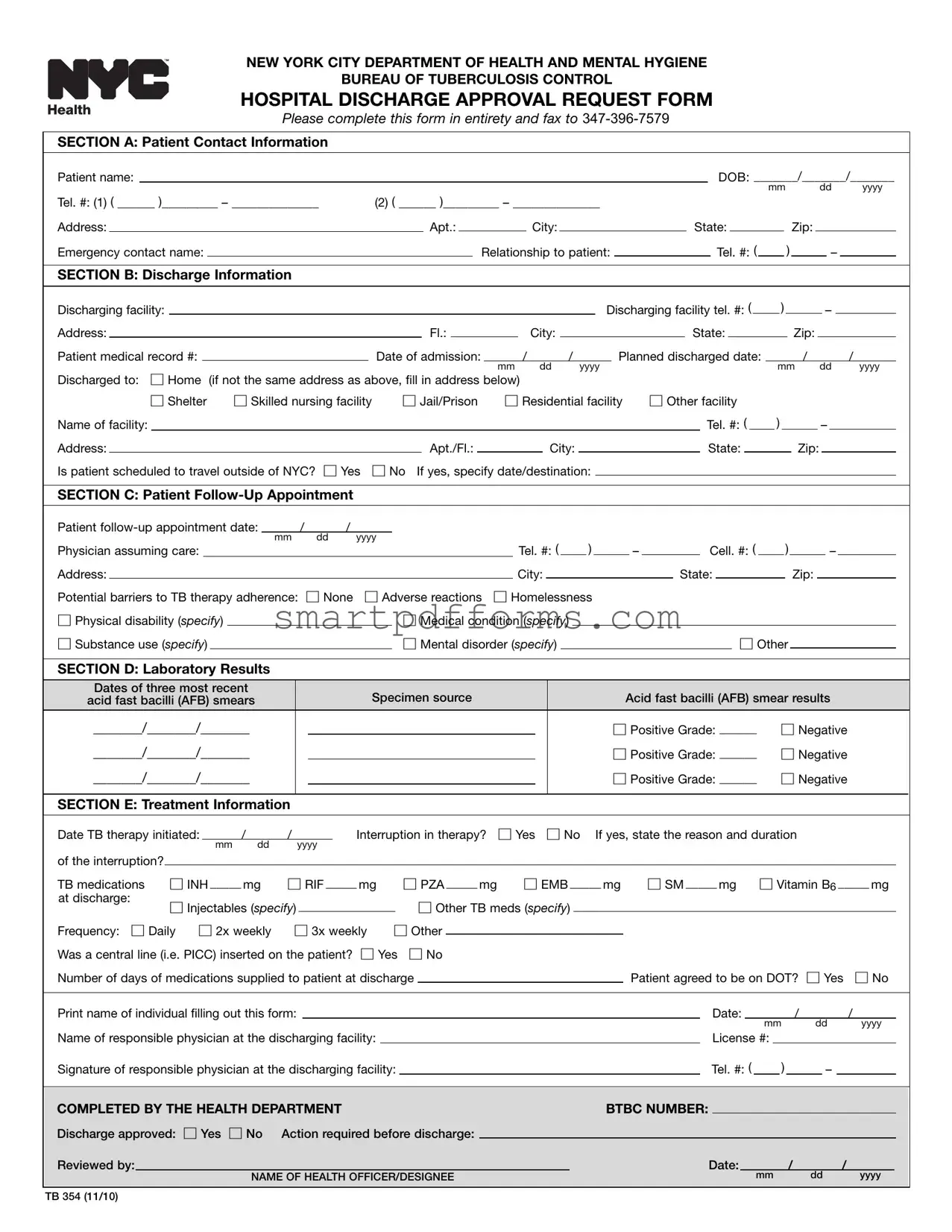
Blank Hospital Discharge Papers PDF Template
When it comes to managing the discharge of patients diagnosed with tuberculosis (TB) from hospitals, the New York City Department of Health and Mental Hygiene has set a mandated procedure through the Hospital Discharge Approval Request Form (TB 354). This form plays a crucial role in ensuring a structured and safe transition for patients from hospital care back to their community, necessitating a thorough compilation of information ranging from patient contact specifics, discharge details, follow-up appointments, laboratory results, to critical treatment information. The form notably requires health care providers to seek approval from the Department of Health & Mental Hygiene before discharging infectious TB patients, adhering to strict guidelines that involve submitting the form at least 72 hours before the anticipated discharge date. This approval system, mandated by Article 11 of the New York City Health Code since June 16, 2010, aims to mitigate the risk of TB transmission and reassert the importance of continuity in TB therapy post-discharge, demanding detailed reporting on treatment regimens, potential barriers to treatment adherence, and plans for directly observed therapy (DOT), among other requirements. Ensuring an in-depth briefing on patient follow-up and precise documentation on TB therapy, the form acts as a linchpin in the collective efforts to control TB spread, requiring a coordinated effort between discharging facilities and the Bureau of Tuberculosis Control to facilitate a discharge process that prioritizes both patient welfare and public health safety.
