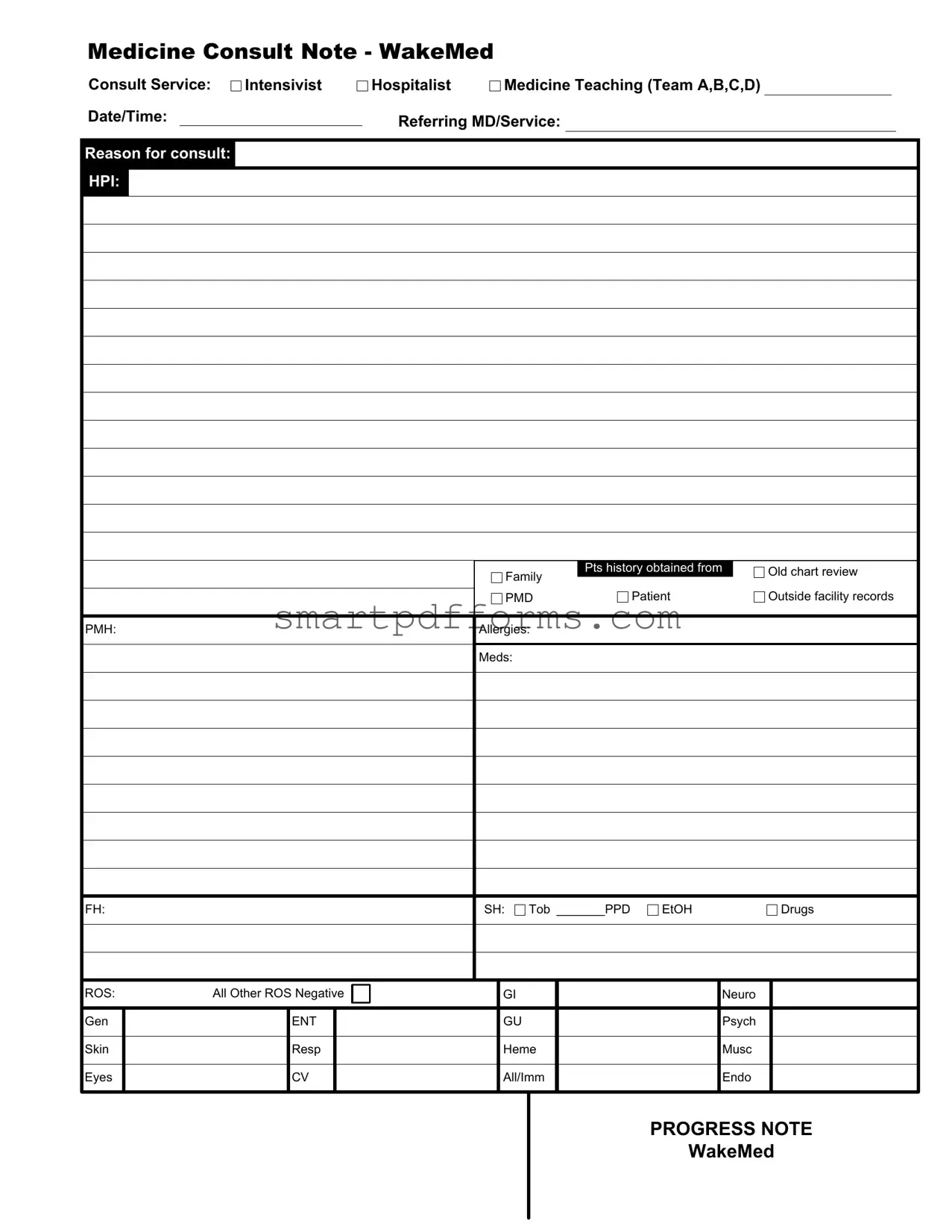
Blank Internal Medicine Progress Note PDF Template
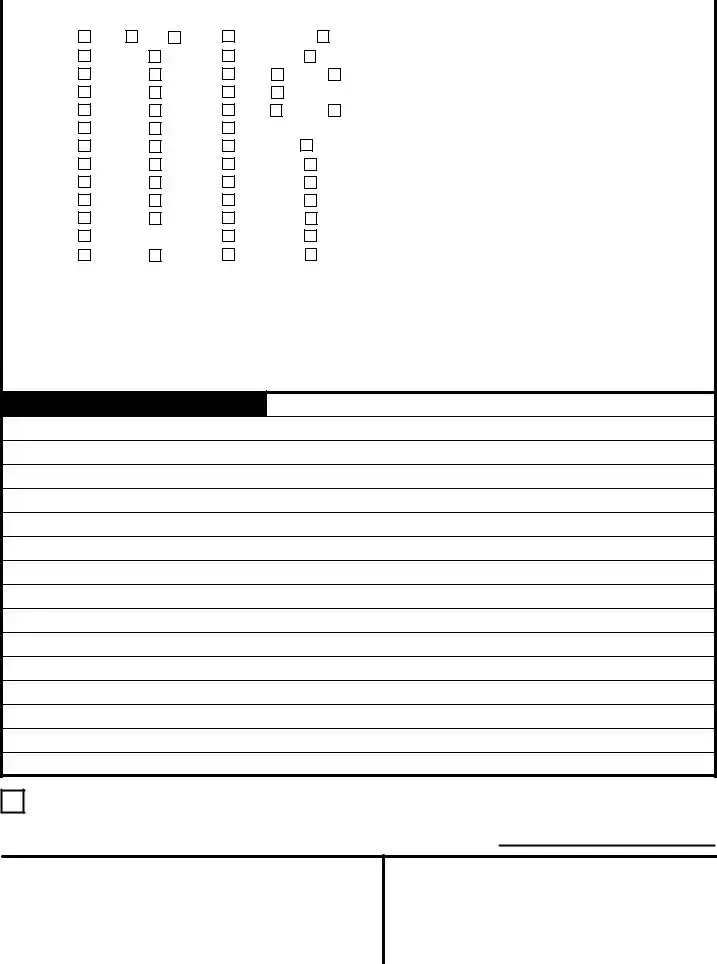
The Internal Medicine Progress Note form stands as a critical document within the realm of medical documentation, especially designed to cater to the needs of healthcare professionals in internal medicine. This structured format aids in systematically recording various aspects of patient care, including the reason for consult, history of present illness (HPI), patient and family history, review of systems (ROS), and the detailed physical examination findings. Moreover, it also encompasses the inclusion of vital signs, assessments, and recommendations made by the attending physician, alongside the documentation of labs and diagnostic tests results. Crucially, it reflects on the collaborative nature of patient care, highlighting how assessments and plans are discussed and confirmed with the attending physician, who then co-signs the document along with the resident. By encapsulating detailed patient information and healthcare interventions, this form serves as an indispensable tool for internal medicine practitioners, ensuring a comprehensive and coherent approach towards patient care and facilitating continuity of care within multidisciplinary teams.
Preview - Internal Medicine Progress Note Form

Medicine Consult Note - WakeMed
Consult Service: |
|
Intensivist |
|
Hospitalist |
|
|
|
Medicine Teaching (Team A,B,C,D) |
|
|
|
|
||||||||||||||||
Date/Time: |
|
|
|
|
|
|
Referring MD/Service: |
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Reason for consult: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
HPI: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Family |
Pts history obtained from |
|
|
|
Old chart review |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Patient |
|
|
|
|
Outside facility records |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
PMD |
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PMH: |
|
|
|
|
|
|
|
Allergies: |
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
Meds: |
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FH: |
|
|
|
|
|
|
|
SH: |
Tob _______PPD |
EtOH |
|
|
|
|
|
Drugs |
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ROS: |
All Other ROS Negative |
|
|
|
|
|
|
GI |
|
|
|
|
|
|
Neuro |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Gen |
|
|
|
|
ENT |
|
|
|
|
|
|
|
GU |
|
|
|
|
|
|
Psych |
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Skin |
|
|
|
Resp |
|
|
|
|
|
|
|
Heme |
|
|
|
|
|
|
Musc |
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Eyes |
|
|
|
CV |
|
|
|
|
|
|
|
All/Imm |
|
|
|
|
|
|
Endo |
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PROGRESS NOTE
WakeMed
Medicine Consult Note - Page 2
|
Physical Exam |
T |
|
|
|
|
|
HR |
|
|
|
|
|
|
|
|
|
|
RR |
|
BP |
POX |
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Check Normal Findings |
