Blank Cms 10123 Nomnc PDF Template
Navigating the complexities of Medicare and understanding when coverage for services will end can be overwhelming for patients and their families. At the heart of this process is the CMS 10123 NOMNC form, a crucial document that serves as a notice to Medicare recipients about the discontinuation of coverage for specific services. This form is issued by providers or health plans to inform patients that Medicare is unlikely to continue paying for their current services after a given date, putting the responsibility on the patient for any subsequent charges unless they act swiftly. Importantly, the form outlines the patient's right to appeal this decision, offering a pathway to contest the termination of funding through an immediate, independent medical review. Such an appeal must be requested promptly, specifically no later than noon of the day before the effective termination date of coverage, through the designated Beneficiary and Family-Centered Care Quality Improvement Organization (BFCC-QIO). The appeal process is designed to ensure patients have the opportunity to have their cases reviewed fairly, potentially allowing for the continuation of services if the independent reviewer rules in their favor. However, if the appeal is not successful, or if the patient chooses not to appeal, they face the possibility of financial liability for future services. Understanding the details, deadlines, and procedures outlined in the CMS 10123 NOMNC form is vital for patients navigating the potential end of Medicare coverage for their services, emphasizing the importance of informed and timely actions in the face of such notifications.
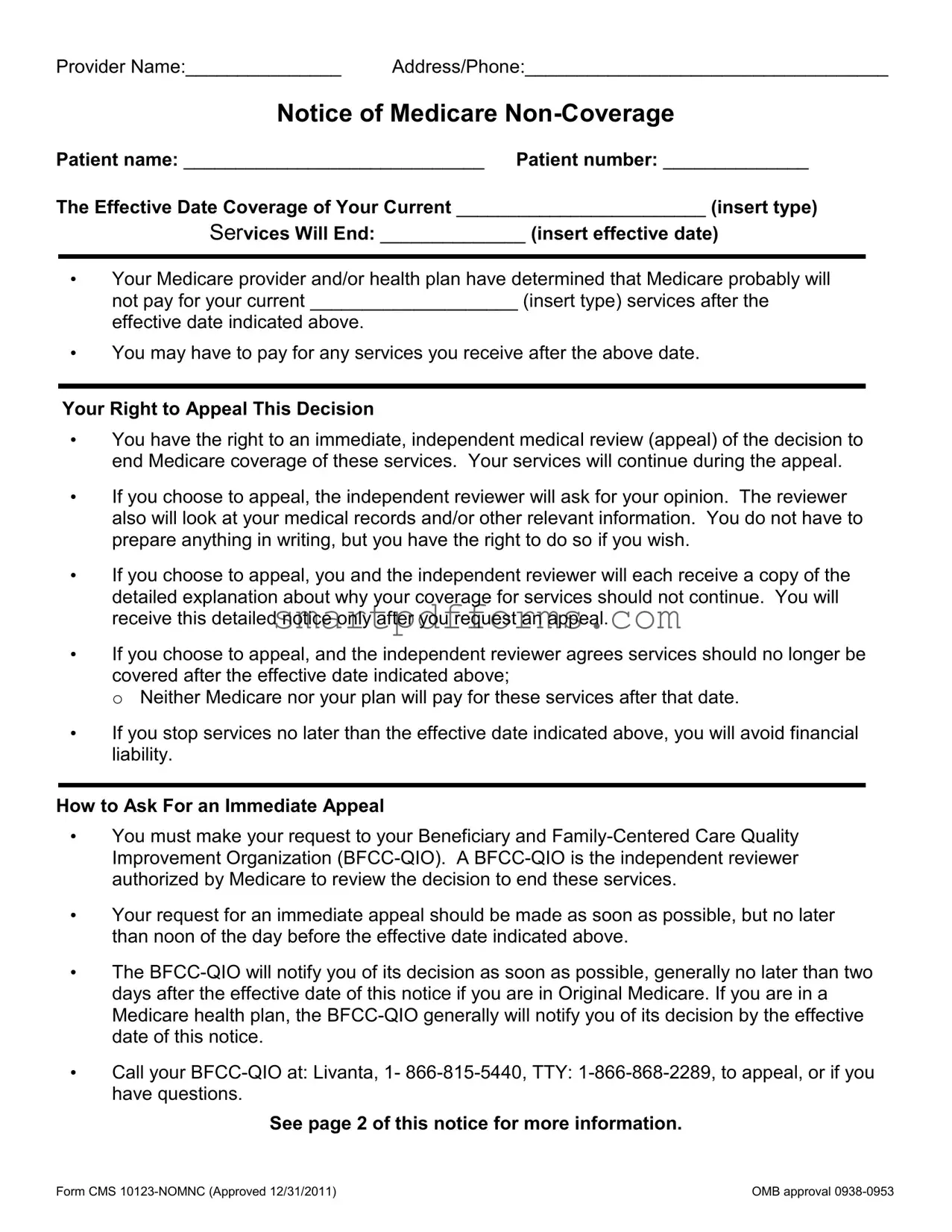
Preview - Cms 10123 Nomnc Form
Provider Name:_______________ Address/Phone:___________________________________
Notice of Medicare
Patient name: _____________________________ Patient number: ______________
The Effective Date Coverage of Your Current ________________________ (insert type)
Services Will End: ______________ (insert effective date)
•Your Medicare provider and/or health plan have determined that Medicare probably will not pay for your current ____________________ (insert type) services after the effective date indicated above.
•You may have to pay for any services you receive after the above date.
Your Right to Appeal This Decision
•You have the right to an immediate, independent medical review (appeal) of the decision to end Medicare coverage of these services. Your services will continue during the appeal.
•If you choose to appeal, the independent reviewer will ask for your opinion. The reviewer also will look at your medical records and/or other relevant information. You do not have to prepare anything in writing, but you have the right to do so if you wish.
•If you choose to appeal, you and the independent reviewer will each receive a copy of the detailed explanation about why your coverage for services should not continue. You will receive this detailed notice only after you request an appeal.
