Blank Home Health Audit PDF Template
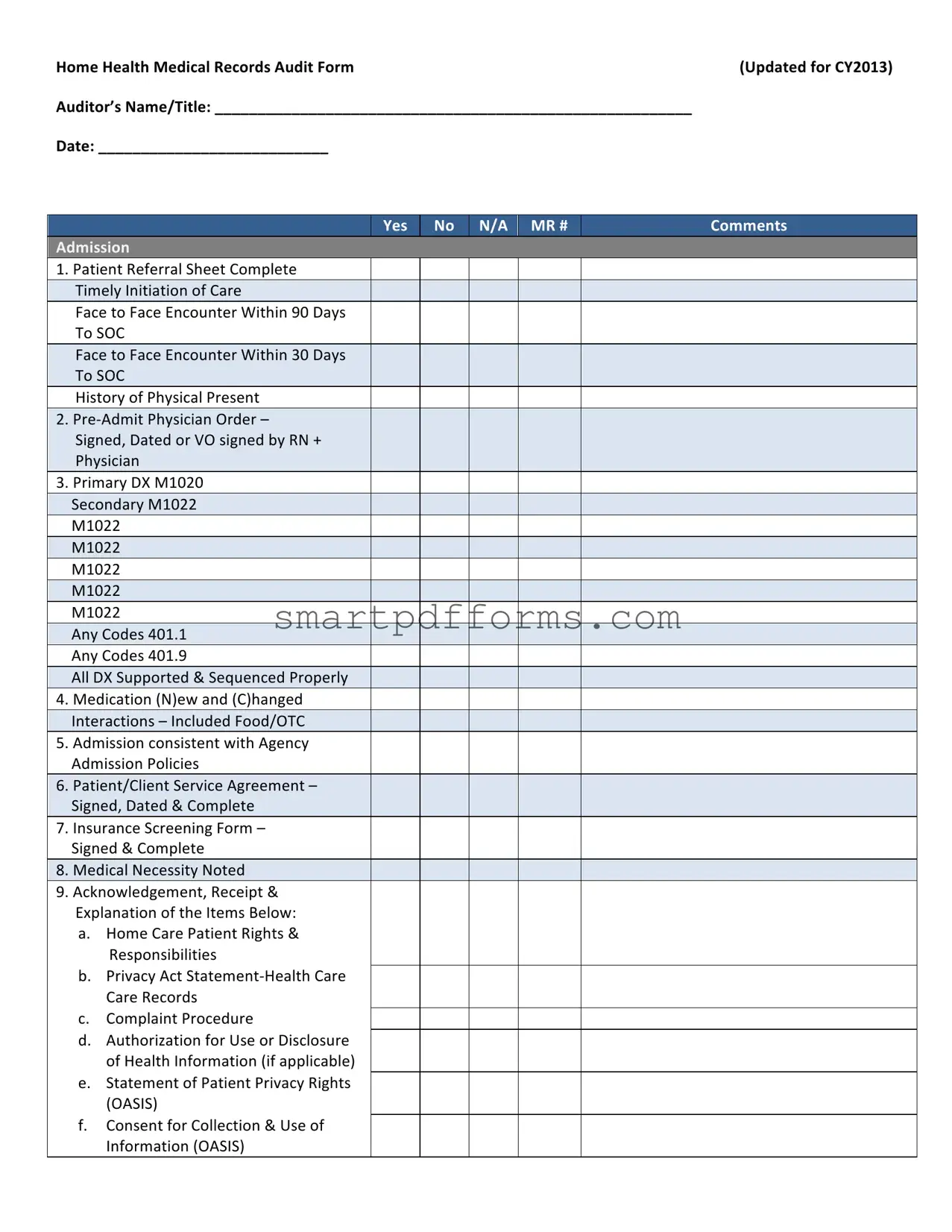
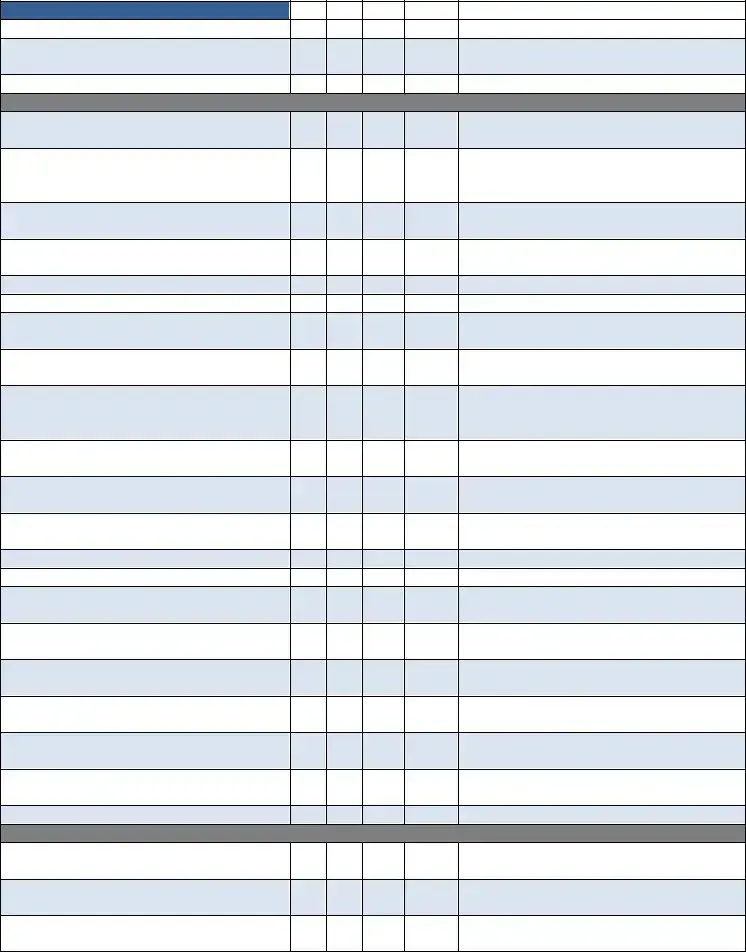
The Home Health Medical Records Audit Form, revised for the calendar year 2013, serves as a comprehensive tool for assessing the quality and completeness of home health care documentation, vital for ensuring patient safety, regulatory compliance, and the facilitation of coordinated care. The audit covers a broad array of categories, including but not limited to, timely admission and initiation of care, accurate and complete documentation of patient encounters, physician orders, diagnosis coding, medication management, patient rights, emergency preparedness, care plans, and skilled nursing notes. It further evaluates the consistency and comprehensiveness of OASIS assessments, adherence to physician orders, homebound status documentation, the effectiveness of treatment and intervention documentation, the involvement of home health aides, and therapy services rendered. Each item on the audit form is meticulously designed to verify the presence of essential documentation and to ensure it meets the stipulated guidelines, such as signatures, dates, and correct sequencing of diagnoses and care plans. This exhaustive process underscores the importance of meticulous record-keeping in home health care, aiming to enhance the quality of care, optimize patient outcomes, and ensure compliance with healthcare standards and regulations.
Preview - Home Health Audit Form
Home Health Medical Records Audit Form |
(Updated for CY2013) |
Auditor’s Name/Title: ________________________________________________________ |
|
Date: ___________________________ |
|
Yes
No
N/A MR #
Comments
Admission
1.Patient Referral Sheet Complete Timely Initiation of Care
Face to Face Encounter Within 90 Days To SOC
Face to Face Encounter Within 30 Days To SOC
History of Physical Present
2.Pre‐Admit Physician Order –
Signed, Dated or VO signed by RN + Physician
3.Primary DX M1020 Secondary M1022 M1022
M1022
M1022
M1022
M1022
Any Codes 401.1 Any Codes 401.9
All DX Supported & Sequenced Properly
4.Medication (N)ew and (C)hanged Interactions – Included Food/OTC
5.Admission consistent with Agency Admission Policies
6.Patient/Client Service Agreement – Signed, Dated & Complete
7.Insurance Screening Form – Signed & Complete