|
|
|
|
|
|
|
|
|
|
|
Describe Abnormalities |
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
General |
|
|
Awake |
|
Alert |
|
|
NAD |
|
|
|
Normal Habitus |
|
|
|
Obese |
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
Psych |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
Orient x 3 |
|
|
|
Nl MS |
|
|
|
Mood Nl |
|
|
|
|
|
|
Affect Nl |
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
Eyes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
Sclera Cl |
|
|
Conj Cl |
|
|
|
PERRL |
|
|
|
EOMI |
|
|
|
|
Nl Optic Disc |
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ENT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
O/P clear |
|
|
Dent. Nl |
|
|
|
TMs nl |
|
|
|
Nares Clear |
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
Neck |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
Nl appear |
|
|
No mass |
|
|
|
No LAD |
|
|
Non tend |
|
Thyroid Nl |
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
Chest |
|
|
BS nl |
|
|
No rales |
|
|
|
Work of breathing nl |
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
No rhonchi |
|
|
|
No retractions |
|
|
|
|
Nl percussion |
|
|
|
|
|||||||||||||
|
|
|
|
No wheeze |
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
Cardiac |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
RRR |
|
|
No MGR |
|
|
|
No carotid bruit |
|
|
No edema |
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
Abdominal |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
Soft |
|
|
Non tend |
|
|
|
No HSM |
|
|
|
|
|
|
No masses |
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
MSK |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
Gait nl |
|
|
Tone nl |
|
|
|
No cyan/club |
|
|
Nl joints |
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
Neuro |
|
|
Nl sensation |
|
|
RAM nl |
|
|
|
CN |
|
|
|
|
|
|
Finger to nose nl |
|
|
|
|
||||||||||||||
|
|
|
Strength nl |
|
|
|
|
|
|
DTRs nl |
|
|
|
|
|
|
No Babinski |
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
Skin |
|
|
|
|
|
|
|
|
Nl palpation |
|
|
|
|
|
|
No induration |
|
|
|
|
|||||||||||||||
|
|
|
No lesions |
|
No rash |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Labs & Diagnostic Tests |
|
Blood gluc:_______________________________________________________ |
|||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Assessment/Recommendations:
I, the attending physician, saw and evaluated this patient. The findings and assessment/plan were discussed and confirmed. I agree with the above documentation with any addendums noted.
Attending Signature |
|
Resident Signature |
|
|
|
PROGRESS NOTE
WakeMed
Form Data
| Fact Name | Description |
|---|---|
| Form Usage | Used by physicians to document consultations in internal medicine at WakeMed. |
| Consult Services Included | Intensivist, Hospitalist Medicine, and Teaching Teams (A, B, C, D). |