Preview - Hospital Discharge Papers Form
NEW YORK CITY DEPARTMENT OF HEALTH AND MENTAL HYGIENE
BUREAU OF TUBERCULOSIS CONTROL
HOSPITAL DISCHARGE APPROVAL REQUEST FORM
Please complete this form in entirety and fax to
SECTION A: Patient Contact Information
|
|
Patient name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DOB: _______/_______/_______ |
|
|
|||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
|
|
dd |
|
yyyy |
|
|
|||||||||||||||||||||
|
|
Tel. #: (1) ( ______ )_________ – ______________ |
|
(2) ( ______ )_________ – ______________ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Apt.: |
|
|
|
|
|
|
|
|
City: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
State: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
Emergency contact name: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Relationship to patient: |
|
|
|
|
|
|
|
|
|
|
|
Tel. #: ( |
|
|
|
|
|
) |
|
|
|
|
|
|
|
|
|
|
|
– |
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
SECTION B: Discharge Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Discharging facility: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Discharging facility tel. #: ( |
|
|
|
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
– |
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Fl.: |
|
|
|
|
|
|
|
City: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
State: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
Patient medical record #: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date of admission: |
|
|
/ |
|
/ |
|
|
|
|
|
|
Planned discharged date: |
|
|
/ |
|
|
|
|
|
|
|
|
|
|
|
/ |
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
dd |
yyyy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
|
|
dd |
|
yyyy |
|
|
|||||||||||||||||||||||||||||||||||
|
|
Discharged to: |
☐ Home (if not the same address as above, fill in address below) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
☐ Shelter |
☐ Skilled nursing facility |
|
|
|
|
☐ Jail/Prison |
|
☐ Residential facility |
|
|
☐ Other facility |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
Name of facility: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tel. #: ( |
|
|
|
) |
|
|
|
|
|
|
|
|
|
|
|
– |
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Apt./Fl.: |
|
|
|
|
|
|
|
|
|
City: |
|
|
|
|
|
|
|
|
|
|
|
|
|
State: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||
|
|
Is patient scheduled to travel outside of NYC? |
☐ Yes ☐ No If yes, specify date/destination: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SECTION C: Patient |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
Patient |
|
/ |
|
/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
dd |
yyyy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
Physician assuming care: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tel. #: ( |
|
|
|
|
) |
|
|
|
|
|
– |
|
|
|
|
|
Cell. #: ( |
|
|
) |
|
|
|
|
|
|
|
|
|
|
|
|
– |
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||
|
|
Address: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
City: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
State: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Zip: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
Potential barriers to TB therapy adherence: ☐ None |
☐ Adverse reactions |
☐ Homelessness |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
☐ Physical disability (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Medical condition (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
☐ Substance use (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Mental disorder (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SECTION D: Laboratory Results |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
Dates of three most recent |
|
|
|
|
|
|
|
|
|
|
|
Specimen source |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Acid fast bacilli (AFB) smear results |
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
acid fast bacilli (AFB) smears |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||
|
|
_______/_______/_______ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Positive Grade: ______ |
|
☐ Negative |
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
_______/_______/_______ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Positive Grade: ______ |
|
☐ Negative |
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
_______/_______/_______ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
☐ Positive Grade: ______ |
|
☐ Negative |
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
SECTION E: Treatment Information |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
Date TB therapy initiated: |
|
/ |
|
|
/ |
|
|
|
|
|
|
Interruption in therapy? |
|
☐ Yes |
|
☐ No |
|
|
If yes, state the reason and duration |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
mm |
dd |
|
|
yyyy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
of the interruption? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
☐ RIF _____ mg |
|
|
|
|
☐ PZA _____ mg |
|
|
☐ EMB _____ mg |
|
|
☐ SM _____ mg ☐ Vitamin B6 _____ mg |
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
TB medications |
|
|
☐ INH _____ mg |
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
