Blank Express Scripts Prior Authorization PDF Template
In navigating the complexities of prescription medication coverage, the Express Scripts Prior Authorization form emerges as a crucial tool for plan members and their doctors. This document serves as a gateway for obtaining requisite approval from Express Scripts Canada® for medications that demand prior authorization, a step that often precedes reimbursement under a private drug benefit plan. The form delineates a structured process involving three primary steps: completion of Part A by the plan member, Part B by the prescribing doctor, and the final submission through either fax or mail. Despite the straightforwardness of its process, the completion and submission of this form do not inherently assure approval. Express Scripts Canada bases its approval or denial on stringent clinical criteria, primarily revolving around Health Canada's approved indications and evidence-based clinical protocols. Should there be a denial, plan members retain the right to appeal. The consequent implications of approval or denial involve not only the potential for reimbursement but also a direct communication loop with the prescribing physician. Moreover, the form extends into detailing patient information, including enrollment in patient support programs and attempts at seeking coverage under provincial plans. The intricate design of this form highlights its role in the broader healthcare framework, catering to the logistical and financial concerns intertwined with accessing prescribed medications.
Preview - Express Scripts Prior Authorization Form
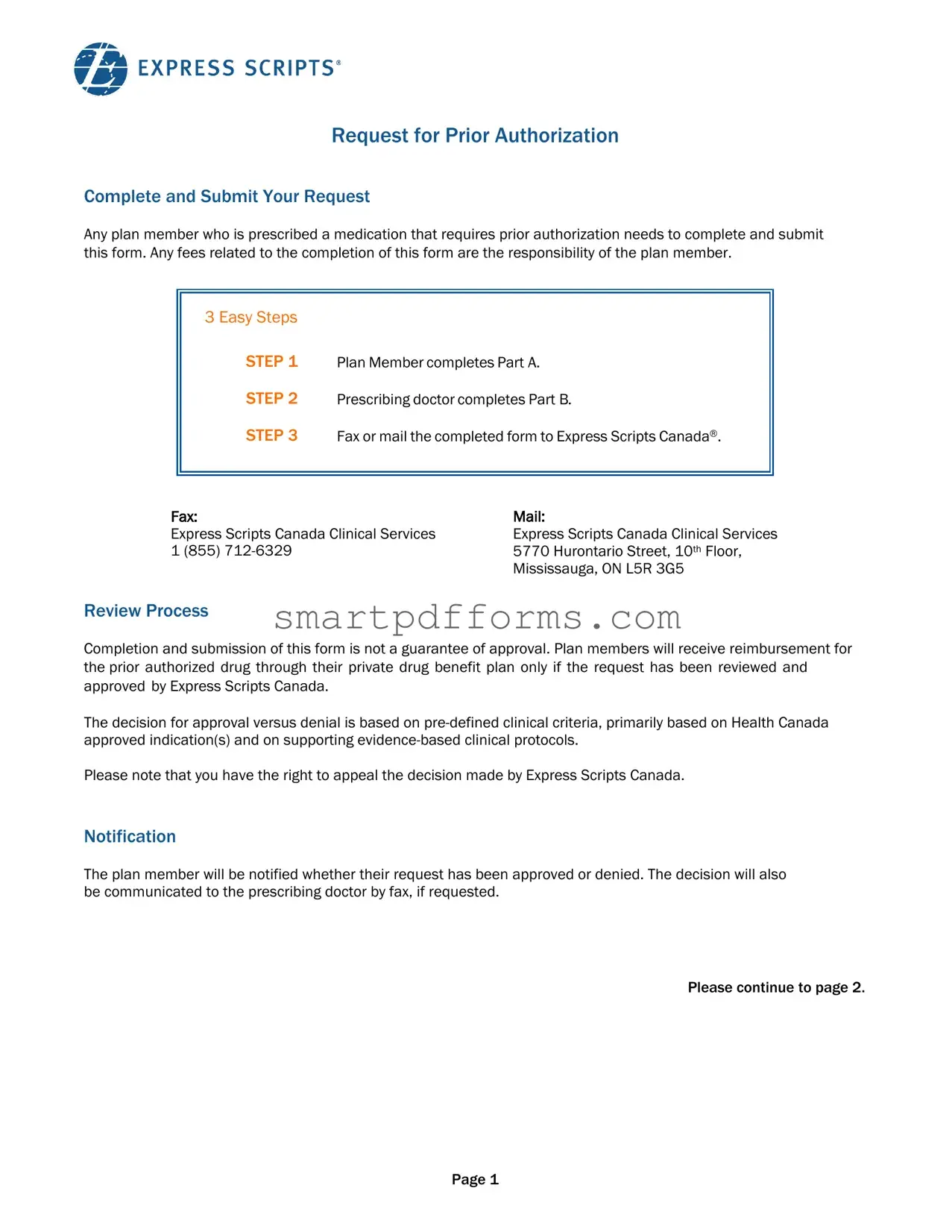
Request for Prior Authorization
Complete and Submit Your Request
Any plan member who is prescribed a medication that requires prior authorization needs to complete and submit this form. Any fees related to the completion of this form are the responsibility of the plan member.