| Key Components | Includes sections on patient history, physical exam findings, and assessments with recommendations. |
| Information Sources | Data is gathered from multiple channels including the old chart review, patient, outside facility records, and the Primary Managing Doctor (PMD). |
| Document Structure | Structured in a two-page format with initial patient information and history on the first page, and physical exam details along with labs, diagnostics, and assessments on the second. |
| Physical Exam Checks | A comprehensive examination that includes general appearance, psychological state, cardiovascular, respiratory, gastrointestinal, musculoskeletal, neurological evaluations, and more. |
| Labs & Diagnostic Tests | Suggests inclusion of blood glucose levels but provides a format for additional tests. |
| Assessment and Recommendations | Allows physicians to document their findings, suggested plans, and any follow-up actions recommended. |
| Signature Requirement | Both the attending physician and the resident involved in the consult must sign the document, ensuring accountability and agreement on the documented findings and plans. |
Instructions on Utilizing Internal Medicine Progress Note
Filling out the Internal Medicine Progress Note is a crucial step in ensuring that the patient's medical history, present condition, and the consultation process are comprehensively recorded. This document is a fundamental tool used by healthcare providers to communicate vital information. It is typically utilized following a consultation with an internal medicine specialist. As you embark on completing this form, remember that accuracy and clarity are key to effective communication among healthcare professionals. Below are the steps you need to take to fill out this form accurately.
- Start with the Medicine Consult Note section at the top. Check the appropriate box to indicate the consult service needed (Intensivist, Hospitalist, Medicine Teaching Team A, B, C, or D).
- Fill in the Date/Time field with the current date and time.
- Under Referring MD/Service, write the name of the physician or the medical service referring the patient for consultation.
- Record the specific Reason for consult in the provided space to ensure the consulting physician understands the consultation's purpose.
- The HPI (History of Present Illness) section should detail the patient’s presenting symptoms and the duration of these symptoms. This section can also include relevant information on how symptoms have progressed.
- For the patient's history, check the appropriate source of the history (e.g., Family, Pts history obtained from, Old chart review, Outside facility records, PMD) and fill in specific details such as PMH (Past Medical History), Allergies, current Medications (Meds), Family History (FH), and Social History (SH), including tobacco use (Tob), alcohol use (EtOH), and drug use.
