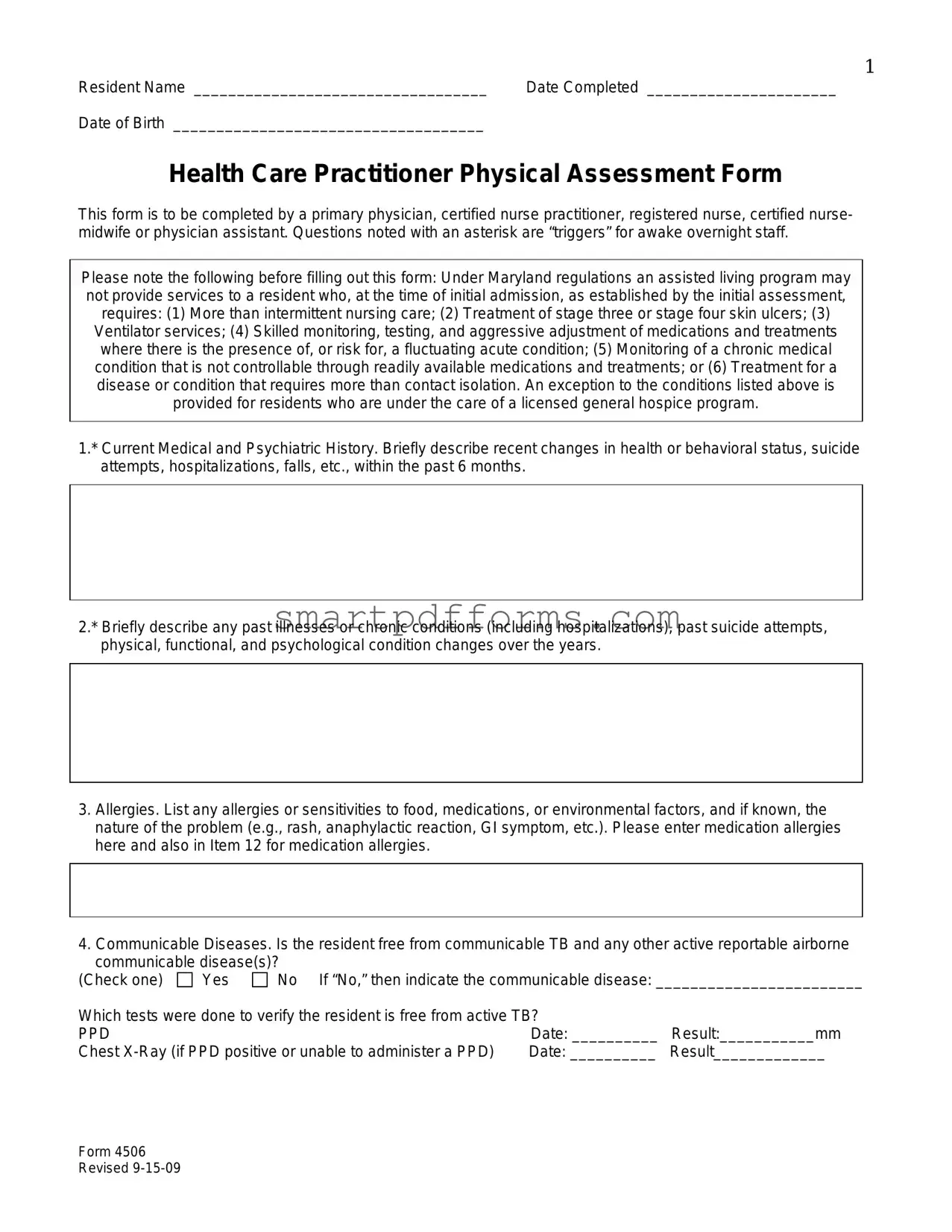
Blank Health Practitioner Physical Assessment PDF Template
In the landscape of assisted living and healthcare management, the Health Practitioner Physical Assessment form stands as a cornerstone document, designed to ensure a comprehensive evaluation of residents' medical and psychological well-being. This detailed assessment, mandatory to be filled out by a wide range of healthcare professionals, including primary physicians and certified nurse practitioners among others, plays a pivotal role in tailoring individualized care plans. It meticulously records not only the current medical and psychiatric status of residents, including recent health changes and allergy information, but also delves into their past health history, substance use, and risk factors for falls and injuries. Moreover, the form addresses the resident's cognitive and behavioral status, nutritional status, ability to self-administer medications, and even nuances like sensory impairments and skin conditions. This rigorous documentation process, guided by Maryland's regulatory framework, ensures that assisted living programs are well-informed about the healthcare needs of their residents, thus barring the admission of individuals requiring more intensive, specialized care unless under a general hospice program. The form not only facilitates a comprehensive health evaluation but also enforces critical checks ensuring the exclusion of individuals with conditions that exceed the care capabilities of assisted living facilities, thereby safeguarding both the individual resident and the community at large.