at discharge: |
|
|
☐ Injectables (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
☐ Other TB meds (specify) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||
|
|
Frequency: ☐ Daily ☐ 2x weekly |
|
☐ 3x weekly |
|
|
☐ Other |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
|
Was a central line (i.e. PICC) inserted on the patient? |
☐ Yes ☐ No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||
|
|
Number of days of medications supplied to patient at discharge |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Patient agreed to be on DOT? ☐ Yes |
☐ No |
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Print name of individual filling out this form: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date: |
/ |
|
|
|
|
|
|
|
|
|
|
|
|
|
/ |
|
|
|
|
||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
dd |
|
yyyy |
|
|
||||||||||||||||||||||||
|
|
Name of responsible physician at the discharging facility: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
License #: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||
|
|
Signature of responsible physician at the discharging facility: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Tel. #: ( |
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
– |
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
COMPLETED BY THE HEALTH DEPARTMENT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
BTBC NUMBER: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||||||||
|
|
Discharge approved: ☐ Yes |
☐ No |
Action required before discharge: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
|
|
Reviewed by: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date: |
|
/ |
|
|
/ |
|
|
|
|
|
||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
NAME OF HEALTH OFFICER/DESIGNEE |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
mm |
|
|
|
|
|
|
|
|
|
|
dd |
|
yyyy |
|
|
|||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TB 354 (11/10)
Guidelines for How to Complete and Submit the Mandatory TB
Hospital Discharge Approval Request Form (TB 354)
As of June 16, 2010, Article 11 of the New York City Health Code mandates health care providers to obtain approval from the New York City Department of Health & Mental Hygiene (DOHMH) before discharging infectious TB patients from the hospital.
Discharge of an Infectious (sputum smear positive) Tuberculosis Patient
Health care providers must submit a Hospital Discharge Approval Request Form (TB 354) at least 72 hours prior to the anticipated discharge date. The DOHMH will review the form and approve or request additional information before the patient can be discharged from the health care facility.
Weekday
Weekend and Holiday Discharge: All arrangements for discharge should be made in advance when weekend or holiday discharge is anticipated.
For detailed information about hospital admission and discharge of TB patients, please refer to the New York City Department of Health and Mental Hygiene, Bureau of TB Control Policies and Protocols manual available online at
Instructions for Completing the Hospital Discharge Approval Request Form (TB 354)
Section A Patient contact information: Provide the patient’s contact information including patient’s name, a verified address and telephone numbers. In addition, include a name of an emergency contact, the contact’s relationship to the patient and the contact’s verified phone number.
Section B Discharge information: Provide the name and phone number of the discharging facility, the medical record number of the patient at the facility, date the patient was admitted, planned discharge date, and the location to which the patient is being discharged. If the patient will be discharged to a location other than the patient’s address listed in Section A, a facility name (if applicable), address and phone number must be provided. If the patient plans to travel, provide the date and destination.
Section C Patient
Section D Laboratory results: Report the results of the three most recent acid fast bacilli (AFB) smears including the date of specimen collection, specimen source, and AFB smear results and/or grade.
Section E Treatment information: Fill in the date TB treatment was initiated. If there were any treatment interruptions, indicate the reason and number of days treatment was stopped. Check the box next to each prescribed drug and state dosages for each drug. Write in drugs and dosages for drugs not specified. Specify the treatment frequency by checking one of the three boxes, or writing in a different treatment schedule. State whether the patient will have a central line inserted at the time of discharge. If TB medication will be supplied to the patient at discharge, write the number of days for which the medication will be supplied. State whether the patient agreed to be on directly observed therapy (DOT).
After Section E, the name of the person completing the form should be printed and the authorized physician at the discharging facility must print and sign their name, and provide their medical license number and telephone number.
Forms should be faxed to the DOHMH at
If you have questions about completing the form, please call 311 and ask to speak to a Bureau of Tuberculosis Control physician.