8.Medical Necessity Noted
9.Acknowledgement, Receipt & Explanation of the Items Below:
a.Home Care Patient Rights & Responsibilities
b.Privacy Act Statement‐Health Care Care Records
c.Complaint Procedure
d.Authorization for Use or Disclosure of Health Information (if applicable)
e.Statement of Patient Privacy Rights (OASIS)
f.Consent for Collection & Use of Information (OASIS)
Yes |
No |
N/A |
MR # |
Comments |
|
|
|
|
|
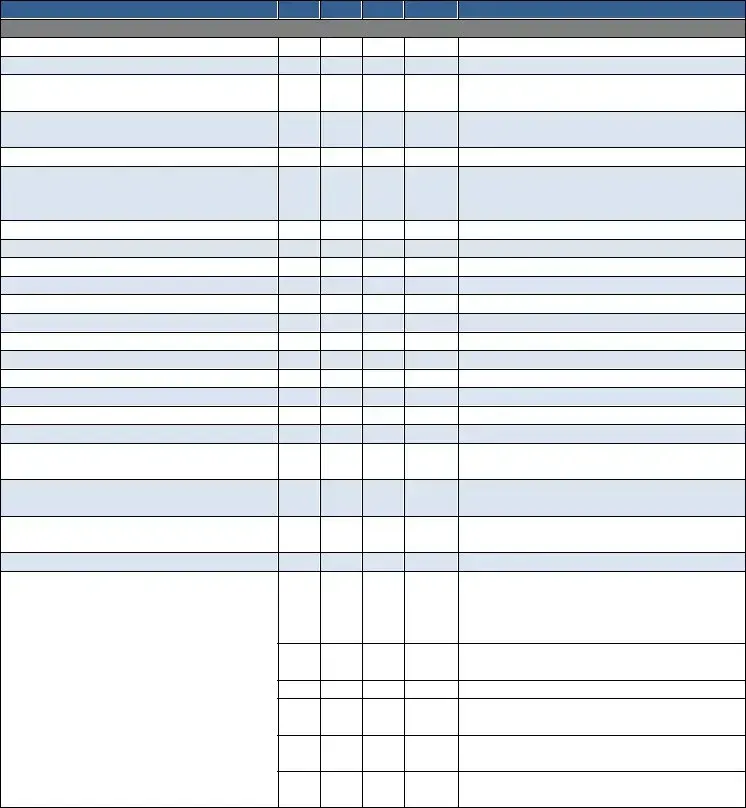
g.Emergency Preparedness Plan/Safety Instructions
h.Advance Directives & HHABN
10. Complete Post Evaluation –
D/C Summary Report by RN/PT/OT/ST on:
a. Start of Care
b. Resumption of Care
c. Recertification
Plan of Care 485
11.Plan of Care Signed & Dated by Physician Within 30 Working Days or State Specific days‐ ________
12.Diagnoses Consistent with Care Ordered
13.Orders Current
14. Focus of Care Substantiated
15.Daily Skilled Nurse Visit Frequencies with Indication of End Point
16. Measurable Goals for Each Discipline
17. Tinetti or TUG Completed at SOC
18. Recertification Plan of Care Signed &
Dated Within 30 Days or State Required
Time
19.BiD Insulin Visits Documented with Vision, Musculoskeletal Need, Not Willing/Capable Caregiver. MSW Every Episode
20. Skilled Nurse Consult
Medication Profile Sheet
21.Medication Profile Consistent with the 4 485
22. Medication Profile Updated at
Recertification, ROC, SCIC, Initialed &
Dated
23.Medication Profile Complete with Pharmacy Information
Physician Orders/Change Verbal Orders
24. Change/Verbal Orders Include Disciplines, Goals, Frequencies, Reason for Change, Additional Supplies as Appropriate
25.Change Orders Signed & Dated by Physician Within 30 Working Days
OASIS Assessment Form
26. Complete, Signed & Dated by:
___________________________
27.M2200 Answer Meets the Threshold for a Medicare High Case Mix Group
28. M1020 & M1022 Diagnoses & ICD‐9 are Consistent with the Plan of Care
Yes |
No |
N/A |
MR # |
Comments |
|
|
|
|
|
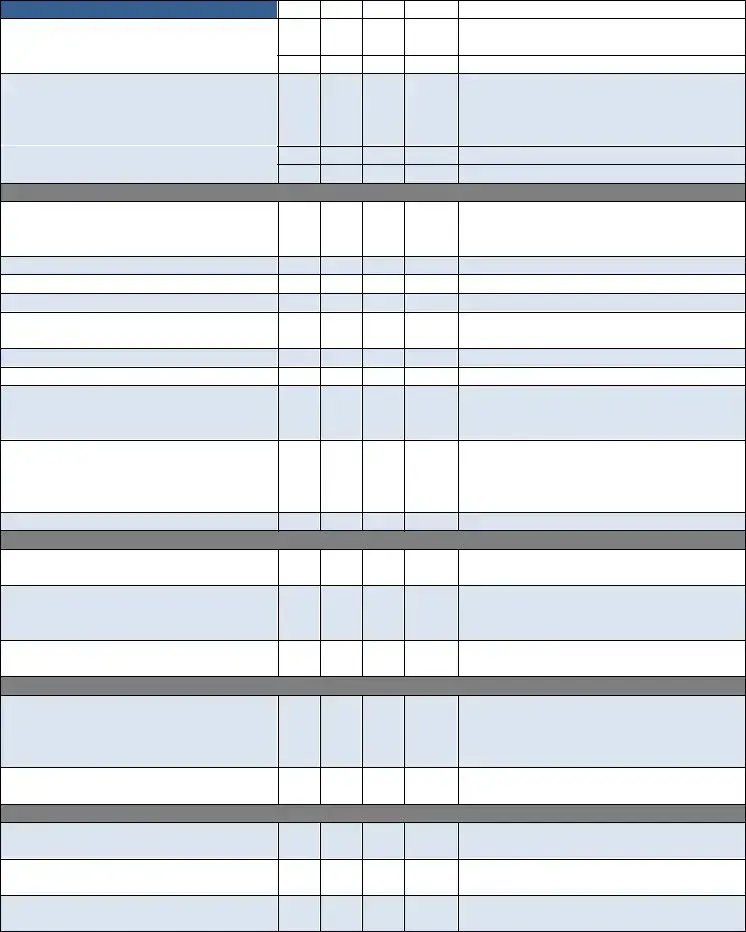
29.All OASIS Assessments Were Exported Within 30 Days
30. OASIS Recertifications Were Done
Within 5 Days of the End of the Episode
31.All OASIS Were Reviewed for Consistency in Coordination with the Discipline Who Completed the Form
Skilled Nursing Clinical Notes