3 Easy Steps
STEP 1 |
Plan Member completes Part A. |
STEP 2 |
Prescribing doctor completes Part B. |
STEP 3 |
Fax or mail the completed form to Express Scripts Canada®. |
Fax: |
Mail: |
Express Scripts Canada Clinical Services |
Express Scripts Canada Clinical Services |
1 (855) |
5770 Hurontario Street, 10th Floor, |
|
Mississauga, ON L5R 3G5 |
Review Process
Completion and submission of this form is not a guarantee of approval. Plan members will receive reimbursement for the prior authorized drug through their private drug benefit plan only if the request has been reviewed and approved by Express Scripts Canada.
The decision for approval versus denial is based on
Please note that you have the right to appeal the decision made by Express Scripts Canada.
Notification
The plan member will be notified whether their request has been approved or denied. The decision will also be communicated to the prescribing doctor by fax, if requested.
Please continue to page 2.
Page 1
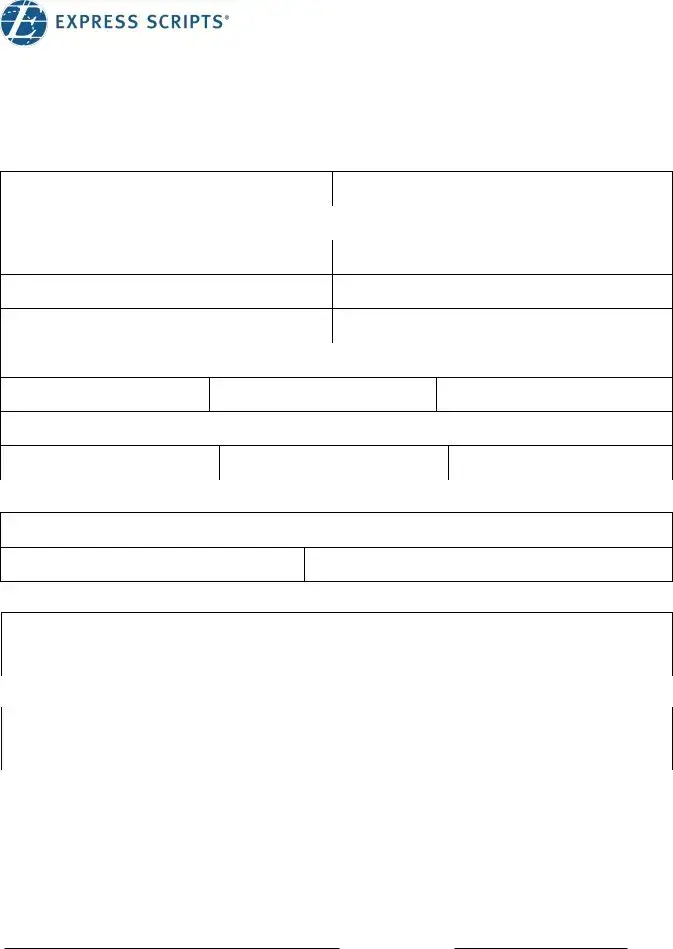
Request for Prior Authorization
Part A – Patient
Please complete this section and then take the form to your doctor for completion.