To fulfill State requirements for communicable disease reporting, health care providers must report all suspected or confirmed TB cases to the Health Department via Reporting Central (formerly Universal Reporting Form (URF)). Instructions for reporting a case of tuberculosis can be found at
NOTE: A discharge approval request form does not substitute required case reports.
TB 354 (11/10)
Form Data
| Fact Name | Description |
|---|---|
| Governing Law | Article 11 of the New York City Health Code mandates health care providers to obtain approval from the New York City Department of Health & Mental Hygiene (DOHMH) before discharging infectious TB patients from the hospital. |
| Form Objective | The Hospital Discharge Approval Request Form (TB 354) is designed to ensure that infectious TB patients are properly discharged, with arrangements made for their continued care and monitoring. |
| Prior Notice Requirement | Health care providers must submit the Hospital Discharge Approval Request Form at least 72 hours prior to the anticipated discharge date to allow the DOHMH to review and approve the discharge plan. |
| Submission Process | The form must be completed in its entirety and faxed to 347-396-7579 for the DOHMH's review and approval. |
| Sections of the Form | The form includes sections for patient contact information, discharge information, patient follow-up appointment, laboratory results, and treatment information. |
| Review and Approval Process | Upon receipt, Bureau of TB Control staff will review the discharge plan and, within 24 hours, notify the provider of approval or any further actions required before the patient can be discharged. |
| Follow-up and Reporting Requirements | In addition to discharge approval, health care providers must report all suspected or confirmed TB cases to the Health Department via Reporting Central, in compliance with state requirements for communicable disease reporting. |
Instructions on Utilizing Hospital Discharge Papers
Filling out the Hospital Discharge Approval Request Form is a critical step in the discharge process for patients diagnosed with tuberculosis. This procedure ensures that the New York City Department of Health & Mental Hygiene (DOHMH) approves the patient's release from the hospital, guaranteeing the safety and continuity of care for both the patient and the community. The form must be submitted at least 72 hours before the planned discharge date to allow the DOHMH adequate time to review and respond to the discharge plan. Here are the detailed steps on how to properly fill out this form.
- Section A - Patient Contact Information:
- Enter the patient's full name.
- Fill in the patient's Date of Birth (DOB) in the format mm/dd/yyyy.
- Provide two telephone numbers for the patient, if available.
- Write the patient's address, including apartment number, city, state, and zip code.
- Include the name, relationship to patient, and telephone number of an emergency contact.
- Section B - Discharge Information:
- State the name of the discharging facility and its telephone number.
- Provide the facility address, floor, city, state, and zip code.
- Enter the patient's medical record number and the date of admission.
- Fill in the planned discharge date in the format mm/dd/yyyy.
- Check the appropriate box to indicate where the patient will be discharged to and provide additional details if they will be discharged to an address that differs from the one provided in Section A or to another type of facility.
- If the patient is scheduled to travel outside of NYC, mark "Yes" and specify the date and destination.
- Section C - Patient Follow-Up Appointment:
- Fill in the date of the patient's follow-up appointment.
- Enter the name and contact information of the physician assuming care after discharge.
- Check any potential barriers to TB therapy adherence that apply.
- Section D - Laboratory Results:
- List the dates of the three most recent Specimen source Acid fast bacilli (AFB) smear results, including the results and/or grades.
- Section E - Treatment Information:
- Specify the date TB therapy was initiated.
- If there was an interruption in therapy, check "Yes" and provide details.
- For each TB medication at discharge, check the box, indicate the medication, and fill in the dosage.
- Select the frequency of treatment.
- Indicate if a central line was inserted on the patient by checking "Yes" or "No."
- Enter the number of days of medications supplied to the patient at discharge.
- Mark whether the patient agreed to be on directly observed therapy (DOT).
- Print the name of the individual filling out this form and the date.
- The responsible physician at the discharging facility must print and sign their name, provide their medical license number, and telephone number.
Once the form is completed, it should be faxed to the DOHMH at 347-396-7579. For any inquiries regarding the form, call 311 and ask to speak with a Bureau of Tuberculosis Control physician. It is essential to recognize that this discharge approval request form does not replace the mandatory case reports required for communicable diseases. Proper completion and timely submission of this form are essential in adhering to the legal and health protocols established for the discharge of tuberculosis patients.
Obtain Answers on Hospital Discharge Papers
Frequently Asked Questions about the Hospital Discharge Papers Form:
What is the purpose of the Hospital Discharge Approval Request Form (TB 354)?