32. Visit Frequencies & Duration are Consistent with Physician Orders
33.Orders Written for Visit Frequencies/ Treatment Change
34. Homebound Status Supported on Each Visit Note
35.Measurable Goals for Each Discipline with Specific Time Frames
36. Frequency of Visits Appropriate for Patient’s Needs & Interventions Provided
37. Appropriate Missed Visit (MV) Notes
38. Skilled Care Evident on Each Note
39. Evidence of Coordination of Care
40. Every Note Signed & Dated
41. Follows the Plan of Care (485)
42. Weekly Wound Reports are Completed
43. Missed Visit Reports are Completed
44. Pain Assessment Done Every Visit with Intervention (If Applicable)
45.Abnormal Vital Signs Reported to Physician & Case Managers
46. Evidence of Interventions with Abnormal Parameters/Findings
47.Skilled Nurse Discharge Summary/ Instructions Completed
48. LVN Supervisory Visit Every 30 Days by Registered Nurse
Certified Home Health Aide
49.Visit Frequencies & Duration Consistent with Physician Orders
50. Personal Care Instructions Documented,
Signed & Dated
51.Personal Care Instructions Modified as Appropriate
52. Notes Consistent with Personal Care Instructions Noted on the CHHA Assignment Sheet Completed by the RN/PT/ST/OT
53.Notes Reflect Supervisor Notification of Patient Complications or Changes
54. Visit Frequencies Appropriate for Patient Needs
Yes |
No |
N/A |
MR # |
Comments |
|
|
|
|
|
55. Each Note Reflects Personal Care Given
56. Supervisory Visits at Least Every 14 Days by RN or PT
57. Every Note Signed & Dated
PT
58. Assessment Includes Evaluation,
Care Plan & Visit Note
59.Evaluation Done Within 48 Hours of Referral Physician Order or Date Ordered
60. Visit Frequencies/Duration Consistent with Physician Orders
61.Evidence of Need for Therapy/Social Service
62. Appropriate Missed Visit (MV) Notes
63. Notes Consistent with Physician Orders
64. Evidence of Skilled Service(s) Provided
in Each Note
65.Treatment/Services Provided Consistent with Physician Orders & Care Plan
66. Notes Reflect Supervisor & Physician Notification of Patient Complications or Changes
67.Specific Evaluation & “TREAT” Orders Prior to Care
68. Verbal Orders for “TREAT” Orders Prior to Care
69.Homebound Status Validated in Each Visit Note
70. Notes Reflect Progress Toward Goals
71. Evidence of Discharge Planning
72. Evidence of Therapy Home Exercise
