Blank Hcfa 487 PDF Template
Delving into the realm of healthcare documentation, the HCFA-487 form emerges as a critical piece, underpinning the meticulous processes that fuse medical treatment plans with the financial scaffolding provided by health services. Administered by the Department of Health and Human Services, this form carries the stamp of approval from the Health Care Financing Administration, now known as the Centers for Medicare & Medicaid Services (CMS), highlighting its pivotal role in the American healthcare system. The form serves as an addendum to a patient's treatment plan, offering a structured means for updating medical information within a specific certification period. It meticulously records details ranging from the patient's Health Insurance (HI) Claim Number to provider names, alongside the dates marking the start and end of service, underscoring the form's significance in maintaining the continuum of care. Moreover, it garners importance from its requirement for a physician's signature, ensuring that any amendment or medical update adheres to a medically authorized framework. This condensed yet comprehensive form encapsulates the dynamic interaction between care providers and the insurance apparatus, facilitating a fluid exchange of vital healthcare information.
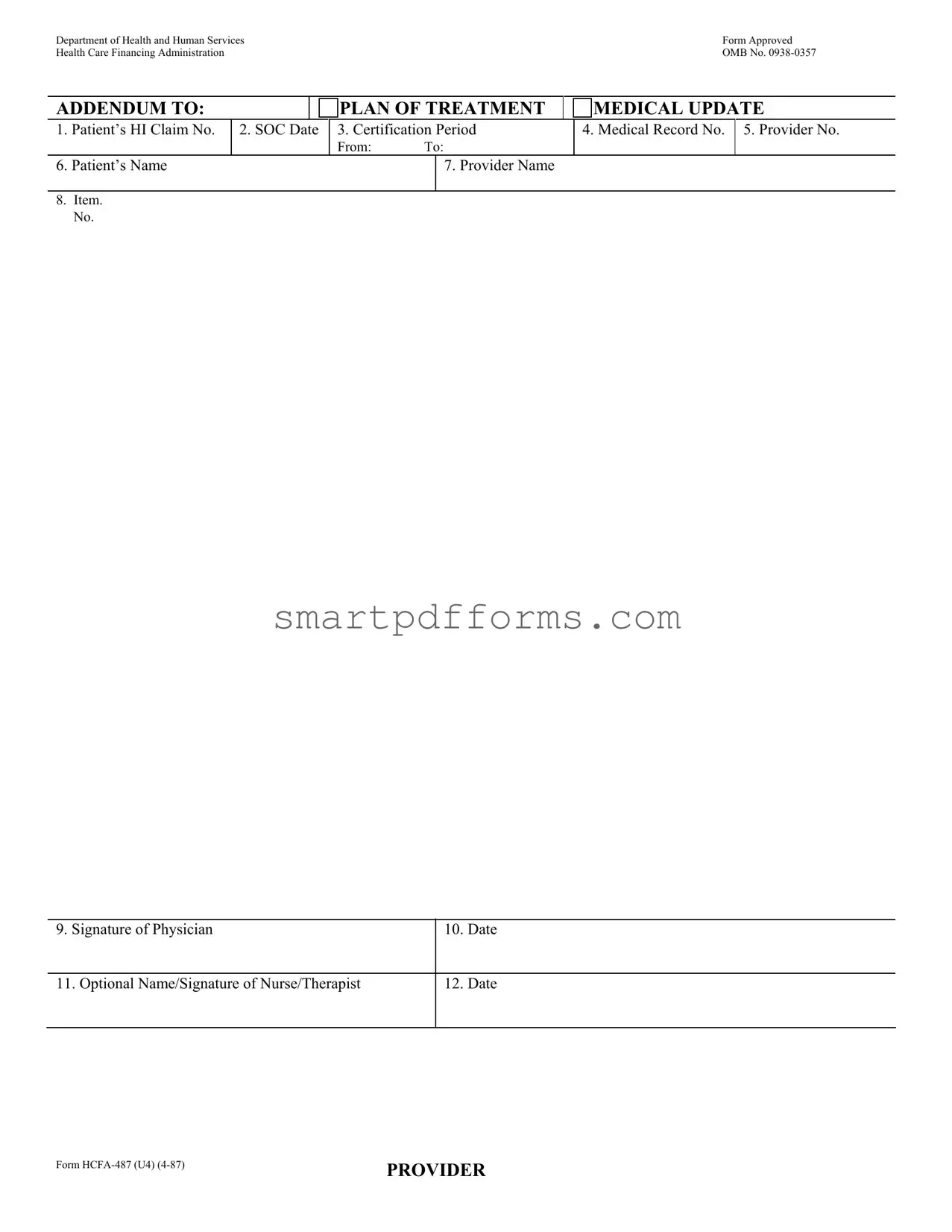
Preview - Hcfa 487 Form
Department of Health and Human Services |
Form Approved |
Health Care Financing Administration |
OMB No. |
ADDENDUM TO: |
|
|
PLAN OF TREATMENT |
|
MEDICAL UPDATE |
||||
|
|
|
|
|
|
|
|
|
|
1. |
Patient’s HI Claim No. |
2. SOC Date |
3. Certification Period |
|
4. Medical Record No. |
5. Provider No. |
|||
|
|
|
|
From: |
To: |
|
|
|
|
6. |
Patient’s Name |
|
|
|
|
7. Provider Name |
|
|
|
|
|
|
|
|
|
|
|
|
|
8.Item.