This form is used by healthcare providers in New York City to get approval from the Department of Health & Mental Hygiene (DOHMH) before discharging patients with infectious tuberculosis (TB) from the hospital. It ensures that patients with TB are properly managed and continue their treatment after discharge.
When should the form be submitted?
The form must be sent to the DOHMH at least 72 hours before the anticipated discharge date. This timeline allows the DOHMH to review the form and respond with approval or request additional information if needed.
How should the form be submitted?
For weekday (non-holiday) discharges, the discharge plan should be faxed to the Bureau of TB Control between 8am-5pm. The Bureau staff will review the discharge plan within 24 hours. For weekend or holiday discharges, arrangements should be made in advance. The form should be faxed to 347-396-7579.
What information is required in Section A of the form?
Section A requires patient contact information, including their name, address, telephone numbers, and the name and contact information of an emergency contact.
What details are needed in Section B: Discharge Information?
This section collects detailed information about the discharging facility, patient medical record number, admission and planned discharge dates, and where the patient will go after discharge. If the patient will be discharged to a different location than the one listed, facility name, address, and phone number are required.
What should be included in Section C: Patient Follow-Up Appointment?
Provide the date of the patient’s follow-up appointment, including the contact information of the provider who will assume care. Also, identify any potential barriers that may affect the patient’s adherence to TB therapy.
How to complete Section D: Laboratory Results?
Report the dates, specimen sources, and results of the three most recent acid-fast bacilli (AFB) smears, including the grade if the result is positive.
What information is required in Section E: Treatment Information?
Detail the TB treatment information, including the start date, any interruptions in therapy, medications prescribed with dosages, treatment frequency, and if a central line was inserted. Also, specify if the patient agreed to be on directly observed therapy (DOT).
If there are questions about filling out the form, who should be contacted?
For any inquiries or clarifications while completing the form, one should call 311 and request to speak to a physician from the Bureau of Tuberculosis Control.
Remember: The approval request form is crucial for managing TB patients' care post-discharge and is a mandatory step for health care providers in New York City handling infectious TB patients.
Common mistakes
When completing the Hospital Discharge Approval Request Form, individuals often make mistakes that can impact the discharge process. Avoiding these common errors ensures a smoother transition for patients. Here are five mistakes to avoid:
-
Not providing complete patient contact information: It's crucial to fill out all sections of patient contact information accurately. This includes verifying the patient's address and providing alternative contact numbers. Omitting or inaccurately filling this section can lead to difficulties in follow-up care.
-
Skipping details in the Discharge Information section: Every detail in the Discharge Information section aids in ensuring the patient receives appropriate care post-discharge. Failing to specify the discharge location or not indicating if the patient is traveling outside of NYC can cause confusion and hinder necessary arrangements.
-
Providing incomplete follow-up appointment information: The Follow-up Appointment section is pivotal for the continuity of care. Not providing the date, the physician's name, or contact information can lead to missed follow-up appointments, impacting the patient's health.
-
Omitting Laboratory Results: Accurate laboratory results are critical for the ongoing management of the patient's condition. Neglecting to include the dates and results of the most recent Acid Fast Bacilli (AFB) smears can result in inadequate follow-up care and monitoring.
-
Inaccurate or incomplete TB Treatment Information: The Treatment Information section requires careful attention to detail. Not specifying treatment interruptions, dosages of TB medications, and the patient's agreement to Directly Observed Therapy (DOT) can significantly affect the patient's treatment plan and adherence.
To avoid these mistakes, it is advisable to review the form thoroughly before submission. Ensuring all information is accurate and complete will facilitate a better care transition for the patient.
Documents used along the form
When a patient is ready to be discharged from the hospital, a variety of forms and documents beyond the Hospital Discharge Approval Request Form may be necessary to ensure a smooth transition from hospital care to home care, another facility, or follow-up appointments. These documents each serve a specific purpose, from confirming the patient's understanding of their aftercare instructions to ensuring that any services or equipment needed for recovery are appropriately arranged. Here are ten additional forms and documents that are commonly used alongside the Hospital Discharge Papers:
- Medication Reconciliation Form: Lists all medications a patient is taking at the time of discharge, including dosage, frequency, and purpose. This document helps prevent adverse drug interactions and ensures continuity of care.