•If you choose to appeal, and the independent reviewer agrees services should no longer be covered after the effective date indicated above;
o Neither Medicare nor your plan will pay for these services after that date.
•If you stop services no later than the effective date indicated above, you will avoid financial liability.
How to Ask For an Immediate Appeal
•You must make your request to your Beneficiary and
•Your request for an immediate appeal should be made as soon as possible, but no later than noon of the day before the effective date indicated above.
•The
•Call your
See page 2 of this notice for more information.
Form CMS |
OMB approval |
If You Miss The Deadline To Request An Immediate Appeal, You May Have Other Appeal Rights:
•If you have Original Medicare: Call the
•If you belong to a Medicare health plan: Call your plan at the number given below.
Plan Contact Information:
UPMC for Life
APPEALS & GRIEVANCES
PO BOX 2939
PITTSBURGH, PA 15230
CALL:
8 a.m. to 8 p.m., Monday through Friday and 8 a.m. to 3 p.m. on Saturday FAX:
Additional Information (Optional):
Please sign below to indicate you have received this notice.
I have been notified that coverage of my services will end on the effective date indicated on this notice and that I may appeal this decision by contacting my QIO.
Signature of Patient or Representative |
Date |
Form CMS |
OMB approval |
Form Data
| Fact Name | Description |
|---|---|
| Form Purpose | The CMS 10123-NOMNC form is used to notify a patient that their Medicare provider has determined Medicare likely will not cover their services after a specified date. |
| Right to Appeal | Patients have the right to an immediate, independent medical review (appeal) if they disagree with the decision to end coverage of services. Services will continue during the appeal process. |
| How to Appeal | Patients must request an immediate appeal through their Beneficiary and Family-Centered Care Quality Improvement Organization (BFCC-QIO) as soon as possible but no later than noon of the day before the effective date indicated. |
| Appeal Outcome | If the independent reviewer agrees that services should no longer be covered after the effective date, neither Medicare nor the patient’s plan will pay for the services beyond that date. |
| Governing Law | This form follows federal Medicare regulations, applicable throughout the United States, with appeals processed by BFCC-QIOs designated for each state or region. |
Instructions on Utilizing Cms 10123 Nomnc
Filling out the CMS 10123 NOMNC form is a necessary step for patients who have been informed their Medicare coverage for certain services will soon end. This form initiates the process to appeal that decision. It’s important to complete and submit this document promptly to ensure your rights are protected and to potentially continue receiving the necessary services without interruption. Here’s a guide to help you accurately fill out the form.