Program
73.Discharge/Transfer Summary Complete with Goals Met/Unmet
74. Assessment & Evaluation performed by Qualified Therapist Every 30 Days
75.Supervision of PTA/OTA at Least Every 2 Weeks
76. Qualified Therapy Visit 13th Visit (11, 12, 13)
77.Qualified Therapy Visit 19th Visit (17, 18, 19)
78. Every Visit Note Signed & Dated
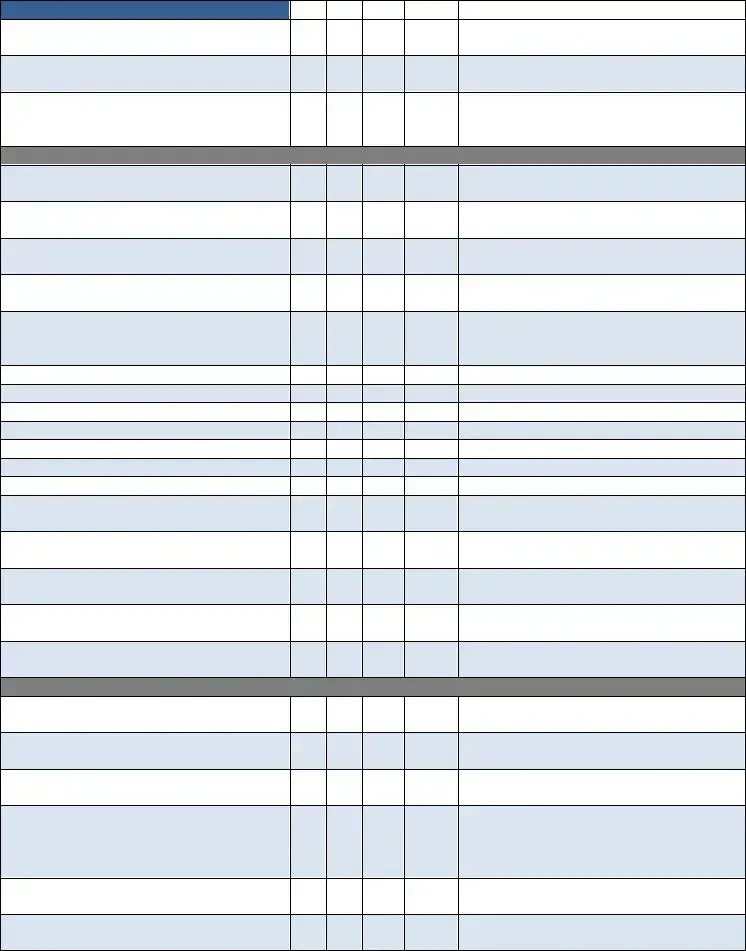
SLP
79.Assessment Includes Evaluation, Care Plan & Visit Note
80. Evaluation Done Within 48 Hours of Referral Physician Order or Date Ordered
81.Visit Frequencies/Duration Consistent with Physician Orders
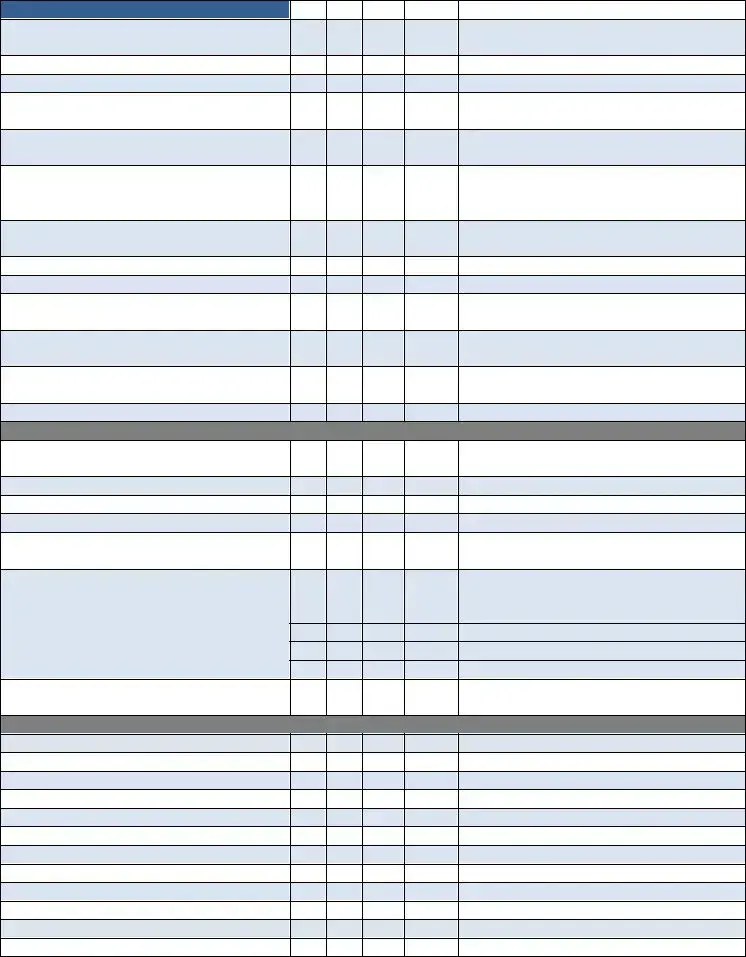
Yes |
No |
N/A |
MR # |
Comments |
|
|
|
|
|
82. Evidence of Need for Therapy/Social Service
83. Appropriate Missed Visit (MV) Note
84. Notes Consistent with Physician Orders
85.Evidence of Skilled Service(s) Provided in Each Note
86. Treatment/Services Provided Consistent with Physician Orders & Care Plan
87.Notes Reflect Supervisor & Physician Notification of Patient Complications or Changes
88. Homebound Status Validated in Each Visit
Note
89. Notes Reflect Progress Toward Goals
90. Evidence of Discharge Planning
91.Evidence of Therapy Home Exercise Program
92. Discharge/Transfer Summary Complete with Goals Met/Unmet
93.Supervision of PTA/OTA at Least Every 2 Weeks
94. Every Visit Note Signed & Dated
Miscellaneous
95.Progress Summary Completed(30‐45Days) Each Episode Signed & Dated
96. Field Notes are Submitted & Complete
97. Chart in Chronological Order
98. Chart in Order per Agency Policy
99.Patient Name & Medical Records Number on Every Page
100. Physician Orders are Completed/ Updated for Clinical Tests Such as:
a. Coumadin: Protime/INR
b. Hemoglobin A1C
c. CBC, Metabolic Panel, CMP
d. Others: _______________________
101.Communication with Physician Regarding Test Results
Process Measures:
Timely Initiation of Care
Influenza Received
PPV Ever Received
Heart Failure
DM Foot Care & Education
Pain Assessment
Pain Intervention
Depression Assessment
Medication Education
Falls Risk Assessment
Pressure Ulcer Prevention
Pressure Ulcer Risk Assessment
Additional Comments/Recommendations ‐
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
__________________________________________________________________________________________________
THE FOLLOWING IS APPLICABLE FOR QUARTERLY MEDICAL REVIEW REPORT