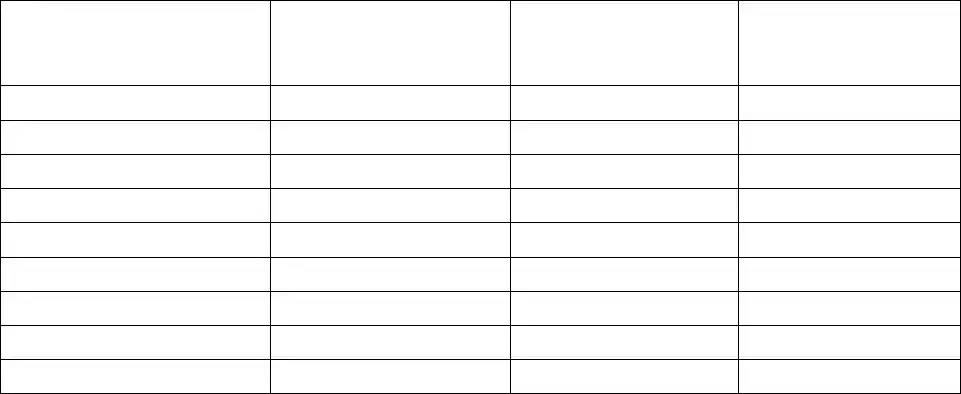
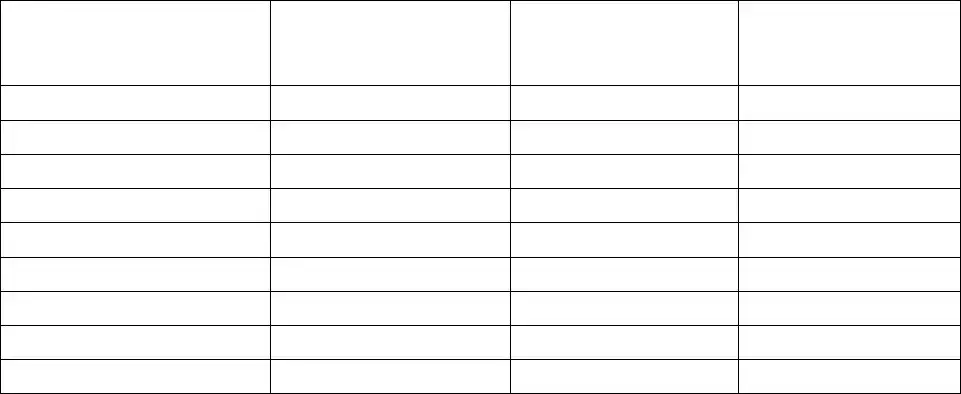
Preview - Health Practitioner Physical Assessment Form
1
Resident Name __________________________________ |
Date Completed ______________________ |
Date of Birth ____________________________________ |
|
Health Care Practitioner Physical Assessment Form
This form is to be completed by a primary physician, certified nurse practitioner, registered nurse, certified nurse- midwife or physician assistant. Questions noted with an asterisk are “triggers” for awake overnight staff.
Please note the following before filling out this form: Under Maryland regulations an assisted living program may not provide services to a resident who, at the time of initial admission, as established by the initial assessment, requires: (1) More than intermittent nursing care; (2) Treatment of stage three or stage four skin ulcers; (3) Ventilator services; (4) Skilled monitoring, testing, and aggressive adjustment of medications and treatments where there is the presence of, or risk for, a fluctuating acute condition; (5) Monitoring of a chronic medical condition that is not controllable through readily available medications and treatments; or (6) Treatment for a disease or condition that requires more than contact isolation. An exception to the conditions listed above is provided for residents who are under the care of a licensed general hospice program.
1.* Current Medical and Psychiatric History. Briefly describe recent changes in health or behavioral status, suicide attempts, hospitalizations, falls, etc., within the past 6 months.
2.* Briefly describe any past illnesses or chronic conditions (including hospitalizations), past suicide attempts, physical, functional, and psychological condition changes over the years.
3.Allergies. List any allergies or sensitivities to food, medications, or environmental factors, and if known, the nature of the problem (e.g., rash, anaphylactic reaction, GI symptom, etc.). Please enter medication allergies here and also in Item 12 for medication allergies.