- Start by entering the Provider Name in the designated space at the top of the form.
- Next, fill in the Address/Phone section with the provider's address and contact number.
- Under the section titled Notice of Medicare Non-Coverage, write the Patient Name and Patient Number in the appropriate fields.
- In the line that begins with “The Effective Date Coverage of Your Current,” insert the type of service that is being discontinued.
- Next to this, you will see a space to fill in the effective date when this coverage is slated to end. Make sure to write this date clearly.
- Read through the rights and instructions provided, ensuring you understand the implications and the steps for appealing the decision.
- If you decide to request an immediate appeal, note the phone number provided for Livanta, the Beneficiary and Family Centered Care Quality Improvement Organization (BFCC-QIO), and be prepared to contact them promptly.
- For those with Original Medicare, make a note of the deadline to request an appeal, which is no later than noon of the day before the effective end date indicated.
- If you belong to a Medicare health plan, the plan’s contact information is provided. Record the phone and fax numbers, as well as the hours of operation for future reference.
- Finally, at the bottom of the form, the Signature of Patient or Representative line must be signed, and the Date of signing entered, to acknowledge receipt of this notice and the intent to appeal (if applicable).
After completing and submitting this form, an immediate action will be initiated to review your case. It's critical to follow through with the appeal process swiftly to ensure your services may continue without disruption. Remember, the BFCC-QIO is there to assist you through this process, so do not hesitate to reach out to them for guidance or with any questions you might have.
Obtain Answers on Cms 10123 Nomnc
What is the CMS 10123-NOMNC form?
The CMS 10123-NOMNC form, standing for Notice of Medicare Non-Coverage, informs Medicare recipients that Medicare will likely not cover their current services beyond a specified effective date. This document details the type of services being terminated, the effective date of termination, and the patient’s rights to appeal this decision.
Why would I receive a CMS 10123-NOMNC form?
You would receive this notice because your Medicare provider or health plan has determined that your current services will no longer be covered by Medicare after a certain date. It serves as a formal notification and also outlines your immediate rights to challenge this decision.
What are my rights if I receive this notice?
Upon receiving the CMS 10123-NOMNC form, you have the right to an immediate, independent medical review (appeal) of the decision to end coverage for your services. Importantly, your services will continue during the appeal process. You are not required to prepare anything in writing for your appeal, but you have the option to do so.
How do I request an appeal?
To appeal, you must contact your Beneficiary and Family-Centered Care Quality Improvement Organization (BFCC-QIO) as soon as possible, but no later than noon the day before the effective termination date indicated on the form. The BFCC-QIO is the independent reviewer authorized by Medicare to review the decision.
What happens if I miss the deadline to request an immediate appeal?
If you miss the deadline, you might still have other appeal rights. If you have Original Medicare, you should call the BFCC-QIO listed on the form. If you belong to a Medicare health plan, you should call your plan using the contact information provided on the form.
What happens if I decide not to appeal?
If you choose not to appeal and your services are discontinued on the effective date indicated, Medicare or your plan may not cover the services received after this date. If you discontinue services by this date, you can avoid financial liability for further services.
Where can I find the contact information to appeal?
The form provides specific contact information for the BFCC-QIO, including a phone number and TTY number for appeals or questions. Additionally, for those in a Medicare health plan, the form will include your plan's contact information for appeals and grievances.
Common mistakes
Filling out the CMS 10123 NOMNC form correctly is critical for patients facing the end of Medicare coverage for certain services. However, common mistakes can create unnecessary complications or delays. Here are eight frequent errors:
- Incorrect or Incomplete Provider Information: Failing to accurately provide the name, address, and phone number of the provider can lead to confusion and delays in processing the form.