REVIEWED AND SIGNED BY THE FOLLOWING DISCIPLINARY REPRESENTATIVE
______________________________________ |
______________________________________ |
Registered Nurse |
Occupational Therapist (If Applicable) |
______________________________________ |
______________________________________ |
Physical Therapist (If Applicable) |
Speech Language Pathologist (If Applicable) |
______________________________________ |
______________________________________ |
Medical Director |
MSW (If Applicable) |
MR # ______________________
Form Data
| Fact Number | Fact Detail |
|---|---|
| 1 | The Home Health Medical Records Audit Form is updated for the Calendar Year 2013. |
| 2 | It includes sections for both mandatory and optional (Yes, No, N/A) entries regarding patient admission, medication, and service agreements. |
| 3 | The form requires detailed information about the admission process, including referral sheet completeness, timely initiation of care, face-to-face encounters, and history of physical presence. |
| 4 | There are specific sections dedicated to physician orders, diagnoses codes, medication profiles, including interactions and updates at recertification. |
| 5 | Patient rights, privacy act statements, complaint procedures, and emergency preparedness plans are among the items that must be acknowledged, received, and explained. |
| 6 | The audit form covers a wide range of processes including, but not limited to, skilled nursing clinical notes, certified home health aide notes, physical therapy assessments, and miscellaneous operational aspects like progress summary and chart order. |
Instructions on Utilizing Home Health Audit
Filling out the Home Health Audit form requires attention to detail and a comprehensive review of the patient's medical records. This task ensures that all aspects of home health care meet the required standards for quality and compliance. Upon completion of this form, it should be submitted to the designated supervisor or compliance department for review. This will facilitate the necessary actions to address any identified issues, reinforcing the commitment to high-quality patient care. The process harmonizes with regulatory requirements and supports continuous improvement in home health care services.