No.
9. Signature of Physician
10. Date
11. Optional Name/Signature of Nurse/Therapist
12. Date
Form
PROVIDER
Form Data
| Fact Name | Description |
|---|---|
| Form Identifier | HCFA-487 (U4) (4-87) |
| Form Purpose | Addendum to Plan of Treatment Medical Update |
| Approval Authority | Department of Health and Human Services, Health Care Financing Administration, OMB No. 0938-0357 |
| Key Contents | Includes patient's HI Claim No., SOC Date, Certification Period, Medical Record No., Provider No., Patient's and Provider's Name, Item No., Physician's and Nurse/Therapist's Signature and Date. |
| Governing Law(s) | Specific governing laws may vary by state; this form is approved at a federal level by the Department of Health and Human Services and the Health Care Financing Administration. |
Instructions on Utilizing Hcfa 487
Once the HCFA 487 form is accurately completed, it serves as a critical step in ensuring the patient's plan of treatment and medical updates are properly documented and aligned with health care procedures. This form is mostly used by healthcare providers for administrative purposes. Following the correct steps to fill out the form ensures that all necessary information is conveyed accurately to the Department of Health and Human Services and the Health Care Financing Administration. Below are the detailed steps to fill out the form efficiently.
- Enter the patient’s Health Insurance Claim Number in the space provided for Patient’s HI Claim No.
- Input the Start of Care (SOC) Date in the designated area.
- For the Certification Period, include both the start and end dates in the corresponding fields.
- Fill in the Medical Record No. that pertains to the patient’s medical records.
- Insert the Provider No. which is the unique identifier for the healthcare provider.
- Write the Patient’s Name clearly to avoid any confusion regarding the identity of the patient.
- Under Provider Name, put the name of the healthcare provider completing the form.
- In the Item No. field, specify the number associated with the update or plan of treatment being documented, if applicable.
- Have the attending Physician’s Signature in the assigned space to certify the accuracy of the information provided.
- Record the Date next to the physician’s signature to indicate when the form was completed.
- If applicable, include the Optional Name/Signature of Nurse/Therapist who assisted in the plan of treatment or medical update.
- Next to the optional signature, ensure the Date is also filled to confirm when the nurse or therapist reviewed or contributed to the form.
Once all the required information has been filled out, it is crucial to review the form for accuracy to prevent any potential issues. After review, the form should be submitted to the designated department or authority as per the healthcare provider's standard operating procedures. This completed document plays a crucial role in the patient's healthcare records, ensuring continuity of care and proper healthcare administration.
Obtain Answers on Hcfa 487
What is the HCFA-487 form used for?
The HCFA-487 form, issued by the Department of Health and Human Services and approved by the Health Care Financing Administration, now known as the Centers for Medicare & Medicaid Services (CMS), serves a specific purpose within the medical field. This form acts as an addendum to a patient's plan of treatment, providing a necessary medical update. It is primarily used in settings where continuous patient care is provided, such as home health agencies. Through the HCFA-487, providers can document changes or updates in a patient’s treatment plan, ensuring that the care delivered is aligned with the patient's current health status and needs. Moreover, it facilitates communication between healthcare professionals involved in the patient's care, ensuring that everyone has the latest information regarding the patient's treatment plan.
Who needs to complete the HCFA-487 form?