Patient information |
|
|
|
|
|
|
First Name: |
|
|
|
Last Name: |
|
|
Insurance Carrier Name/Number: |
|
|
|
|
|
|
Group number: |
|
|
|
Client ID: |
|
|
Date of Birth (DD/MM/YYYY): |
/ |
/ |
Relationship: |
□ Employee |
□ Spouse □ Dependent |
|
Language: |
□ English |
□ |
French |
Gender: |
□ Male |
□ Female |
Address: |
|
|
City: |
Province: |
Postal Code: |
Email address: |
|
|
Telephone (home): |
Telephone (cell): |
Telephone (work): |
Patient Assistance Program |
|
|
Is the patient enrolled in any patient support program? ❒ Yes |
❒ No |
|
Contact name: |
Telephone: |
|
Provincial Coverage |
|
|
Has the patient applied for reimbursement under a provincial plan? ❒ Yes ❒ No
What is the coverage decision of the drug? ❒ Approved ❒ Denied **Attach provincial decision letter**
Primary Coverage
If patient has coverage with a primary plan, has a reimbursement request been submitted? ❒ Yes ❒ No ❒ N/A What is the coverage decision of the drug? ❒ Approved ❒ Denied **Attach decision letter **
Authorization
On behalf of myself and my eligible dependents, I authorize my group benefit provider, and its agents, to exchange the personal information contained on this form. I give my consent on the understanding that the information will be used solely for purposes of administration and management of my group benefit plan. This consent shall continue so long as my dependents and I are covered by, or are claiming benefits under the present group contract, or any modification, renewal, or reinstatement thereof.
Plan Member Signature |
Date |
Page 2
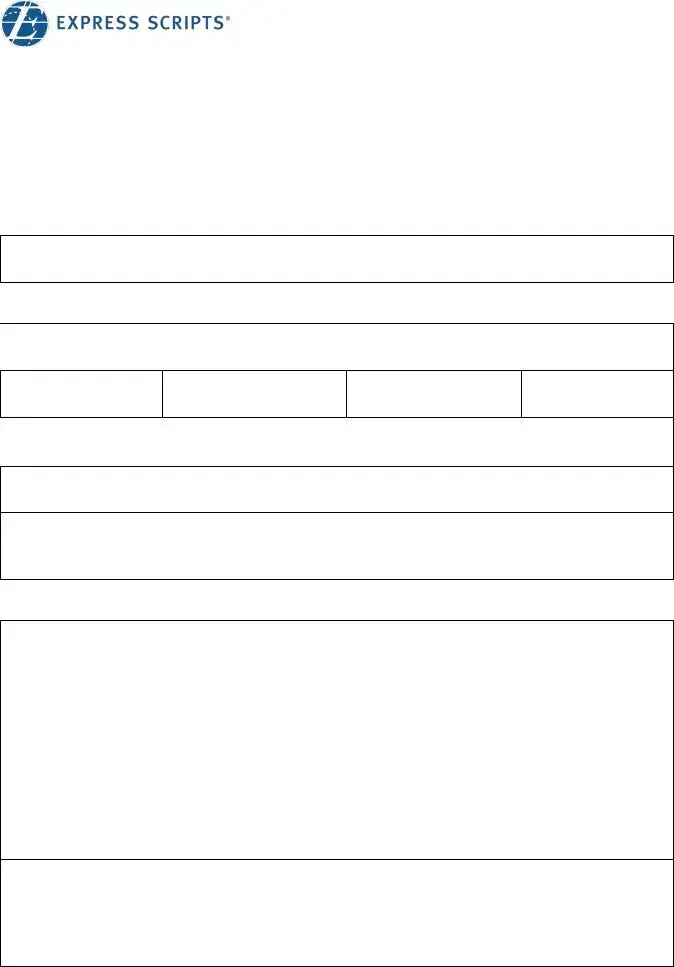
Request for Prior Authorization
Part B – Prescribing Doctor
Drugs in the Prior Authorization Program may be eligible for reimbursement only if the patient uses the drug(s) for Health Canada approved indication(s). Please provide information on your patient's medical condition and drug history, as required by the group benefit provider to reimburse this medication.