- Enter the Auditor’s Name/Title and the Date of the audit at the top of the form.
- Review the patient's Admission section, checking each item (Patient Referral Sheet, Timely Initiation of Care, etc.) against the medical record. Mark "Yes," "No," or "N/A" accordingly and provide comments if necessary.
- In the section labeled "Yes No N/A MR # Comments," thoroughly assess each component listed (e.g., Primary DX, Medication, Admission consistency) based on the patient’s medical records.
- For items such as Medication interactions and adherence to Admission Policies, verify the information and document any discrepancies or confirmations in the "Comments" area.
- Ensure that all legal and regulatory documents (Home Care Patient Rights & Responsibilities, Privacy Act Statement, etc.) are signed, dated, and complete.
- Examine the Plan of Care section, including physician orders, diagnoses, and the focus of care. Confirm these are consistent, current, and substantiated within the specified time frames.
- Inspect sections pertaining to OASIS Assessment Form, Skilled Nursing Clinical Notes, and Certified Home Health Aide, checking the consistency of visit frequencies, duration, and the appropriateness of care provided.
- Assess the therapy and social service sections (PT, SLP) for evaluations, care plans, and visit notes to ensure they align with physician orders and reflect progress towards goals.
- Complete the Miscellaneous section by reviewing progress summaries, field notes, and ensuring the chart is in chronological order and follows agency policy. Verify each page includes the patient's name and medical record number.
- Review and confirm the completion of Process Measures sections, which include timely initiation of care, vaccinations received, and assessments for depression, medication, falls risk, and pressure ulcer prevention.
- Once the audit form is fully completed, go through each section to ensure nothing was overlooked and that all information provided is accurate and reflective of the patient's records and care received.
- Submit the completed form to the designated supervisor or compliance department for further evaluation and follow-up action.
Obtain Answers on Home Health Audit
-
What is the Home Health Audit form?
The Home Health Audit form is a tool used by auditors to review and ensure compliance with regulatory requirements for home health agencies. It scrutinizes various aspects such as patient referral, admission processes, medication management, patient rights, emergency preparedness, care plans, OASIS assessment forms, skilled nursing clinical notes, certified home health aide documentation, and therapy services documentation.
-
Why is the Home Health Medical Records Audit form important?
This form plays a crucial role in maintaining high standards of care in home health services. It helps identify areas of non-compliance with health regulations, highlights best practices, and underscores areas needing improvement. By ensuring that all necessary documentation is complete and up to date, it ultimately contributes to the provision of safe, effective, and high-quality care to patients.
-
Who completes the Home Health Audit form?
The audit form is typically completed by an auditor with a title or position relevant to quality control or compliance within a home health agency. This could include a range of professionals from internal auditors to external consultants specialized in home health care standards and regulations.
-
What does "Timely Initiation of Care" mean on the audit form?
"Timely Initiation of Care" refers to the requirement that home health services begin within a specific timeframe after a physician's referral or hospital discharge to ensure continuity of care and to meet the patient's immediate healthcare needs. Compliance with this item ensures patients receive the necessary care without undue delay.
-
How is medication management audited in this form?
Medication management is evaluated through several criteria, including whether medication (new or changed) interactions with food or over-the-counter drugs are included, if the medication profile is consistent with physician orders, updated appropriately, and complete with pharmacy information. This ensures accuracy in medication administration and reduces the risk of medication errors.
-
What is the significance of the OASIS Assessment Form within the Home Health Audit?
The OASIS (Outcome and Assessment Information Set) Assessment Form is crucial for ensuring accurate patient assessments, determining home health care needs, and planning care. Compliance checks on this form include completeness, timely signing and dating by qualified personnel, and consistency of diagnoses with the care plan. It plays a key role in tailoring care to patient needs and documenting outcomes for regulatory compliance.
-
How does the audit form ensure compliance with patient rights and privacy?
Compliance with patient rights and privacy is ensured through documentation reviews including the acknowledgment and receipt of home care patient rights and responsibilities, privacy act statements, complaint procedures, and other pertinent authorizations. This confirms that patients are informed of their rights and that their information is handled in a confidential and secure manner.
-
What do "skilled nursing clinical notes" entail on this form?
Skilled nursing clinical notes cover a range of checks, from the consistency of visit frequencies and durations with physician orders to the documentation of homebound status, measurable goals for each discipline, interventions provided, and coordination of care. These notes provide evidence of the skilled care provided to the patient and help ensure each visit’s necessity and productivity.