The completion of the HCFA-487 form involves several key participants in the patient's care team. Primarily, the patient’s physician is responsible for filling out most of the form, including updating the patient's plan of treatment. The physician's signature is crucial as it validates the changes made to the treatment plan. Furthermore, there is an optional section for the name and signature of a nurse or therapist involved in the patient's care. This inclusion recognizes the interdisciplinary approach often required in managing a patient's treatment across different care settings. The form ensures that there is a documented consensus among the healthcare professionals involved regarding the patient’s current care plan.
How is the HCFA-487 form submitted?
The process of submitting the HCFA-487 form typically adheres to the protocols set by Medicare, Medicaid, or the respective healthcare provider's internal procedures. Once completed and signed by the necessary medical professionals, the form should be submitted to the healthcare facility's administration or directly to the insurance provider, depending on the established workflow. This ensures that the patient's records are updated promptly, and any relevant changes are communicated to parties responsible for funding or overseeing the patient’s care. In the age of digital records, some institutions may also accept electronic submissions, streamlining the process and ensuring the information is quickly integrated into the patient’s electronic health record (EHR).
What information is mandatory on the HCFA-487 form?
The HCFA-487 form requires several key pieces of information to be filled out accurately to be considered valid. Firstly, the patient's Health Insurance (HI) Claim Number is essential for identifying the patient within the healthcare system and ensuring that the update is properly linked to the right individual. The Start of Care (SOC) date, Certification Period, Medical Record Number, and Provider Number must also be included to give context to the treatment period and identify the healthcare provider. Additionally, both the patient's and provider's names are mandatory, facilitating the connection between the treatment plan and the individuals involved. Most importantly, the physician's signature is required to validate the updates made to the patient's treatment plan. The optional section for a nurse or therapist to sign and date the form also indicates the collaborative effort in the patient’s care, though not strictly mandatory.
Common mistakes
Filling out the HCFA-487 form, an essential document for healthcare professionals in communicating treatment plans and medical updates to the Health Care Financing Administration, can sometimes be more complicated than expected. Here are six common mistakes people often make on this form:
- Incorrect Patient Information: A simple typo or error in the patient's Health Insurance Claim Number or name can lead to significant processing delays. Each piece of patient information must match the records exactly.
- Leaving Dates Blank: The SOC (Start of Care) Date, Certification Period, and the form's completion date are crucial for timely processing. Forgetting to fill these in can cause unnecessary setbacks.
- Incomplete Provider Details: The Provider Number and Provider Name must be filled out completely and accurately. Since this form acts as an addendum to a plan of treatment, correct identification of the healthcare provider is essential for the form to be processed correctly.
- Missing Signatures: Signature fields, particularly that of the physician (Item No. 9) and, if applicable, the nurse or therapist (Item No. 11), are often overlooked. Without these signatures, the form lacks the necessary verification to be considered valid.
- Ignoring Optional Sections: Although Item No. 11 is labeled as "optional," providing the name and signature of a nurse or therapist can sometimes make a difference, especially in cases where further clarification on the treatment plan might be required.
- Misunderstanding the Form's Purpose: Sometimes people confuse the HCFA-487 form with other healthcare documentation. This form is specifically for updating or adding to a patient's treatment plan, and its proper use is vital for ensuring that the patient's care is appropriately documented and billed.
Correctly filling out the HCFA-487 form plays a crucial role in healthcare administration, ensuring that patients receive the care they need while allowing for smooth operational processes between healthcare providers and insurance administrations. By steering clear of these common pitfalls, one can help facilitate better healthcare outcomes and more efficient administrative procedures.
Documents used along the form
The HCFA 487 form, integral to the process of updating a patient's treatment plan within the realm of services funded by the Health and Human Services, marks a vital piece in maintaining accurate and current medical records for those under care. However, to ensure comprehensive care management and regulatory compliance, several other forms and documents are often utilized in conjunction alongside the HCFA 487 form. These documents not only enhance the clarity of the patient's medical journey but also ensure that all aspects of their care are meticulously documented and readily available for review by healthcare professionals and relevant administrative bodies.
- HCFA-485 (Home Health Certification and Plan of Care): This form outlines the need for home health services, certifying that the patient requires such care and detailing what services are to be provided, goals of treatment, and the plan of care.
- HCFA-486 (Home Health Update or Revision): Complementary to the HCFA-487, this document is used for updating or revising the plan of care for patients receiving home health services, ensuring that changes in health status or treatment goals are accurately recorded.