- Not Specifying Patient Information Completely: Omitting patient name or number can make it difficult to identify the individual in question, complicating the appeal process.
- Leaving the Type of Services Blank: Not inserting the type of services being discontinued can result in a lack of clarity about what coverage is ending.
- Incorrect Effective Date: Misstating the effective date of when services will end can lead to misunderstandings about the appeal timeline.
- Omitting the Appeal Process Details: Patients often overlook their right to an immediate, independent medical review. Not understanding or utilizing this right can result in unwarranted charges.
- Failure to Contact the BFCC-QIO Promptly: Not contacting the Beneficiary and Family-Centered Care Quality Improvement Organization promptly can lead to missed deadlines for appealing the decision.
- Not Utilizing the Right to Provide Additional Information: Patients sometimes fail to realize they can provide additional information or documentation to support their appeal, potentially missing an opportunity to affect the outcome.
- Not Signing the Form: A simple but critical oversight is failing to sign and date the bottom of the form, which could render the appeal process invalid.
Ensuring that all sections of the CMS 10123 NOMNC form are correctly filled out and submitted on time can significantly affect a patient's ability to appeal Medicare's decision. Awareness and attention to detail can help avoid these common mistakes.
Documents used along the form
Understanding the CMS 10123 NOMNC (Notice of Medicare Non-Coverage) form is essential for patients and their families when services covered by Medicare are about to end. However, this form is often not the only document needed during such times. Several other forms and documents frequently accompany the CMS 10123 NOMNC form to ensure that patients smoothly navigate their healthcare transitions and understand their rights and responsibilities fully.
- Form CMS-20027: This form is used to file a written complaint or appeal against a Medicare health plan or any provider. It's crucial for individuals who disagree with a coverage or payment decision made by Medicare.
- Form CMS-R-131 (Advance Beneficiary Notice of Noncoverage): This notice is provided by providers before furnishing a service or item that Medicare is likely not to pay for. It helps patients decide whether to proceed with the service and accept financial responsibility.
- Form CMS-10260: This is the detailed explanation of non-coverage decision required if a beneficiary decides to appeal a NOMNC decision. It provides comprehensive reasons why Medicare believes the services should no longer be covered.
- Beneficiary Notice of Appeal Rights: A document detailing a beneficiary's rights to appeal a health plan's decision. It outlines the process for requesting a reconsideration or hearing to dispute the plan's decision.
- Appointment of Representative Form (CMS-1696): This form allows a beneficiary to appoint another person to act on their behalf in dealing with Medicare, including filing an appeal. This can be particularly useful if the beneficiary needs assistance managing their Medicare coverage and decisions.
- Medicare Summary Notice (MSN): The MSN is a summary of services billed to Medicare, showing what Medicare paid and what the beneficiary may owe the provider. It is essential for tracking charges and understanding potential costs not covered by Medicare.
- State-specific Medicaid forms: If a patient is also a Medicaid recipient, various state-specific forms may be required to coordinate benefits or appeal coverage decisions. These forms ensure that patients can access their entitled Medicaid benefits in addition to Medicare.
- Quality Improvement Organization (QIO) Complaint Form: If a patient believes the quality of care received was inadequate, this form allows filing a complaint with the QIO. It is instrumental in ensuring that care standards are met and maintained.
Each of these documents plays a vital role in facilitating patients' understanding and management of their healthcare services, especially when facing the termination of Medicare-covered services. By familiarizing themselves with these forms, patients and their advocates can ensure they are well-equipped to navigate their healthcare journeys effectively.
Similar forms
The CMS-L564 Request for Employment Information form is similar to the CMS 10123 NOMNC form in that both are used in conjunction with Medicare services. The CMS-L564 is used to provide proof of employment, group health plan coverage, and the end of such coverage, which is pertinent to Medicare eligibility and premium calculations, much like how the NOMNC is used to notify of the end of covered services.