All information requested below is mandatory for the approval process, any fields left blank will result in an automatic denial. Please fill any
❒First time Prior Authorization application for this drug *Fill sections 1, 2 and 4*
❒Prior AuthorizationRenewal for this drug *Fill sections 1, 3 and 4*
SECTION 1 – DRUG REQUESTED
 Drug name:
Drug name:
Dose Administration (ex: oral, IV, etc) FrequencyDuration
 Medical condition:
Medical condition:
Will this drug be used according to its Health Canada approved indication(s)? |
❒ Yes ❒ No |
Site of drug administration: |
|
❒ Home ❒ Doctor office/Infusion clinic ❒ Hospital (outpatient) |
❒ Hospital (inpatient) |
SECTION 2 –
Any relevant information of the patient’s condition including the severity/stage/type of condition
Example: monthly frequency and duration for migraines, fibrosis status for Hepatitis C patient, lab values such as LDL and IgE levels, BMI, symptoms etc. (please do not provide genetic test information or results)
Therapies
Page 3
Request for Prior Authorization
Section 2 - Continued
Please list previously tried therapies
|
Duration of therapy |
Reason for cessation |
||
Drug |
Dosage and |
|
Inadequate/ |
Allergy/ |
|
administration |
|
||
|
From |
To |
Suboptimal |
Drug |
|
response |
Intolerance |
||
|
|
|
||
|
|
|
❒ |
❒ |
|
|
|
❒ |
❒ |
|
|
|
❒ |
❒ |
|
|
|
❒ |
❒ |
|
|
|
❒ |
❒ |
SECTION 3 – RENEWAL INFORMATION
 Date of treatment initiation:
Date of treatment initiation:
Details on clinical response to requested drug
Example: PASI/BASDAI, laboratory tests, etc. (please do not provide genetic test information or results)
If prior approval was not authorized by Express Script Canada, please attach a copy of the approval letter.
SECTION 4 – PRESCRIBER INFORMATION
Physician’s Name: |
|
Address: |
|
Tel: |
Fax: |
License No.: |
Specialty: |
Physician Signature: |
Date: |
Page 4
Form Data
| Fact Name | Detail |
|---|---|
| Form Component | Divided into two primary sections: Part A for the plan member and Part B for the prescribing doctor. |
| Authorization Requirement | Medications needing prior authorization must have the form completed and submitted by both the plan member and their prescribing doctor. |
| Submission Method | Completed forms can be faxed or mailed to Express Scripts Canada. |
| Review Outcome | Approval for medication is not guaranteed with form submission; it is contingent on review by Express Scripts Canada based on specific clinical criteria. |
| Notification Process | Plan members and, if requested, their prescribing doctors are informed via fax about the approval or denial. |
| Appeal Rights | Plan members have the right to appeal Express Scripts Canada’s decision. |
| Cost Responsibility | Fees associated with the completion of the form are the responsibility of the plan member. |
| Decision Criteria | Decisions are made based on pre-defined clinical criteria, including Health Canada approved indications. |
| Continuity of Consent | Consent for personal information exchange is provided by the plan member and remains effective as long as benefits are claimed under the contract. |
Instructions on Utilizing Express Scripts Prior Authorization
Before diving into filling out the Express Scripts Prior Authorization form, it's important to understand the process that follows its submission. Once the form is completed and submitted to Express Scripts Canada, it will undergo a review process to determine if the requested medication will be approved based on clinical criteria and guidelines. This decision is crucial as it influences whether the plan member will receive reimbursement for the prior authorized drug through their private drug benefit plan. It's also worth noting that the plan member has the right to appeal the decision made by Express Scripts Canada. They, along with their prescribing doctor, will be notified about the approval or denial of the request. This knowledge is key in setting expectations and preparing for next steps after the form is submitted.
- Complete Part A - Patient Information:
- Fill in the patient's first and last name.
- Enter the insurance carrier name/number, group number, and client ID.
- Provide the patient's date of birth in DD/MM/YYYY format.
- Indicate the relationship to the plan member (Employee, Spouse, or Dependent).
- Select the preferred language of communication (English or French).
- Identify the patient's gender (Male or Female).
- Complete the address section with the city, province, and postal code.
- Input email address and telephone numbers (home, cell, and work).
- Check if patient is enrolled in any patient assistance programs and if they have applied for provincial coverage or have primary coverage elsewhere, attaching any relevant decision letters.
- Sign the authorization statement, agreeing to the exchange of personal information for the management of the group benefit plan.
- Part B - Prescribing Doctor fills out:
- Indicate if it is a first-time prior authorization application or a renewal.
- For the drug requested, specify the drug name, dose, method of administration, frequency, and duration.
- Detail the medical condition and if the drug will be used per Health Canada approved indications.
- Specify the site of drug administration (Home, Doctor's office/Infusion clinic, Hospital outpatient, Hospital inpatient).