4.Communicable Diseases. Is the resident free from communicable TB and any other active reportable airborne communicable disease(s)?
(Check one) |
Yes |
No If “No,” then indicate the communicable disease: ________________________ |
||
Which tests were done to verify the resident is free from active TB? |
|
|||
PPD |
|
|
Date: __________ |
Result:___________mm |
Chest |
Date: __________ |
Result_____________ |
||
Form 4506 Revised
2
Resident Name __________________________________ |
Date Completed ______________________ |
Date of Birth ____________________________________ |
|
5.History. Does the resident have a history or current problem related to abuse of prescription,
(a)Substance: OTC,
1. |
Recent (within the last 6 months) |
Yes |
No |
2. |
History |
Yes |
No |
(b)Abuse or misuse of prescription medication or herbal supplements
1. |
Currently |
Yes |
No |
2. |
Recent (within the last 6 months) |
Yes |
No |
(c)History of
1. |
Currently |
Yes |
No |
2. |
Recent (within the last 6 months) |
Yes |
No |
(d)Describe misuse or abuse: _________________________________________________________
____________________________________________________________________________________
6.* Risk factors for falls and injury. Identify any conditions about this resident that increase his/her risk of falling or
injury (check all that apply): 
 orthostatic hypotension
orthostatic hypotension 
 osteoporosis
osteoporosis 
 gait problem
gait problem 
 impaired
impaired
balance  confusion
confusion  Parkinsonism
Parkinsonism  foot deformity
foot deformity  pain
pain  assistive devices
assistive devices  other (explain)
other (explain)
__________________________________________________________________________________________ |
|
||||||||||||||||
7.* Skin condition(s). Identify any history of or current ulcers, rashes, or skin tears with any standing treatment |
|
||||||||||||||||
orders. _________________________________________________________________________________ |
|
||||||||||||||||
__________________________________________________________________________________________ |
|
||||||||||||||||
8.* Sensory impairments affecting functioning. (Check all that apply.) |
|
|
|
|
|
|
|
||||||||||
(a) Hearing: |
Left ear: |
|
|
|
Adequate |
|
Poor |
Deaf |
|
Uses corrective aid |
|
|
|
||||
(b) Vision: |
Right ear: |
|
|
|
Adequate |
|
Poor |
Deaf |
|
Uses corrective aid |
|
|
|
||||
Adequate |
Poor |
|
Uses corrective lenses |
Blind (check all that apply) - |
R |
L |
|||||||||||
(c) Temperature Sensitivity: |
|
|
|
Normal |
Decreased sensation to: |
Heat |
Cold |
|
|
|
|||||||
9. Current Nutritional Status. |
Height |
|
|
inches |
|
|
Weight |
|
lbs. |
|
|
|
|
|
|||
(a) Any weight change (gain or loss) |
in the |
past 6 months? |
|
|
|
|
|
Yes |
No |
|
|
||||||
(b) How much weight change? |
|
|
lbs. in the past |
|
months (check one) |
Gain |
Loss |
|
|
||||||||
(c) Monitoring necessary? (Check one.) |
|
|
|
|
|
|
|
Yes |
No |
|
|
||||||
If items (a), (b), or (c) are checked, explain how and at what frequency monitoring is to occur: ___________ |
|
||||||||||||||||
__________________________________________________________________________________________ |
|
||||||||||||||||
(d) Is there evidence of malnutrition or risk for undernutrition? |
|
|
|
Yes |
No |
|
|
||||||||||
(e)* Is there evidence of dehydration or a risk for dehydration? |
|
|
|
Yes |
No |
|
|
||||||||||
(f) Monitoring of nutrition or hydration status necessary? |
|
|
|
|
|
Yes |
No |
|
|
||||||||
If items (d) or (e) are checked, explain how and at what frequency monitoring is to occur: _______________
__________________________________________________________________________________________
(g)Does the resident have medical or dental conditions affecting: (Check all that apply)
 Chewing
Chewing  Swallowing
Swallowing  Eating
Eating  Pocketing food
Pocketing food  Tube feeding
Tube feeding
(h)Note any special therapeutic diet (e.g., sodium restricted, renal, calorie, or no concentrated sweets restricted): _________________________________________________________________________________
__________________________________________________________________________________________
(i)Modified consistency (e.g., pureed, mechanical soft, or thickened liquids): _________________________
__________________________________________________________________________________________
(j) Is there a need for assistive devices with eating (If yes, check all that apply): |
Yes |
No |
||
Weighted spoon or built up fork |
Plate guard |
Special cup/glass |
|
|
(k) Monitoring necessary? (Check one.) |
|
|
Yes |
No |
If items (g), (h), or (i) are checked, please explain how and at what frequency monitoring is to occur:
__________________________________________________________________________________________
Form 4506 Revised
3
Resident Name __________________________________ |
Date Completed ______________________ |
Date of Birth ____________________________________ |
|
10.* Cognitive/Behavioral Status.