- In the Review of Systems (ROS), mark all that apply and specify any other systems reviewed with findings under "All Other ROS Negative."
- On the second page, under Physical Exam, check "Normal Findings" or "Describe Abnormalities" for each assessed body system. This includes General appearance, Psychological state, Eyes, ENT (Ear, Nose, Throat), Neck, Chest, Cardiac, Abdominal, MSK (Musculoskeletal), Neurological, and Skin evaluations.
- Record the results of any Labs & Diagnostic Tests conducted, such as blood glucose levels.
- In the Assessment/Recommendations section, detail the attending physician's findings, the assessments made, and any recommended plans for the patient.
- Finally, the attending physician and resident should provide their signatures at the bottom of the form to confirm that they have seen, evaluated the patient, and agreed with the documented findings and assessment/plan.
Upon completing the Internal Medicine Progress Note form, it should be filed with the patient's medical records and shared with the appropriate healthcare team members. This ensures continuity of care by providing a clear and comprehensive account of the patient's current medical status and the recommended next steps in their treatment plan.
Obtain Answers on Internal Medicine Progress Note
Frequently Asked Questions about the Internal Medicine Progress Note Form
- What is the purpose of the Internal Medicine Progress Note form?
- Who completes the Internal Medicine Progress Note form?
- What is included in the "HPI" section of the form?
- How is the "Physical Exam" section of the form structured?
- What does "ROS" stand for, and what does it include?
- Can you explain the "Labs & Diagnostic Tests" section?
- What is the significance of the attending and resident signatures?
This form serves as a detailed record for patients seen by the internal medicine team. It covers the consultation's purpose, patient history, physical examination findings, lab and diagnostic test results, and the assessment and recommendations by the attending physician. This comprehensive documentation ensures continuity of care and facilitates clear communication among healthcare providers.
Both the attending physician and the resident involved in the patient's care are responsible for filling out the form. The attending physician must review, confirm, and agree with the documentation, including any addendums made by the resident physician.
The "HPI" or History of Present Illness section includes details about the reason for the current consultation, capturing information from various sources such as family, patient, old chart review, outside facility records, and the Primary Medical Doctor (PMD). This part provides context for the current health issue being addressed.
In the physical exam section, both normal findings and abnormalities must be noted across various systems, including general appearance, psychological state, ENT (Ear, Nose, Throat), cardiovascular, respiratory, abdominal, musculoskeletal, neurological, and dermatological aspects. This comprehensive review allows for a detailed assessment of the patient's physical condition.
"ROS" stands for Review of Systems. This is a thorough checklist that includes gastrointestinal, neurological, genitourinary, ENT, psychiatric, skin, respiratory, hematological, musculoskeletal, ocular, cardiovascular, immunological, and endocrinological systems. The form states if all other reviewed systems are negative, which helps to streamline the patient's medical history review.
This section is designated for entering results from blood glucose tests and any other relevant laboratory or diagnostic testing that has been performed. It is crucial for diagnosing, monitoring, and making informed decisions about the patient's care plan.
The signatures of the attending physician and the resident confirm that both have reviewed, discussed, and agreed upon the documented findings and the proposed assessment and recommendations. This step ensures accountability and the accuracy of the information recorded on the progress note.
Common mistakes
When completing the Internal Medicine Progress Note, it's essential for healthcare professionals to navigate this detailed documentation with precision and care. Despite the best intentions, common mistakes can occur, potentially impacting patient care and the accuracy of the medical record. Here are five errors often made on these forms:
Failing to update the date and time for each entry. This critical piece of information provides context for the progress note, establishing when the observation or intervention took place. A missing or incorrect date and time can lead to confusion about the sequence of events in the patient's care.
Omitting detail in the reason for consult. A vague description lacks the specificity required for subsequent caregivers to understand the initial concern fully. Detailed documentation ensures a more seamless continuity of care, allowing team members to grasp the situation's urgency and complexity.
Not specifying allergies and medications accurately. Overlooking this information can result in dangerous medication errors or allergic reactions. Each drug and allergy must be comprehensively listed with the correct dosages and reactions to ensure patient safety.
Skipping sections of the review of systems (ROS) and physical examination. If portions are left incomplete because they’re deemed irrelevant, it creates gaps in patient history. Even negative findings provide valuable information, painting a complete picture of the patient's health status. Noting all systems, even when findings are negative, ensures comprehensive patient evaluation.
Inaccurate or incomplete documentation of assessment and recommendations. This part of the note is vital for planning patient care. Ambiguities or omissions can hinder the care plan’s effectiveness, complicate follow-up, and potentially affect outcomes. Clear, concise documentation of the healthcare provider's findings and plans for follow-up or treatment is essential.