The Advance Beneficiary Notice of Noncoverage (ABN), Form CMS-R-131, shares similarities with the CMS 10123 NOMNC as it also informs Medicare recipients about services or items that Medicare is not expected to pay for. Both documents are designed to alert beneficiaries of potential out-of-pocket expenses and grant them the opportunity to make informed decisions about their care and coverage.
Medicare Redetermination Request Form parallels the CMS 10123 NOMNC by involving Medicare beneficiaries in the appeal process regarding coverage decisions. While the NOMNC notifies beneficiaries of the termination of service coverage, the Redetermination Request Form is used by beneficiaries to appeal previous Medicare coverage or payment decisions.
The Medicare Authorization to Disclose Personal Health Information form intersects with the CMS 10123 NOMNC through their mutual association with Medicare policies. This authorization form allows Medicare to release personal health information, highlighting the importance of informed consent and awareness, similar to the NOMNC’s role in making the beneficiary aware of coverage decisions and their rights.
The Notice of Privacy Practices shares a connection with the CMS 10123 NOMNC due to both documents being focused on the rights of individuals under healthcare policies. While the Notice of Privacy Practices informs patients about how their medical information may be used and disclosed, the NOMNC specifically deals with the cessation of Medicare-covered services and the beneficiary’s right to appeal such decisions.
Appointment of Representative Form, CMS Form No. 1696, has similarities with the CMS 10123 NOMNC because both pertain to Medicare beneficiaries’ rights and the processes available to them. Form No. 1696 allows a beneficiary to appoint a representative for appeals or claims, similar to how the NOMNC provides instructions for appealing Medicare coverage decisions.
The Medicare Complaint Form is akin to the CMS 10123 NOMNC as both involve feedback mechanisms for individuals to express dissatisfaction with Medicare-related services. While the NOMNC involves the process to appeal a non-coverage decision, the Complaint Form addresses a broader range of issues including quality of care.
Medicare Wellness Visit Questionnaire links to the CMS 10123 NOMNC by both focusing on patient care and Medicare coverage aspects. The Questionnaire collects health information for personalized prevention plan services, similarly, the NOMNC is about informing patients regarding the specific coverage of their health services under Medicare.
Health Insurance Claim Form, CMS-1500, relates to the CMS 10123 NOMNC through their involvement in the Medicare billing and appeals process. CMS-1500 is used by healthcare providers to submit claims to Medicare, whereas the NOMNC informs beneficiaries about the discontinuation of Medicare coverage for certain services, potentially leading to billing concerns.
Dos and Don'ts
When it comes to filling out the CMS 10123 NOMNC (Notice of Medicare Non-Coverage) form, navigating the process correctly is crucial to ensure your rights and responsibilities are clear. This form serves as an official notice from Medicare or your Medicare health plan that coverage for your current services will end on a specific date, but it also outlines your right to appeal this decision. Here are some dos and don'ts to keep in mind:
What You Should Do
- Review the form carefully as soon as you receive it. Ensure you understand which services are being discontinued and the effective date of this change.
- Contact your provider for clarification if there's any part of the notice you don't understand. They can provide additional insights into why coverage is ending.
- Act promptly to appeal the decision if you believe the coverage should continue. Note the deadline for filing an appeal is no later than noon of the day before the effective date indicated on the notice.
- Seek assistance from a healthcare advocate, if needed, to help navigate the appeals process. They can offer valuable guidance and support.
- Keep detailed records of all communications regarding the NOMNC, including the appeal, to ensure you have a comprehensive paper trail.
What You Shouldn't Do
- Don't ignore the notice. Doing so could result in being financially responsible for services received after the coverage ends.
- Don't wait until the last minute to appeal. Late appeals may not be accepted, leaving you without coverage for needed services.
- Don't hesitate to ask for help from the provider, Medicare, or a Medicare health plan if you're confused about any part of the form or the appeal process.
- Don't discard any documentation related to your services, the NOMNC, or your appeal. This information could be critical in supporting your case.
- Don't sign the form without ensuring that all the information is correct and that you have been fully informed of your rights, including the right to appeal.