-
How are therapy services evaluated?
Therapy services are evaluated by verifying that evaluations are conducted within a set timeframe, visit frequencies and durations are consistent with physician orders, the need for therapy or social services is evident, and treatments are provided as ordered. Documentation must reflect ongoing communication with supervisors and physicians regarding patient progress or complications.
-
What happens if non-compliance is found through the audit?
If non-compliance is detected, the agency is required to take corrective actions to address the deficiencies identified. This might include revising policies, additional staff training, improving documentation processes, or more closely monitoring care provision. These actions help to ensure that the agency returns to full compliance and continues to provide safe and effective care to its patients.
Common mistakes
Completing the Home Health Audit form accurately is essential for ensuring compliance and providing the highest quality of care. However, several common mistakes can lead to inaccuracies or omissions on this important document. Here are seven errors often made during the completion process:
Overlooking details in the patient referral sheet: It's critical to meticulously review the patient referral sheet for completeness. All necessary information must be provided timely to initiate the care process effectively.
Failing to document the face-to-face encounter correctly: The encounter must occur within specific time frames—either 90 days prior to the start of care (SOC) or within 30 days after SOC. This requirement is often misunderstood or not documented properly.
Not ensuring that the pre-admit physician order is appropriately signed and dated: Any verbal orders (VO) must be signed by both the RN and the physician, a step that is frequently missed.
Incorrectly coding or sequencing diagnoses: Diagnoses must be supported and sequenced correctly. Ensuring that the primary and secondary codes are accurate and properly listed is a common area of confusion.
Omitting medication interactions: Including new (N) and changed (C) medications, as well as their interactions with food or over-the-counter (OTC) products, is essential. Missing this information can have significant implications for patient care.
Incomplete patient/client service agreements: These must be fully executed—signed, dated, and complete. Yet, they are often submitted with missing details or signatures.
Inadequate documentation of skilled nursing clinical notes: Notes must substantiate the need for skilled care at each visit and reflect the plan of care (485). This documentation often lacks sufficient detail or fails to include every note signed and dated.
Each of these areas requires careful attention to avoid potential errors that could impact the audit's outcome. By understanding these common mistakes, individuals can take steps to ensure that their Home Health Audit forms are accurate and complete, thereby facilitating compliance and fostering optimal patient care.
Documents used along the form
When managing home health care, the Home Health Medical Records Audit Form serves as a crucial tool for ensuring quality and compliance within the care provided. However, to present a comprehensive and holistic view of the patient's care and to adhere to regulatory standards, this form is often accompanied by several other important documents. Each of these documents plays a significant role in delivering and documenting the care practice effectively and efficiently.
- Patient Referral Form: This document initiates the process of home health care. It contains the patient's personal information, medical history, and the referring physician's details and recommendations. The form ensures that the home health care agency understands the patient's initial condition and what services are being requested.
- OASIS (Outcome and Assessment Information Set): As part of the required documentation for Medicare and Medicaid, the OASIS form captures patient data at various points during home care. It assesses the patient's condition and the outcomes of care, helping in the standardization of data collection and facilitating the improvement of quality care.
- Physician’s Orders for Services and Plan of Care (Form CMS-485): This document outlines the medical and treatment plan as ordered by the patient's physician. It includes specific services, frequency of visits, medications, diet, and therapies. Signed by the physician, it acts as an official order that guides the healthcare professionals in delivering care.
- Consent and Authorization Forms: These include various consents and authorizations required by law, such as consent to treat, acknowledgment of privacy practices, and authorization for release of information. These forms ensure that the patient or their legal representative is informed about the care and agrees to the services provided, maintaining the patient's rights and the agency’s compliance with legal standards.
The integration and careful management of these documents, alongside the Home Health Medical Records Audit Form, streamline the process of delivering home health care. They ensure that all aspects of care are properly documented, patient rights are respected, and the care provided meets both the medical needs of the patient and the regulatory standards set by governing bodies. As such, these forms collectively support the goal of providing high-quality, individualized care in the patient's home.
Similar forms
Medical Audit Checklist: Similar to the Home Health Medical Records Audit Form, this checklist evaluates adherence to medical practices and documentation standards within a healthcare setting. Both forms assess whether medical records, care plans, and patient assessments are accurately documented and comply with defined policies.
Patient Admission Form: This document collects essential information at the time of patient admission, similar to the sections of the Home Health Audit form that verify if patient referrals and admissions are consistent with agency policies, ensuring all necessary documentation is completed and signed.
Medication Administration Record (MAR): The MAR tracks all medications prescribed and administered to patients, akin to how the Home Health Audit form checks for medication profile accuracy, updates, and whether interactions are included, ensuring patient safety and adherence to prescriptions.
Physician Order Sheet: Similar to portions of the Home Health Audit form that review all physician orders for current and relevant care, including verbal or change orders, ensuring that every order is signed, dated, and consistent with the patient's plan of care.
Quality Assurance (QA) Checklists for Home Health Care: These checklists evaluate the quality and effectiveness of home health care services. Much like the audit form, they review protocols for patient care, documentation, medication management, and adherence to prescribed treatments.