- Aftercare Instructions: Provides detailed guidelines a patient should follow after leaving the hospital, covering wound care, activity levels, dietary restrictions, signs of complications, and other personalized instructions.
- Patient Summary Form: Summarizes the patient’s hospital stay, including diagnoses, treatments received, and major procedures performed. This document is crucial for follow-up care providers.
- Follow-up Appointment Schedule: Lists dates, times, and locations for any necessary follow-up appointments with specialists or the primary care physician, ensuring continuity of care.
- Home Health Care Plan: If home care services are required, this plan describes the type and frequency of services to be provided, such as nursing, physical therapy, or home health aide visits.
- Equipment Prescription Form: Details any medical equipment prescribed for use at home, like walkers, wheelchairs, or hospital beds, including specifications for ordering and delivery.
- Advance Directives Form: Contains the patient’s living will and health care proxy information, outlining their wishes regarding medical treatment in cases where they cannot communicate their decisions.
- Patient Rights and Responsibilities: Informs patients of their rights regarding treatment and privacy, as well as their responsibilities, such as providing accurate health information and following agreed-upon treatment plans.
- Insurance Verification Form: Confirms that the patient’s insurance coverage is up-to-date and outlines which services or equipment are covered as the patient transitions out of hospital care.
- Emergency Contact Form: Lists contacts to be notified in case of an emergency, including names, relationships to the patient, and contact information.
Together with the Hospital Discharge Approval Request Form, these documents contribute to comprehensive discharge planning. They address various aspects of patient care and post-discharge support, ensuring that patients understand their care plan, know when and where their follow-up care will occur, and have access to necessary medications and equipment for a safe recovery. By preparing and reviewing these forms carefully, healthcare providers can help minimize the risk of readmission and support a smooth transition to the next phase of care.
Similar forms
Medical Records Release Form: Similar to Hospital Discharge Papers, this form involves the disclosure of patient medical information. Both require patient identification, like name and date of birth, medical details, and the healthcare provider's information but serve different purposes. Hospital Discharge Papers summarize care and treatment during a hospital stay, while a Medical Records Release Form grants permission to share detailed medical records with third parties.
Patient Referral Form: This document, like Hospital Discharge Papers, contains patient information, diagnosis, and the recommended next steps in treatment or care after the initial healthcare service. It often includes follow-up care instructions and the contact information of the medical professional or facility taking over care, mirroring the patient follow-up appointment section in the discharge papers.
Prescription Medication Form: Both Hospital Discharge Papers and Prescription Medication Forms include vital medication information. In the discharge papers, medication details at discharge are provided, including drug names, dosages, and treatment duration—similar to what's found on a standard prescription form, although within the broader context of a discharge process.
Advance Directive Form: While serving different primary functions, both the Hospital Discharge Papers and Advance Directive Forms are critical in patient care planning. An Advance Directive outlines a patient's wishes regarding treatment and end-of-life care, potentially impacting discharge planning and follow-up care included in the discharge paperwork.
Emergency Contact Form: Similar to sections in Hospital Discharge Papers that require patient and emergency contact information, this standalone form ensures healthcare providers have access to a patient's designated contacts. Both forms prioritize having a readily available contact in case of emergencies or necessary follow-up.
Infectious Disease Reporting Form: Similar to the specific TB Discharge Approval Request Form, Infectious Disease Reporting Forms are used to notify public health authorities about cases of notifiable diseases. Both include patient details, diagnosis, treatment information, and laboratory results essential for public health monitoring and control measures.
Dos and Don'ts
When completing the Hospital Discharge Approval Request Form for a tuberculosis patient, certain practices should be observed to ensure an accurate and compliant submission. Below are critical dos and don'ts:
- Do complete the form in its entirety. Skipping sections or providing incomplete information can delay the discharge process.
- Do verify the patient's contact information, including the address and telephone numbers, to avoid any issues with follow-up care.
- Do provide detailed discharge information, including the discharging facility’s name, address, and phone number, along with the patient's destination post-discharge.
- Do accurately report the patient’s follow-up appointment details and potential barriers to TB therapy adherence to help ensure the patient receives necessary post-discharge care.
- Do include precise laboratory results and treatment information, such as the dates of the three most recent AFB smears, TB therapy initiation date, medication types, and dosages.