(a)* Is there evidence of dementia? (Check one.)
(b) Has the resident undergone an evaluation for dementia? (c)* Diagnosis (cause(s) of dementia): 

(d)
Yes |
No |
Yes |
No |

 Other
Other
10(e)* Instructions for the following items: For each item, circle the appropriate level of frequency or intensity, depending on the item. Use the “Comments” column to provide any relevant details.
Item 10(e) |
A |
B* |
C* |
|
D* |
Comments |
|
|
|
Cognition |
|
|
|
I. Disorientation |
Never |
Occasional |
Regular |
|
Continuous |
|
II. Impaired recall |
Never |
Occasional |
Regular |
|
Continuous |
|
(recent/distant events) |
|
|
||||
|
|
|
|
|
|
|
III. Impaired judgment |
Never |
Occasional |
Regular |
|
Continuous |
|
IV. Hallucinations |
Never |
Occasional |
Regular |
|
Continuous |
|
|
|
|
|
|
|
|
V. Delusions |
Never |
Occasional |
Regular |
|
Continuous |
|
|
|
|
Communication |
|
|
|
VI. Receptive/expressive |
Never |
Occasional |
Regular |
|
Continuous |
|
aphasia |
|
|
||||
|
|
|
|
|
|
|
|
|
Mood |
and Emotions |
|
|
|
VII. Anxiety |
Never |
Occasional |
Regular |
|
Continuous |
|
|
|
|
|
|
|
|
VIII. Depression |
Never |
Occasional |
Regular |
|
Continuous |
|
|
|
|
Behaviors |
|
|
|
IX. Unsafe behaviors |
Never |
Occasional |
Regular |
|
Continuous |
|
|
|
|
|
|
|
|
X. Dangerous to self or |
Never |
Occasional |
Regular |
|
Continuous |
|
others |
|
|
||||
|
|
|
|
|
|
|
XI. Agitation (Describe |
|
|
|
|
|
|
behaviors in comments |
Never |
Occasional |
Regular |
|
Continuous |
|
section) |
|
|
|
|
|
|
10(f) Health care
(a) Probably can make higher level decisions (such as whether to undergo or withdraw
(b) Probably can make limited decisions that require simple understanding.
(c) Probably can express agreement with decisions proposed by someone else.
(d) Cannot effectively participate in any kind of health care
11.* Ability to
(a) Independently without assistance
(b) Can do so with physical assistance, reminders, or supervision only
(c) Need to have medications administered by someone else
___________________________________ |
________________ |
Print Name |
Date |
______________________________________ |
|
Signature of Health Care Practitioner |
|
Form 4506 Revised
4
Resident Name __________________________________ |
Date Completed ______________________ |
Date of Birth ____________________________________ |
|
PRESCRIBER’S MEDICATION AND TREATMENT ORDERS AND OTHER INFORMATION
Allergies (list all): ___________________________________________________________________________________________________________________
Note: Does resident require medications crushed or in liquid form? Indicate in 12(a) with medication order. If medication is not to be crushed please indicate.
12(a) Medication(s). Including PRN, OTC, herbal, & dietary supplements.
Include dosage route (p.o., etc.), frequency, duration (if limited).
12(b) All related diagnoses, problems, conditions.
Please include all diagnoses that are currently being treated by this medication.
12(c) Treatments (include frequency & any instructions about when to notify the physician).
Please link diagnosis, condition or problem as noted in prior sections.
12(d) Related testing or monitoring.
Include frequency & any instructions to notify physician.
Prescriber’s Signature ________________________________________________________ |
Date |
______________________________ |
Office Address ______________________________________________________________ |
Phone |
______________________________ |
Form 4506 Revised
5
Resident Name __________________________________ |
Date Completed ______________________ |
Date of Birth ____________________________________ |
|
PRESCRIBER’S MEDICATION AND TREATMENT ORDERS AND OTHER INFORMATION
Allergies (list all): ___________________________________________________________________________________________________________________
Note: Does resident require medications crushed or in liquid form? Indicate in 12(a) with medication order. If medication is not to be crushed please indicate.
12(a) Medication(s). Including PRN, OTC, herbal, & dietary supplements.
Include dosage route (p.o., etc.), frequency, duration (if limited).