- For first-time applications, provide information on the patient's condition, planned therapies, and previously tried therapies along with the reasons for cessation.
- For renewals, detail the date of treatment initiation and clinical response to the requested drug.
- The prescribing doctor must then fill out their information including name, address, telephone, fax, license number, and specialty, and sign the form.
- Finally, fax or mail the completed form to Express Scripts Canada using the provided fax number or mailing address.
By following these steps meticulously, the submission process for the Express Scripts Prior Authorization form can be navigated smoothly. Attention to detail and ensuring complete and accurate information will aid in the timely review and potential approval of the medication request. Remember, this form plays a crucial role in the reimbursement process for medications requiring prior authorization, making accuracy and thoroughness paramount.
Obtain Answers on Express Scripts Prior Authorization
What is the Express Scripts Prior Authorization form?
The Express Scripts Prior Authorization form is a document required for any plan member who is prescribed a medication that needs prior authorization. This form must be filled out and submitted by following three steps: the plan member completes Part A, the prescribing doctor completes Part B, and the completed form is then faxed or mailed to Express Scripts Canada. This process is essential for obtaining coverage through a private drug benefit plan for those medications that require prior authorization.
How does the prior authorization process work?
The process involves three main steps for completion and submission. Initially, the plan member is responsible for filling out Part A of the form. Subsequently, the prescribing doctor fills out Part B, which includes detailed medical and drug history information. Finally, the completed form should be sent to Express Scripts Canada either by fax or mail. Approval of the medication is not guaranteed and depends on meeting certain clinical criteria based on Health Canada's approvals and evidence-based clinical protocols.
Who is responsible for any fees associated with completing the form?
All fees related to the completion of the Express Scripts Prior Authorization form are the responsibility of the plan member. It's important for members to be aware of potential costs that may be incurred in the process of obtaining prior authorization for prescribed medications.
What happens after the form is submitted?
Once the form is submitted, it undergoes a review process where the decision to approve or deny the request is made based on specific clinical criteria linked to the medication's approved indications and supporting evidence. Both the plan member and the prescribing doctor will be notified of the decision. If the prescribing doctor has requested it, the decision can also be communicated via fax.
Is the plan member notified about the decision?
Yes, the plan member will be notified about the outcome of their request. They will learn if their request for prior authorization has been approved or denied, ensuring transparent communication about their medication coverage eligibility.
What if the request for prior authorization is denied?
If a request is denied, the plan member has the right to appeal the decision made by Express Scripts Canada. This means that there is an avenue available for members to seek reconsideration of the decision, possibly requiring the submission of additional supporting documents or clarification on the medical necessity of the medication.
Can additional information be submitted to support the drug reimbursement request?
Yes, supplemental information supporting the drug reimbursement request is accepted and can be beneficial for the approval process. For example, for a first-time application, details on the severity or stage of the condition, previous therapies, and reasons for their cessation can be crucial. For a renewal, details on the clinical response to the requested drug are necessary. Providing comprehensive and detailed information can aid in the assessment and potential approval of the request.
Common mistakes
Not fully completing all required sections: Plan members sometimes submit forms with incomplete sections. Parts A and B must be fully completed, including patient information, drug information, medical condition, and prescribing doctor's information. Leaving any mandatory field blank or not filling non-applicable fields with 'N/A' can automatically result in a denial.
Failing to attach necessary supporting documents: Essential documents, such as the provincial decision letter if the drug has been denied or approved under a provincial plan and any previous decision letters from primary plans, are often overlooked. This oversight can impact the review process negatively.
Not providing detailed medical condition and treatment history: In Section 2, for a first-time application, and Section 3, for a renewal, it is crucial to include detailed information about the patient's medical condition, treatment history, and clinical response. A summary or lack of specifics can hinder the approval process.
Mistakes in the authorization section: Some plan members forget to sign the authorization section, which gives consent for the exchange of personal information for the purpose of processing the request. This signature is vital for the form to be processed.
Incorrect submission method: The form must be faxed or mailed to the specified Express Scripts Canada addresses. Using incorrect or outdated contact information for submission can delay or prevent the form from being processed.
Ensuring each of these common mistakes is avoided can streamline the review process, potentially leading to a faster approval decision.