These mistakes, while seemingly minor, can have significant implications for patient care and legal compliance. Health professionals should exercise diligence and attention to detail when filling out the Internal Medicine Progress Note, ensuring every section is accurately and thoroughly completed. Adopting a meticulous approach to documentation can help improve patient outcomes, enhance communication among care teams, and maintain compliance with healthcare regulations.
Documents used along the form
In the realm of healthcare, especially within internal medicine, the Internal Medicine Progress Note form represents a crucial document for patient care. This form is detailed in capturing a patient's visit, including observations and treatment plans. However, it is part of a broader ecosystem of documents and forms that work in concert to ensure comprehensive patient care and documentation. These complementing documents each serve a specific function, enhancing the care process and facilitating communication among healthcare professionals.
- Medication Administration Record (MAR): This document is essential in the healthcare setting, as it tracks the administration of medications to a patient. It includes information about the specific medication, dose, route of administration, and time. The MAR is crucial for ensuring medication safety and efficacy.
- Admission History and Physical Examination (H&P) Form: This form is completed when a patient is admitted to a hospital. It documents the patient's current complaints, medical history, review of systems, physical examination findings, and the initial plan of care. It serves as the foundation for the patient's hospital record.
- Discharge Summary: At the conclusion of a patient's hospital stay, the discharge summary provides a comprehensive overview of their hospitalization. It covers the reason for admission, significant findings, procedures performed, treatment rendered, condition at discharge, and post-discharge care instructions.
- Physician Orders: This encompasses all orders written by physicians during a patient’s stay in the hospital, including medications, laboratory tests, procedures, diet, and activity level. It's critical for implementing the patient's treatment plan.
- Consultation Reports: When a specialist's input is needed on a patient's condition, a consultation report is generated. It describes the consultant's findings, opinions, and recommendations, enriching the comprehensive care of the patient.
- Advanced Directives: These legal documents record a patient's preferences regarding treatments they want or don't want to receive in the event they become unable to communicate their wishes. It ensures that the healthcare team respects the patient’s autonomy and decisions regarding their health care.
Together, these documents form a tapestry of patient information that allows healthcare professionals to deliver personalized, informed care. Ensuring these forms are properly completed and integrated into patient care not only enhances the quality of care but also supports the communication among the different members of the healthcare team. As healthcare continues to evolve with technological innovations, the essence of documenting comprehensive patient information remains a cornerstone of quality care.
Similar forms
Admission Notes: Similar to the Internal Medicine Progress Note, this document outlines the initial assessment and plan for a patient upon being admitted to a hospital. Both capture essential patient history details, including previous medical history (PMH), allergies, and medications (Meds), but the Admission Note specifically focuses on the reason for the current hospital admission and initial care plan.
Discharge Summary: This document, while aimed at summarizing a patient's hospital stay upon release, shares similarities with the Progress Note through its inclusion of a comprehensive review of the patient’s hospital course, including diagnostic findings, treatment received, and patient status at discharge. Both documents ensure continuity of care by providing detailed medical information.
Surgical Operation Notes: These notes, detailing the procedures and findings during surgery, also contain pre-operative and post-operative diagnoses, similar to how the Progress Note includes assessments and recommendations. Both document types are essential for communicating the patient’s condition and the interventions made by healthcare professionals.
SOAP Notes (Subjective, Objective, Assessment, Plan): SOAP Notes are used by healthcare providers to document patient visits, mirroring the structure of the Internal Medicine Progress Note by separating subjective patient-reported information from objective findings, assessments, and recommended plans for care.
Transfer Notes: Like Progress Notes, Transfer Notes are crucial when a patient is being moved from one healthcare setting to another. They include detailed patient information, reason for transfer, and medical history, ensuring the receiving facility or team is fully aware of the patient’s needs and current condition.
Nursing Notes: Nursing Notes document ongoing patient evaluations, similarly including observations on physical exams and any changes in condition. While the focus may be more on day-to-day care and response to treatment, both types of notes are integral in providing a comprehensive picture of a patient’s health journey.
Radiology Reports: These reports offer detailed findings from imaging studies, akin to the "Labs & Diagnostic Tests" section of the Internal Medicine Progress Note. Both are essential for diagnosing and monitoring treatment progress, capturing key data points that inform patient care decisions.