- OASIS (Outcome and Assessment Information Set): As a comprehensive assessment tool for home health patients, OASIS is crucial for ensuring that the patient's needs are thoroughly evaluated and documented, directly affecting the plan of care and treatment updates.
- Medication Profile: This document lists all medications a patient is taking, including dosages and frequencies, playing a crucial role in monitoring for drug interactions and ensuring safe medication administration.
- Advance Directive Forms: Documents such as living wills and healthcare proxies, which outline a patient's wishes regarding life-sustaining treatment, are essential for respecting patient autonomy and making informed care decisions.
- Care Coordination Notes: These notes detail any coordination activities among healthcare providers, ensuring that all members of the healthcare team are informed of the patient's status, plan of care, and any changes thereof.
- Nursing Notes/Progress Notes: Regular entries made by nurses and therapists provide ongoing insights into the patient's condition, response to treatment, and any adjustments made to the care plan, enhancing continuity of care.
- Discharge Planning Forms: When a patient's treatment progresses to a point where they can be discharged, these forms outline post-discharge care, services needed, and any follow-up appointments, ensuring a smooth transition from one level of care to another.
Together, these documents form a coherent ecosystem of care documentation, ensuring that every aspect of the patient’s healthcare journey is accurately tracked and managed. They serve not only as a means of communication among healthcare providers but also as a safeguard for patients, ensuring their treatment is aligned with established goals and regulatory requirements. The careful coordination and completion of these forms, along with the HCFA 487, are essential components in delivering high-quality, patient-centered healthcare.
Similar forms
The CMS-485, Home Health Certification and Plan of Care form, is similar to the HCFA-487 form in that it is also used in the home health setting. Both forms are integral for the planning and certification of home health care services, requiring information such as patient identification, medical provider details, and care plans. The CMS-485 specifically focuses on the certification of home health services and the establishment of a detailed care plan.
The UB-04 (CMS-1450) form bears resemblance to the HCFA-487 form as both are utilized within the healthcare billing process. Where the HCFA-487 form adds to the clinical documentation supporting the necessity of medical care, the UB-04 form is used by hospitals and other healthcare facilities to submit claims to payers. It covers a broad spectrum of patient and provider information, service dates, and billing codes.
HCFA-1500 (now known as CMS-1500) is another document that is comparable to the HCFA-487 form, primarily because it is also used for billing purposes. Unlike HCFA-487, which is specific to treatment updates and certification in a home health scenario, CMS-1500 is a standard claim form used by non-institutional providers and suppliers to bill Medicare Part B services, including physician services, and sometimes Medicaid.
The OASIS (Outcome and Assessment Information Set) document is related to the HCFA-487 form in its application within home health care. While the HCFA-487 form provides a medical update or addition to a plan of treatment, the OASIS is used to gather patient data that measures the outcomes of home health care. Both documents are essential for the evaluation and continuation of care plans in a home health context.
The Plan of Treatment (POT) form closely aligns with the HCFA-487 form by serving a key role in detailing a patient's care plan. Both documents are used by healthcare providers to outline the medical services and interventions prescribed to a patient. The POT form, like the HCFA-487, serves as a foundational document that guides the direction of patient care within various healthcare settings.
The Medication Administration Record (MAR) shares similarities with the HCFA-487 form in that it is used within healthcare to document specifics of patient care. Whereas the HCFA-487 form focuses on the broader treatment plan and updates, the MAR is a more specific log detailing when and what medications have been administered to a patient, ensuring accuracy and adherence to a prescribed treatment regime.
The Interdisciplinary Team Meeting (IDT) Notes can be compared to the HCFA-487 form as both are used within the healthcare planning process. The IDT Notes document the discussions and decisions made by the healthcare team regarding a patient’s treatment plan. Like the HCFA-487, it is a collaborative tool that supports the delivery of coordinated and efficient care.
Dos and Don'ts
When you fill out the HCFA 487 form, there are specific steps you should follow to ensure that the process is completed correctly. This will help in submitting a clear and error-free document to the Health and Human Services Department.
Things you should do:
- Read all instructions carefully before beginning to fill out the form. This ensures you understand the requirements and provide all necessary information accurately.
- Double-check the Patient’s HI Claim No. and Medical Record No. for accuracy. Mistakes in these numbers can lead to processing delays or the rejection of the form.
- Make sure that the certification period is indicated clearly, including both the start and end dates. This is crucial for the processing of the form and for ensuring that coverage is accurately defined.