12(b) All related diagnoses, problems, conditions.
Please include all diagnoses that are currently being treated by this medication.
12(c) Treatments (include frequency & any instructions about when to notify the physician).
Please link diagnosis, condition or problem as noted in prior sections.
12(d) Related testing or monitoring.
Include frequency & any instructions to notify physician.
Prescriber’s Signature ________________________________________________________ |
Date |
______________________________ |
Office Address ______________________________________________________________ |
Phone |
______________________________ |
Form 4506 Revised
Form Data
| Fact Name | Description | Governing Law(s) |
|---|---|---|
| Form Usage | This form is designed for a comprehensive physical assessment by healthcare professionals for residents in assisted living facilities. | Maryland Regulations |
| Healthcare Professionals | Authorized to be filled by primary physicians, certified nurse practitioners, registered nurses, certified nurse-midwives, or physician assistants. | N/A |
| Residency Restrictions | Details conditions under which a resident cannot be admitted to an assisted living program, such as needing more than intermittent nursing care or ventilator services. | Maryland Regulations |
| Hospice Care Exception | Provides exceptions for residents under the care of a licensed general hospice program despite listed conditions. | Maryland Regulations |
| Medical History | Requires information on current and past illnesses, chronic conditions, and any significant changes in health status within the past 6 months. | N/A |
| Allergies and Communicable Diseases | Requires listing of allergies and status on communicable diseases like TB. | N/A |
| Substance Abuse History | Queries on the resident's history and current status regarding abuse of substances. | N/A |
| Risk Assessment | Assesses the risk factors for falls, injury, and asks about nutritional status, weight changes, and potential for dehydration. | N/A |
| Cognitive and Behavioral Status | Evaluates the resident's cognitive health, including dementia diagnosis and behavioral tendencies. | N/A |
| Self-Care Capabilities | Reviews the resident's capability to self-administer medication and make healthcare decisions. | N/A |
| Medication and Treatment Orders | Includes a section for prescribers to list current medications, related diagnoses, and specific treatment orders. | N/A |
Instructions on Utilizing Health Practitioner Physical Assessment
Filling out the Health Practitioner Physical Assessment form is an essential step in ensuring that patients in assisted living receive the appropriate level of care. This comprehensive assessment must be conducted by a qualified health care practitioner, including primary physicians, certified nurse practitioners, registered nurses, certified nurse-midwives, or physician assistants. The form covers a broad spectrum of health and behavioral issues to ensure an all-encompassing review of the patient's condition. To complete this form correctly, follow the step-by-step instructions provided below, paying close attention to each section and accurately documenting all relevant information.
- Enter the patient's full name, the date the form is being completed, and the patient's date of birth at the top of the form.
- In section 1, provide a brief overview of the resident's current medical and psychiatric history. Include any recent changes in health or behavioral status within the past six months, such as hospitalizations or falls.
- Describe past illnesses or chronic conditions, previous suicide attempts, and any notable changes in the resident's physical, functional, and psychological condition over the years in section 2.
- List all known allergies or sensitivities to food, medications, or environmental factors in section 3, detailing the nature of the reaction experienced.
- For section 4, indicate if the resident is free from communicable tuberculosis (TB) and other active airborne diseases, providing details on tests done to verify status if applicable.
- In section 5, detail any history or current issue related to the abuse of substances including prescription and non-prescription drugs, alcohol, and other inhalants.
- Identify risk factors for falls and injuries in section 6 by checking all that apply to the resident's current health status.
- Describe any skin condition(s), including history of or current ulcers, rashes, or tears in section 7, along with any standing treatment orders.
- Check the appropriate boxes in section 8 to indicate any sensory impairments that affect the resident’s functioning, including hearing, vision, and temperature sensitivity.
- Document the resident's current nutritional status in section 9, noting any significant weight changes, evidence of malnutrition or dehydration, and any special dietary needs or restrictions.
- Assess the resident's cognitive and behavioral status in section 10, including evidence of dementia, cognitive impairments, mood, emotions, and behaviors. Fill out section 10(e) with details on the frequency or intensity of these conditions.
- In section 11, evaluate the resident’s ability to self-administer medications, choosing the option that best describes their capability.
- Complete the Prescriber’s Medication and Treatment Orders and Other Information section with a detailed list of all medications including dosage, frequency, and duration, along with any related diagnoses. Also, note if the resident requires medications in a specific form, such as crushed or liquid.
- Have the health care practitioner print their name, sign the form, and provide the date of completion along with their office address and phone number.