- Don't wait until the last minute to submit the form. It must be faxed to 347-396-7579 at least 72 hours before the anticipated discharge date.
- Don't forget to print the name of the individual filling out the form and have the responsible physician at the discharging facility print and sign their name. The physician’s signature and license number are essential for the form’s validity.
- Don't fax the form outside of the Bureau of TB Control's reviewing hours if expecting a weekday discharge. The Bureau reviews plans between 8am-5pm on weekdays.
- Don't substitute this form for required case reports to health authorities. Even after completing this form, you must ensure all suspected or confirmed TB cases are reported according to State requirements.
Following these guidelines will facilitate a smoother discharge process for TB patients, ensuring that they receive the necessary post-discharge care while adhering to legal and health department requirements.
Misconceptions
There are several misconceptions regarding the Hospital Discharge Approval Request Form used by health care providers when discharging patients with tuberculosis (TB) in New York City. Understanding the truth behind these misconceptions is critical for both patients and providers to ensure a smooth discharge process and continued care.
- Misconception 1: The discharge form is optional for TB patients.
- Misconception 2: The form can be submitted at any time before discharge.
- Misconception 3: Any health care professional can complete the form.
- Misconception 4: The discharge form is only for the hospital's records.
- Misconception 5: Completing the form is the last step in the discharge process for TB patients.
This is incorrect. According to the guidelines set by the New York City Department of Health and Mental Hygiene (DOHMH), it is mandatory for health care providers to obtain approval from the DOHMH before discharging infectious TB patients. This process ensures that patients continue to receive the necessary care and treatment after they leave the hospital.
In reality, the form must be submitted at least 72 hours prior to the anticipated discharge date. This timeframe allows the DOHMH to review the form and request additional information or actions if necessary, ensuring the patient’s discharge plan is appropriate and safe.
While many sections of the form require detailed patient information, the form must be completed by a responsible physician at the discharging facility. This physician must also provide their license number and signature, verifying the accuracy of the information provided.
The form serves a much larger purpose than just being part of the patient's hospital records. It is a critical tool used by the Bureau of TB Control to monitor the patient's condition and ensure continuous treatment. Its submission and approval are integral steps in the state’s efforts to control and prevent the spread of tuberculosis.
This statement is not entirely true. While obtaining approval via the discharge form is essential, health care providers must also ensure that all necessary arrangements for the patient's continued care are in place. This includes scheduled follow-up appointments, confirmed TB therapy adherence plans, and coordination with other health care facilities if the patient is not returning home.
Eliminating these misconceptions is crucial for the proper care of TB patients and the public's health. Proper completion and understanding of the Hospital Discharge Approval Request Form enable health care providers to ensure a safe discharge process and support the ongoing treatment and monitoring of TB patients.
Key takeaways
Filling out Hospital Discharge Papers is a crucial step in ensuring the safety and continued treatment of patients being released from a hospital, especially in cases involving infectious diseases like tuberculosis (TB). Here are six key takeaways about how to accurately complete and use the Hospital Discharge Papers form.
- Ensure timely submission: The form must be submitted at least 72 hours prior to the anticipated discharge date to give the Department of Health & Mental Hygiene (DOHMH) ample time for review.
- Complete all sections fully: Every part of the form, from patient contact information to detailed treatment information, must be filled in accurately to avoid delays in the discharge process.
- Be detailed in treatment information: Include specific details about TB therapy, including medication dosages, treatment initiation dates, and any interruptions to ensure clear communication and continuity of care.
- Indicate follow-up care: Clearly state the follow-up appointment date and the physician assuming care post-discharge to ensure the patient continues to receive necessary medical attention.
- Properly report TB cases: In addition to submitting the discharge form, all suspected or confirmed TB cases must be reported to the Health Department to comply with communicable disease reporting requirements.
- Fax is the primary submission method: Completed forms should be faxed to the DOHMH at the provided fax number to ensure they are received and reviewed in a timely manner.
Understanding the importance of each section and requirement on the Hospital Discharge Papers form not only aids in the smooth transition of care for the patient but also complies with public health regulations, ultimately contributing to the containment and treatment of TB.
Popular PDF Forms
Cbu Transcript Request - Each section of the form is crucial for ensuring the accurate and secure handling of transcript requests.
Er Hamilton - By limiting the design to functional elements, the form respects user time, emphasizing a no-frills approach to ordering.