the incident. If more space is required, an additional sheet can be attached.
- The form requires an Employee Acknowledgment, where the reporting individual confirms the accuracy of the information provided to the best of their knowledge. This is followed by the signature of the employee and the date, adding a declarative affirmation about the report's authenticity.
This process is designed not only to capture crucial details about clinical incidents but also to ensure that appropriate follow-up actions are taken to prevent future occurrences, making it a critical tool in maintaining and enhancing patient safety and care quality.
Popular PDF Forms
Religious Vaccine Exemption - While this form provides a means to bypass vaccination mandates, it also emphasizes the importance of truthful, faith-based claims.
4 Animal Personality Types - An illuminating tool to gauge your predispositions and how they shape your interaction with the world.
Ms Harvest Permit - Harvest permit application guidance, highlighting required company details and financial transaction methods.