Documents used along the form
When dealing with the Express Scripts Prior Authorization form, it's important to collect and prepare additional forms and documents to ensure a smooth and efficient approval process. These supplementary documents are critical because they provide a more comprehensive view of the patient’s health status, their financial situation, and the medical necessity for the prescribed medication. Below, we'll explore some of these essential documents.
- Insurance Coverage Verification Form: This document is used to confirm the patient’s current insurance coverage, policy details, and benefits eligibility, which is vital for determining the reimbursement level for the prescribed medication.
- Medical History Record: A detailed record of the patient's medical history, including previous diagnoses, treatments, and outcomes, helps in making an informed decision regarding the necessity and safety of the requested medication.
- Doctor’s Prescription Note: A formal prescription from the prescribing healthcare professional that indicates the necessity of the medication can provide the clinical rationale behind the prior authorization request.
- Laboratory Test Results: Recent lab test results that support the need for the prescribed medication are often required to prove the medical necessity as per the clinical guidelines.
- Treatment Plan: A document outlining the planned course of treatment with the requested medication, including dosage, frequency, and duration, helps in assessing its expected benefits for the patient.
- Drug Formulary: A list from the insurance provider that includes medications that are covered under the patient's health plan can be useful to determine if the requested drug is preferred, non-preferred, or not covered at all.
- Appeal Letter Template: In case of prior authorization denial, having an appeal letter template ready can expedite the process of contesting the decision, providing another opportunity for approval.
- Financial Assistance Program Application: For patients who might face financial challenges in accessing their medication, applications for financial aid or patient assistance programs can be critical.
Having these documents alongside the Express Scripts Prior Authorization form can streamline the approval process, reducing delays and increasing the chances of a favorable outcome. It's crucial for patients and healthcare providers to collaborate closely, ensuring that all required information is accurate, up-to-date, and readily available. This comprehensive approach helps in navigating the complexities of medication approvals, ultimately aiding in the patient's timely access to necessary treatments.
Similar forms
The Medicare Prior Authorization Form is similar because it also requires both patient and prescribing physician information for medication covered under Medicare. This form, like the Express Scripts Prior Authorization form, is a prerequisite for receiving specific medications not automatically covered under the plan’s formulary.
The Pharmacy Benefit Management (PBM) Prior Authorization Request Form shares similarities as it involves a request process where the physician must provide patient-specific details and medical justification for the prescribed medication, much like the Express Scripts form lays out specific requirements for prescription approval.
Medical Insurance Prior Authorization Form operates on the same basic principle - a requirement for prior approval from the insurance company before certain medications or treatments are covered. It necessitates the completion of detailed patient and medication information by the healthcare provider.
The Specialty Pharmacy Medication Request Form is similar in its requirement for specific medication requests to be fully documented and justified by the prescribing physician. This often includes patient history and the reason alternative treatments have been ineffective, parallel to the detailed clinical information requested in Express Scripts' form.
A Pre-Treatment Authorization Form used by dental or medical offices before specific treatments can begin also mirrors this form. It requires healthcare providers to submit treatment plans and justifications to insurance for coverage approval, focusing on the pre-approval process.
The Health Reimbursement Arrangement (HRA) Request Form is similar in its function to verify eligibility for reimbursement of medical expenses, including medications. This form often requires detailed medical information and anticipated costs, akin to prescription drug prior authorization forms.
The Medical Device Prior Authorization Form shares similarities in that it is designed to obtain permission before issuing certain medical devices to patients. Required information typically includes medical necessity and patient condition, much like medication prior authorization forms.
An Insurance Claim Form is similarly detailed, requiring comprehensive patient information, diagnosis, and treatment details for reimbursement purposes. While serving a slightly different end, it similarly involves thorough documentation for financial approval.
The Medication Therapy Management (MTM) Program Enrollment Form parallels the prior authorization form in its objective to tailor patient medication plans for efficacy and safety, requiring detailed patient medication history and current treatments for program eligibility.
Dos and Don'ts
When filling out the Express Scripts Prior Authorization form, there are specific steps and precautions you should take to ensure the process goes smoothly. Below are the dos and don'ts that can help guide you through this process.
Do:
- Make sure the plan member completes Part A of the form thoroughly. Double-check that all personal information fields, such as first name, last name, insurance carrier name/number, group number, client ID, date of birth, relationship, language, gender, address, email, and all telephone numbers are correctly filled.