- Ensure the signature of the physician and the date are included. Without this, the form is considered incomplete and will not be processed.
Things you shouldn't do:
- Avoid leaving any sections blank. If a section does not apply, indicate with “N/A” (Not Applicable) instead of leaving it empty. This helps in confirming that no information was overlooked.
- Do not use unclear handwriting. Since the information needs to be legible to various individuals who will handle the processing, always fill out the form in clear, legible handwriting or, if possible, type the information.
- Don't forget to review the form for errors or omissions before submission. Taking a moment to double-check can prevent unnecessary delays.
- Avoid excluding the optional name/signature of the nurse/therapist if their input is part of the treatment or medical update. Their acknowledgment can be essential for a comprehensive understanding of the patient's care.
By following these guidelines, you can ensure that the HCFA 487 form is filled out completely and accurately, aiding in the efficient processing of your submission.
Misconceptions
When it comes to healthcare paperwork, the HCFA 487 form is essential but often misunderstood. Let's clear up some common misconceptions:
- Misconception 1: The HCFA 487 form is only for hospital use.
This form isn't just for hospitals. It's a vital document for various healthcare providers that offer treatment plans, needing to update medical information for patients. It's designed to ensure continuous, coordinated care across different medical professionals.
- Misconception 2: It's a consent form.
The HCFA 487 form is often confused with consent forms. However, its primary purpose is not to get consent but to provide an update or addendum to a patient's plan of treatment. It ensures that all involved healthcare providers are on the same page regarding the patient's care.
- Misconception 3: Only physicians can complete it.
While it's true that a physician's signature is required, the form also acknowledges the role of nurses and therapists. There's a specific section for the optional name and signature of a nurse or therapist, recognizing their crucial role in the patient's treatment and care coordination.
- Misconception 4: It's a one-time form.
Many assume that once filled out, the HCFA 487 form is set in stone. In reality, healthcare is dynamic, and patient needs may change. This form can be updated as treatment evolves, ensuring that medical records accurately reflect the current plan of care.
Understanding the HCFA 487 form is key to ensuring seamless communication and coordination among healthcare providers. By dispelling these misconceptions, providers can better utilize this form to support their patients' health and treatment outcomes.
Key takeaways
Filling out the HCFA 487 form is an essential administrative process for healthcare providers who are managing patients receiving certain types of medical services. Understanding the key components and purposes of this form can streamline the process and ensure proper documentation and compliance with health care standards. Here are six key takeaways regarding the HCFA 487 form:
- The HCFA 487 form is an addendum to the plan of treatment, focusing on medical updates. It is designed to provide updated information about a patient's treatment plan to the Department of Health and Human Services and the Health Care Financing Administration.
- Information required on this form includes the patient's Health Insurance Claim Number (HICN), Start of Care (SOC) date, certification period, medical record number, provider number, patient's name, and provider's name. These details are crucial for associating the form with the correct patient and treatment plan.
- The form requires the signature of the physician overseeing the treatment, ensuring that any changes or updates to the plan of treatment are medically reviewed and authorized. This measure ensures accountability and adherence to prescribed medical care.
- There is also an option for a nurse or therapist to sign the form, alongside their name. This inclusion acknowledges the multidisciplinary approach to patient care and allows relevant medical professionals involved in the patient’s care to provide updates as necessary.
- The form includes specific dates, such as the certification period and the date of the physician's (and when applicable, the nurse's or therapist's) signature. These dates are essential for documenting when the medical update was made and ensuring that the patient's care plan is reviewed and updated within appropriate timeframes.
- Completing the HCFA 487 form accurately and in a timely manner is essential for compliance with healthcare regulations and to ensure that patients receive the proper care and services they need. It helps in maintaining clear and updated records of treatment plans, facilitating better communication among healthcare providers.
In summary, the HCFA 487 form is a critical document for healthcare providers, enabling them to update patient treatment plans and ensuring that all related medical professionals are informed of any changes. Proper completion and submission of this form not only comply with regulatory requirements but also support the delivery of high-quality, coordinated patient care.
Popular PDF Forms
Social Security Income Tax Form - Used by Social Security beneficiaries to inform on their residence or expected residence outside the U.S.
Lost License Plate Ct - Form DMW 45 A underscores the necessity of having liability insurance as per state law.
Wells Fargo Power of Attorney Form - The form necessitates the Principal's (account owner) signature be notarized to verify identity and intent.