Effectively managing your Medicare coverage and understanding your rights when it comes to non-coverage decisions are key to navigating the health care system. Taking the right steps when you receive a CMS 10123 NOMNC form can help protect those rights and potentially extend the coverage of critical services.
Misconceptions
There are several misconceptions about the CMS 10123 NOMNC (Notice of Medicare Non-Coverage) form. Understanding these misconceptions can help patients navigate their rights more effectively. Below are nine common misunderstandings:
- The CMS 10123 NOMNC form is only for hospital stays. This is incorrect. The form applies to various types of Medicare services, including skilled nursing, home health, and outpatient therapy services, not just hospital stays.
- Patients cannot appeal the decision once they receive the CMS 10123 NOMNC form. In reality, patients have the right to an immediate, independent medical review (appeal) of the decision to end coverage of services.
- Appealing is a complex and lengthy process. While it might seem daunting, the appeal process is designed to be immediate and straightforward. Patients do not need to prepare anything in writing unless they wish to do so, and the independent reviewer will consider their medical records and relevant information.
- If you appeal, you will definitely incur costs for continued services. This is not always the case. If the appeal is successful, Medicare or the plan may continue to cover the services. Services continue during the appeal process without financial liability for the patient if they appeal timely.
- The form must be signed and returned immediately. The patient or representative must acknowledge receipt of the notice by signing it, but the crucial action is to appeal before the deadline if they disagree with the non-coverage decision.
- There is only one way to appeal. Patients have multiple avenues to appeal a non-coverage decision, including contacting the Beneficiary and Family-Centered Care Quality Improvement Organization (BFCC-QIO) listed on the form.
- Missed deadlines mean all appeal rights are lost. Even if the immediate appeal deadline is missed, patients may have other appeal rights, especially in cases involving Original Medicare versus Medicare health plans.
- Only the patient can request an appeal. Patients or their authorized representatives can request an appeal. This ensures that those unable to file an appeal personally still have access to their rights.
- The contact information on the form is only for appeals. While the primary purpose is for appeal requests, patients or their representatives can also contact the numbers provided for questions or further clarification about the notice.
Understanding the truth behind these misconceptions about the CMS 10123 NOMNC form can empower patients to better manage their care and appeal decisions they believe to be incorrect.
Key takeaways
Filling out and understanding the CMS-10123 NOMNC form is crucial for patients receiving Medicare who have been informed their service coverage will end. Below are six key takeaways to guide individuals through this process:
- Notification of Service Termination: The form serves as an official notice that the Medicare provider and/or health plan has determined that Medicare is not expected to cover the patient's current services after the specified effective date.
- Financial Responsibility: Patients may become financially responsible for services received after the effective date of coverage termination, emphasizing the importance of understanding the notice's implications.
- Right to Appeal: Patients have the right to request an immediate, independent medical review (appeal) of the decision to end coverage for the specified services. Importantly, services will continue during the appeal process.
- Appealing Process: To initiate an appeal, the patient must contact the Beneficiary and Family-Centered Care Quality Improvement Organization (BFCC-QIO) by noon the day before the effective termination date. This process is vital for those seeking to contest the termination decision.
- Outcome of the Appeal: If the independent review upholds the decision to terminate services, neither Medicare nor the plan will cover services after the effective date, underscoring the appeal's potential impact on coverage and costs.
- Missed Deadlines and Additional Rights: Patients who miss the deadline to request an immediate appeal may have other appeal rights, which vary depending on whether they have Original Medicare or are part of a Medicare health plan. Contact information for appeal processes is provided in the notice.
Understanding the CMS-10123 NOMNC form and its implications is essential for patients facing the termination of Medicare coverage for their services. Being informed about the right to appeal and following the specified process can significantly affect a patient's financial responsibility and access to necessary services.
Popular PDF Forms
Form 701-7 - Characterized by its clear guidance on how to replace a title, emphasizing proper verification and submission details.
Community Service Hours Log - Specially crafted to aid in the aggregation of service hours critical for meeting specific program criteria or graduation requirements.