- Ensure that the prescribing doctor fills out Part B accurately, providing detailed information about the medical condition, the requested drug, and its administration, including any previous therapies and the current Health Canada approved indication(s) for the drug.
- Attach any necessary supporting documents, such as a provincial decision letter or the primary coverage decision letter, if applicable. This will help in the evaluation of your prior authorization request.
- Review the completed form for any missing information or sections that might have been inadvertently skipped. Missing information can lead to an automatic denial of the request.
Don't:
- Leave any mandatory fields blank in either part of the form. If a section does not apply, be sure to fill it with 'N/A' instead of leaving it empty to avoid automatic denial.
- Forget to sign and date the form where required. A plan member’s signature is needed to authorize the exchange of personal information for the purposes of processing the request.
- Omit any relevant medical information or history that could support the prior authorization request, especially when detailing the medical necessity of the drug and any previous therapies tried.
- Delay in submitting the completed form to Express Scripts Canada via fax or mail. A timely submission is crucial, especially if the medication is needed urgently.
Misconceptions
There are several misconceptions about the Express Scripts Prior Authorization form that need clarification to ensure that both patients and prescribers have a clear understanding of the process. Here are six common misconceptions:
- Any fees associated with completing the form are charged by Express Scripts Canada. In reality, any fees related to the completion of the form are the responsibility of the plan member. This can often be misunderstood, implying that Express Scripts or the prescribing doctor charges additional fees for the authorization process.
- Submitting the form guarantees approval. Just because the form is completed and submitted doesn’t guarantee that the medication will be approved for coverage. The decision is based on pre-defined clinical criteria, primarily focusing on Health Canada approved indications and evidence-based protocols. This is a critical piece of information as it sets realistic expectations for plan members.
- The process is lengthy and complicated. The form outlines three clear steps for submission, suggesting an effort to make the process as straightforward as possible. While it does involve multiple parties—the plan member, the prescribing doctor, and Express Scripts Canada—the steps are designed to be easy to follow.
- There is no recourse if a request is denied. Plan members have the right to appeal the decision made by Express Scripts Canada. This is an important right that ensures plan members are not left without options if their initial request is not approved.
- Prior Authorization is only for rare or expensive drugs. While it's common for expensive or specialty medications to require prior authorization, the criteria include a range of factors, including safety concerns and potential for misuse, not solely the cost of the medication.
- Doctors are solely responsible for the submission process. The process begins with the plan member who must complete the first part of the form before taking it to their doctor. The prescribing doctor completes the second part and then the form is faxed or mailed to Express Scripts Canada by either the doctor or the plan member. Responsibility is shared between the patient and the prescribing physician, highlighting a collaborative aspect of the process.
Understanding these misconceptions can help demystify the prior authorization process with Express Scripts Canada, making it easier for patients and healthcare providers to navigate it effectively.
Key takeaways
Filling out and using the Express Scripts Prior Authorization form requires a thorough understanding to ensure that medications are covered under your plan. Here are key takeaways to guide plan members and prescribing doctors through the process:
- Step-by-Step Completion: The form is divided into a clear, three-step process. Initially, the plan member is responsible for completing Part A. Subsequently, the prescribing doctor must complete Part B. Finally, the completed form should be sent to Express Scripts Canada either by fax or mail. Understanding each part's requirements is crucial for a successful submission.
- Financial Responsibility: It is important for plan members to note that any fees associated with the completion of this form fall under their responsibility. This information sets clear expectations and helps plan members prepare for any potential costs involved in the process.
- Approval is Not Guaranteed: Submission of the prior authorization form does not automatically result in approval. This decision is made based on pre-defined clinical criteria and Health Canada approved indications. Being aware of this can help manage expectations and prepare for alternative steps if the request is denied.
- Right to Appeal: If a request is denied, plan members have the right to appeal Express Scripts Canada's decision. This is a critical point for plan members and prescribing doctors to understand, as it provides an additional course of action in the pursuit of gaining approval for necessary medications.
It is imperative for both plan members and prescribing doctors to pay close attention to detail when completing the form, and to comply with all specified requirements and steps. Doing so maximizes the chances of approval and ensures that the process proceeds as smoothly as possible.
Popular PDF Forms
Hcfa 487 - Helps healthcare providers to maintain an up-to-date and accurate record of patient treatment plans.
Employee Profile Examples - A crucial document for businesses to fill, detailing the racial, gender, and salary composition of their workforce for internal and external review.