Once the Health Practitioner Physical Assessment form is filled out, it’s crucial to review it for accuracy and completeness. This document will greatly assist in providing a thorough understanding of the resident's needs, enabling caregivers and medical professionals in an assisted living setting to deliver personalized and effective care.
Obtain Answers on Health Practitioner Physical Assessment
What is the purpose of the Health Practitioner Physical Assessment Form?
This form is designed for use by health care practitioners—such as primary physicians, certified nurse practitioners, registered nurses, certified nurse-midwives, or physician assistants—to document a comprehensive physical assessment of a resident in an assisted living program. Its purpose is to ensure that the resident's health status is fully evaluated to determine if the assisted living program can adequately meet their needs, considering the regulatory requirements that restrict certain conditions from being managed within such settings.
Who can complete the Health Practitioner Physical Assessment Form?
Authorized professionals including primary physicians, certified nurse practitioners, registered nurses, certified nurse-midwives, or physician assistants are qualified to complete this assessment. It is important that the person completing the form has the appropriate credentials to conduct a thorough and accurate health evaluation of the resident.
What are the regulatory restrictions mentioned in the form?
Under Maryland regulations, assisted living programs are not permitted to admit residents who, at the time of initial assessment, require:
- More than intermittent nursing care
- Treatment of stage three or stage four skin ulcers
- Ventilator services
- Skilled monitoring, testing, and aggressive adjustment of medications and treatments for fluctuating acute conditions
- Monitoring of a chronic medical condition that is not controllable through readily available medications and treatments
- Treatment for diseases or conditions requiring more than contact isolation
What information is required in the current medical and psychiatric history section?
This section requires brief descriptions of any recent changes in the resident's health or behavioral status, including but not limited to suicide attempts, hospitalizations, falls, or significant alterations in health within the past six months. This helps in identifying any triggers that may require awake overnight staff attention.
How should allergies be recorded on the form?
Allergies or sensitivities to food, medications, or environmental factors should be listed clearly, including the nature of reactions they cause—such as rashes, anaphylactic reactions, or gastrointestinal symptoms. Medication allergies must also be noted in a separate section dedicated to medication allergies for clear visibility.
What details are needed under the communicable diseases section?
It must be indicated whether the resident is free from communicable tuberculosis (TB) and any other active reportable airborne communicable diseases. If not, the specific communicable disease must be named. Furthermore, details about tests conducted to verify the resident's freedom from active TB, including PPD tests and chest X-rays, as applicable, along with their dates and results, need to be provided.
How is the risk for falls and injury assessed?
Conditions increasing the resident's risk of falling or injury should be checked off from a list that includes options like orthostatic hypotension, osteoporosis, gait problems, impaired balance, confusion, Parkinsonism, foot deformity, pain, the use of assistive devices, among others. Any other relevant conditions not listed should be explained in detail.
What information is required regarding cognitive/behavioral status?
This section assesses for evidence of dementia, including whether an evaluation for dementia has been conducted, the diagnosis or cause(s) of dementia, and the results of a Mini-Mental Status Exam if tested. Additional details regarding cognition, communication, mood and emotions, and behaviors are captured through rating the frequency or intensity of certain behaviors, such as disorientation, impaired judgment, anxiety, depression, and unsafe behaviors.
How is the resident's ability to self-administer medications evaluated?
Based on a review of the resident’s functional capabilities, physical and cognitive status, and limitations, the health practitioner must rate the resident’s capability to safely and appropriately take their medications. Options range from being able to do so independently without assistance, requiring physical assistance or reminders, to needing someone else to administer the medications.
Common mistakes
When filling out the Health Practitioner Physical Assessment form, accuracy and thoroughness are crucial. However, many people tend to make some common mistakes, which can lead to incomplete or inaccurate information being recorded. Here are seven common mistakes to avoid:
Not fully detailing the current medical and psychiatric history. It's important to describe any recent changes in health or behavioral status comprehensively, yet this section often lacks enough detail.
Skipping or being vague about past illnesses or chronic conditions. Each condition, including past hospitalizations or significant health events, provides vital information for current care plans.
Forgetting to list allergies or sensitivities to food, medications, or environmental factors. Also, medication allergies need to be entered in both the allergies section and the medication allergies section for emphasis and clarity.
Omitting information on communicable diseases, especially if the resident has a history of TB or any other reportable diseases. It's crucial to indicate which tests were done to verify the condition.
Overlooking details about substance abuse history or current issues. It’s essential to specify the type of substance and the recency of abuse or misuse for a comprehensive understanding.
Ignoring or underestimating risk factors for falls and injury. Often, people check off conditions but fail to give additional explanations or note other relevant risk factors in the space provided.