OASIS (Outcome and Assessment Information Set) Assessment Form: This instrument collects patient data to measure home health care outcomes. Its focus on accurate, complete, and timely documentation parallels the Home Health Audit form's comprehensive review of OASIS assessments and their alignment with care plans.
Compliance Checklist for Patient Privacy Rights: This checklist ensures adherence to laws and regulations regarding patient privacy, similar to how the audit form verifies the acknowledgement, receipt, and explanation of patient privacy rights, HIPAA compliances, and consent for information use.
Home Safety Evaluation Checklist: While not directly mentioned in the audit form, a home safety evaluation checklist assesses environmental safety for home health care delivery, mirroring the attention to emergency preparedness, safety instructions, and the overall focus on patient safety in the Home Health Audit form.
Dos and Don'ts
When filling out the Home Health Audit form, it's essential to follow a specific set of guidelines to ensure accuracy and compliance. Here are six things you should and shouldn't do:
- Do ensure that all information is accurate and up to date. This includes checking patient details, diagnosis codes, and care plans.
- Do verify that all required sections are completed. If a section is not applicable, mark it as N/A to indicate this clearly.
- Do obtain and document physician orders, including verbal orders, ensuring they are signed and dated within the required timeframe.
- Don't forget to review and include patient rights, privacy act statements, and emergency preparedness plans as acknowledged by the patient or caregiver.
- Don't leave out any information related to medication management, such as changes, interactions, and confirmations of medication profiles.
- Don't overlook the requirements for OASIS assessments and timely submission. Ensure these are completed, consistent, and exported within the designated period.
Misconceptions
When it comes to Home Health Medical Records Audit Forms, misconceptions are common. It's vital to debunk these myths for better understanding and compliance in home health care audits:
It's Only About Checking Boxes: Some believe the audit form is simply about ticking yes, no, or not applicable. However, it serves as a comprehensive check on the quality of care and adherence to necessary protocols and documentation standards.
Compliance with Form Equals High-Quality Care: While the form ensures minimum standards are met, compliance alone doesn't guarantee the highest quality of care. The form is a tool to aid in the process of delivering exceptional care, not the final measure of it.
Only Clinical Staff Need to Understand It: The form touches on areas such as patient rights, emergency preparedness, and insurance screening, requiring awareness and understanding across various roles within a home health agency, not just by clinical staff.
Audits Are Primarily for Punishment: The purpose of audits is to identify gaps in care or documentation to improve service quality, not to penalize. They are an opportunity for growth and enhancement of care delivery.
Electronic Records Have Made Audits Easier: While electronic health records (EHR) can streamline documentation, they don't automatically solve all compliance issues. Proper training and usage are necessary for EHRs to effectively aid in audit compliance.
Once You're Compliant, You're Always Compliant: Compliance is not a one-time achievement. Regulations and standards evolve, requiring ongoing education and adjustments to practices to maintain compliance.
Small Agencies Are Exempt from Stringent Auditing: Regardless of size, all home health agencies must adhere to the same standards and are subject to audits. There is no exemption based on the size of the agency.
Understanding these misconceptions is key to approaching Home Health Audits with the right mindset, ensuring both compliance and quality in patient care.
Key takeaways
When navigating the complexities of the Home Health Audit form, it's crucial to grasp the essentials for an accurate and compliant audit. Here are some key takeaways to ensure thoroughness and compliance:
- Diligence in Documentation: Every section of the audit form, from patient admission to discharge summaries, requires careful attention. Each entry, whether it's about medication profiles or therapy notes, must be complete and aligned with the care provided.
- Timely Physician Orders: Ensure that all physician orders, including changes or verbal orders, are signed and dated within the required timeframe. This adherence to deadlines is essential for the plan of care's validity and reimbursement.
- Accuracy in Diagnosis Coding: Diagnoses listed on the form, including primary and secondary codes, must be not only accurate but also consistent with the care ordered. This consistency supports the medical necessity of the services provided.
- Comprehensive Medication Profile: Medication profiles must be meticulously maintained, reflecting all new and changed prescriptions, including over-the-counter medications and possible interactions. Updating this profile at key intervals is crucial for patient safety.
- Verification of Homebound Status: For each visit note, the patient's homebound status must be clearly supported, highlighting the necessity and justification for home health services. This is pivotal for meeting Medicare requirements.
- Patient Rights and Emergency Preparedness: Audit forms must include acknowledgment of patient rights, emergency preparedness plans, and advanced directives to ensure compliance with healthcare regulations and patient safety protocols.
- Ongoing Coordination and Evaluation: The form should reflect continuous evaluation and adjustment of care plans, including supervision of auxiliary staff and communication with physicians about patient status and complications.
By focusing on these key aspects, healthcare providers can navigate the intricacies of the Home Health Audit with confidence, ensuring both compliance and high-quality care for patients.
Popular PDF Forms
8010-4 - Insights into the tactical preparation of FAA Field Approval requests, with a focus on the pivotal role of the comprehensive checklist.
Braden Score of 18 - This scale allows for the continuous monitoring of patients' conditions, enabling timely adjustments in care plans to better prevent the occurrence of pressure sores.