Incompletely addressing nutritional status and needs. Any weight changes, risk of malnutrition or dehydration, and dietary requirements must be thoroughly explained to ensure proper care.
Avoiding these mistakes helps ensure the assessment form is filled out comprehensively, accurately reflecting the resident's health status and care needs. This attention to detail supports the provision of high-quality, individualized care.
Documents used along the form
The Health Practitioner Physical Assessment form plays a critical role in managing a resident's health within an assisted living program. It ensures that individuals receive the appropriate level of care and that their unique health needs are accurately documented and addressed. However, this form is often just one component of a comprehensive health documentation strategy. To provide a full picture of a resident's health status and needs, several other forms and documents are commonly used alongside the Health Practitioner Physical Assessment form.
- Medication Administration Record (MAR): This document is essential for tracking all the medications a resident is taking, including the dosage, frequency, and route of administration. It helps healthcare practitioners monitor a resident's adherence to their medication regimen and watch for potential drug interactions.
- Advance Directives: These legal documents allow a resident to outline their preferences for medical treatment and end-of-life care in advance. It includes living wills and durable power of attorney for healthcare, ensuring that a resident's wishes are respected even if they become incapable of making decisions for themselves.
- Care Plan: A care plan is developed based on the comprehensive assessment results, including the physical assessment form. It details the resident's health conditions, required treatments or interventions, and goals for improvement or maintenance of health. This living document is regularly reviewed and adjusted as the resident's needs change.
- Incident Reports: Whenever an unusual event or accident happens (e.g., falls, medical emergencies), an incident report is filled out. It records the details of the incident, the response actions taken, and any follow-up care or changes to the care plan that are required. Incident reports are crucial for risk management and improving resident safety.
Together, these documents provide a comprehensive account of a resident's health care needs, preferences, and the care they are receiving. They allow health practitioners and care teams to deliver personalized, detailed, and effective care to each resident within an assisted living setting. Keeping these documents up-to-date and readily accessible ensures that residents receive the highest quality of care tailored to their individual needs.
Similar forms
Medical History and Physical Examination Form: Similar to the Health Practitioner Physical Assessment form, this document also collects comprehensive health information, including past medical history, psychiatric history, and a detailed physical examination. Both forms are critical to understanding a patient's overall health status and ensuring proper care in clinical or assisted living settings.
Medication Administration Record (MAR): While the MAR specifically tracks the administration of medications, including dosages, times, and frequencies, its requirement for detailed medication allergies and treatments aligns closely with sections 12 (a) and 12 (b) of the Health Practitioner Physical Assessment form. Both documents ensure medication safety and adherence.
Nursing Assessment Form: This form, used by nurses to evaluate new patients, covers areas similar to the Health Practitioner Physical Assessment form, such as allergies, history of substance abuse, and the risk factors for falls and injuries. It plays a fundamental role in creating a care plan, closely mirroring the assessment's goal of ensuring resident safety and well-being in assisted living facilities.
Nutritional Assessment Form: This focuses on a resident's nutritional status, risk for malnutrition, or dehydration, closely paralleling the nutritional status evaluation in the Health Practitioner Physical Assessment form. Both assessments are essential for tailoring diet plans and interventions to meet individual health care needs.
Cognitive Function Assessment Tools: Tools such as the Mini-Mental State Examination (MMSE) are designed to evaluate cognitive impairment, which is similar to section 10 of the Health Practitioner Physical Assessment form. Both identify cognitive deficits and assist in the planning of care and interventions suited to the resident's mental health status.
Functional Assessment Form: Evaluates a patient's ability to perform daily living activities independently, akin to the assessment's sections on the ability to self-administer medications and the use of assistive devices for eating. Understanding the functional capabilities of individuals helps in tailoring care and assistance to their needs.
Substance Abuse Assessment Form: Specifically focuses on identifying history and current problems related to the abuse of substances, including prescriptions, which the Health Practitioner Physical Assessment form also addresses. Both are vital for developing appropriate treatment and monitoring plans.
Dos and Don'ts
When it comes to filling out the Health Practitioner Physical Assessment form, accuracy and attention to detail are paramount. This form plays a crucial role in ensuring that residents receive the tailored care they need. Below are some critical dos and don'ts to keep in mind while completing this form.
Do:
- Verify the resident’s name, date of birth, and the completion date at the beginning of the form to ensure that all information provided relates to the correct individual.
- Provide detailed descriptions for all fields, especially those marked with an asterisk (*), as these indicate critical triggers for awake overnight staff and require special attention.
- Include comprehensive medical and psychiatric history, noting any recent changes in health, allergies, chronic conditions, and any history of substance abuse or misuse.
- Accurately indicate the resident’s risk factors, including fall risks and skin conditions, to enable caretakers to implement necessary precautions and treatments.
- Review and sign the form, ensuring that all provided information is accurate and complete to the best of your knowledge.
Don't:
- Omit any critical health information or history that could influence the caretaking and medical treatment of the resident.
- Leave relevant sections blank; if a section does not apply, mark it as N/A (Not Applicable) to indicate that it has been reviewed but is not relevant to the resident’s current condition.
- Assume details are not important; minor health changes or conditions can greatly impact the overall assessment and subsequent care plans.
- Forget to indicate any communication barriers or cognitive impairments, as these are crucial for tailoring interaction and care approaches.
- Overlook the need to document all allergies, including those to medications, food, and environmental factors, to prevent adverse reactions.
Misconceptions
Many people have misconceptions about the Health Practitioner Physical Assessment form, especially regarding its purpose and how it is utilized within health care settings. Let’s clear up some of these misunderstandings:
- Only physicians can complete the form. This is incorrect. Aside from primary physicians, certified nurse practitioners, registered nurses, certified nurse-midwives, and physician assistants are also authorized to complete this form. It's designed to encompass a broad range of healthcare professionals to ensure comprehensive patient assessment.
- It’s primarily used for hospital admissions. Actually, this form is not limited to hospital admissions. While it can be a part of that process, its use extends to various settings, including assisted living programs. It's instrumental in creating a baseline health assessment for individuals entering these facilities, ensuring they receive appropriate care that aligns with their health status.
- The form covers only current medical conditions. This assumption is incomplete. While current medical and psychiatric conditions are a critical component, the Health Practitioner Physical Assessment form also requires detailed information on past illnesses, chronic conditions, allergies, medication history, and substance misuse, among others. This comprehensive approach helps in understanding the resident’s overall health status.
- Completion of the form means automatic acceptance into an assisted living facility. Submission of this form is a step in the assessment process, but under Maryland regulations, there are specific conditions (like requiring more than intermittent nursing care or having certain skin ulcers) that may preclude admission into an assisted living program. It's crucial to understand this form is part of broader criteria used to determine the suitability of a resident for the facility.
- All sections of the form must be completed for every resident. While comprehensive completion is important to provide a full picture of the resident's health, there are parts of the form noted with an asterisk that serve as “triggers” for awake overnight staff. Additionally, some sections might not apply to every individual. It’s the role of the completing health professional to determine relevancy and completeness based on each resident's unique situation.
Understanding these key points about the Health Practitioner Physical Assessment form can demystify its purpose and usage, clarifying its role in ensuring quality care and appropriate living arrangements for individuals in various health care and living facilities.
Key takeaways
Filling out the Health Practitioner Physical Assessment form requires attention to detail and comprehensive knowledge about the resident's health status. Here are key takeaways to consider.
- Only qualified health professionals can complete the form. This includes primary physicians, certified nurse practitioners, registered nurses, certified nurse midwives, or physician assistants.
- Questions marked with an asterisk (*) are crucial for determining the need for awake overnight staff, indicating the importance of accurately assessing and responding to these triggers.
- The form outlines specific conditions that, if present at the time of initial admission, disqualify a resident from being admitted into an assisted living program under Maryland regulations. Exceptions are made for those under licensed general hospice care.
- It's imperative to provide a thorough medical and psychiatric history, including recent changes in health, behavior, and any past illnesses or chronic conditions. This helps in understanding the resident's current needs and potential risks.
- Allergies and communicable diseases must be clearly listed, along with pertinent details like the nature of allergic reactions and tests confirming the absence of active communicable diseases.
- The form requires detailed information on the resident's risk factors for falls, skin conditions, sensory impairments, nutritional status, and more, to comprehensively assess their physical state.
- Assessing the cognitive and behavioral status is crucial, including potential dementia, to tailor the care plan to the resident's mental health needs.
- The ability to self-administer medication is a crucial component, directly impacting the level of care and supervision required by the resident.
Understanding and accurately completing the Health Practitioner Physical Assessment form ensures that residents receive the appropriate level of care and that their health and safety needs are adequately met.
Popular PDF Forms
Printable Nfpa 25 Nfpa Fire Sprinkler Inspection Forms - Featuring fields for detailed property and service organization information, this form fosters clear communication between parties involved in fire safety.
Idaho Re 21 - It mandates the seller to provide a warranty deed, unless otherwise agreed, ensuring clear title transfer to the buyer.