Multidisciplinary Team Meeting Notes: These notes summarize discussions about patient care among various healthcare professionals. They encapsulate collective assessments and plans, similar to how the Internal Medicine Progress Note may be used to document consensus or shared decisions in a patient’s care trajectory.
Anesthesia Records: Documenting the administration of anesthesia and patient monitoring during procedures, these records share the progress note's goal of chronicling clinical interventions and patient responses, ensuring a continuous record of care during specific interventions.
Prescription Records: While primarily documenting medications prescribed and dispensed, these records also convey important patient care elements reflected in the Progress Note, especially in the "Meds" section, including allergies and responses to medications that inform treatment planning.
Dos and Don'ts
Filling out an Internal Medicine Progress Note form is an essential task for healthcare professionals. It requires attention to detail and accuracy to ensure that patient care is effectively communicated. Here are five things you should and shouldn't do to ensure the form is completed properly.
Things You Should Do
- Verify patient information: Always double-check to make sure you are documenting on the correct patient's form. Mistakes in patient identification can lead to serious errors in care.
- Be precise and thorough when documenting: Explain medical terms in a way that can be universally understood within the medical community. Avoid ambiguity to ensure that the patient's condition is clearly communicated.
- Use legible handwriting or, if possible, type the information: This helps to avoid misunderstandings and ensures that anyone reading the notes can interpret them correctly.
- Include specific details about the patient's progress: Rather than using general statements, provide concrete information such as changes in medication dosage, patient responses, or specific symptoms observed.
- Review and update the form regularly: Patient conditions can change rapidly. Keeping the progress notes up-to-date ensures that all team members are aware of the patient's current status.
Things You Shouldn't Do
- Leave sections blank: If a section does not apply, note it as such (e.g., "N/A" for not applicable). Empty sections can lead to confusion or the assumption of oversight.
- Use jargon or abbreviations that may not be universally understood: Stick to common medical abbreviations and terms to ensure clarity across all healthcare professionals involved in the patient's care.
- Forget to sign and date the form: Authentication of the notes is crucial. It confirms that the attending physician or resident has reviewed and agreed with the documented information.
- Include irrelevant personal opinions or information: Focus on clinical findings, assessments, and recommendations. Personal judgments about the patient should never be part of medical records.
- Ignore abnormalities: If any tests or observations reveal abnormalities, they must be clearly stated and addressed in the patient's care plan.
By following these guidelines, healthcare professionals can ensure that the Internal Medicine Progress Note form serves its purpose as a clear, accurate, and useful document in the patient's medical record.
Misconceptions
When it comes to understanding the Internal Medicine Progress Note used in hospitals, several misconceptions can lead to confusion. Here, we aim to clarify some of these to ensure accurate knowledge.
- Misconception 1: The Progress Note is only for the medical staff.
This misunderstanding might make patients and their families feel excluded from the care process. In reality, while the primary audience is indeed medical professionals, the information within these notes has a significant impact on patient care. They are a cornerstone in ensuring continuity of care, where a clear record of a patient's condition and treatment plan is accessible to any attending healthcare provider. Engaging patients and families in discussing these notes can enhance understanding and involvement in the care process.
- Misconception 2: Everything written in the Progress Note is permanent and cannot be changed.
It's important to recognize that a Progress Note is a living document. While it contains factual, time-stamped entries about patient care, there are scenarios where addendums or corrections are necessary. If new information comes to light or if an error is identified, healthcare providers can update the note accordingly to ensure it accurately reflects the patient's situation.
- Misconception 3: Only doctors are responsible for contributing to the Progress Note.
While the attending physician and resident doctors often make the most significant contributions, many others involved in patient care also play a role. Nurses, specialists, and other healthcare professionals may all add relevant information to provide a comprehensive view of the patient's care journey. Each member contributing to the Progress Note ensures a multidisciplinary approach to patient treatment and monitoring.
- Misconception 4: The more detailed a Progress Note, the better.
Quality over quantity is a guiding principle. While detailed information is crucial, excessively lengthy Progress Notes can make it difficult to quickly ascertain a patient's current condition and care plan. The focus should be on clarity, relevance, and conciseness, ensuring that those who read the notes can efficiently comprehend the essential aspects of the patient's care.
- Misconception 5: The assessment and recommendations section is only the attending physician's responsibility.
This section certainly requires the attending physician's insight, as they oversee the patient's care plan. However, it's often a collective effort where input from the resident doctors and sometimes other specialists is incorporated. This collaborative approach helps in forming a well-rounded assessment and a more effective patient care plan.
- Misconception 6: Progress Notes are irrelevant after the patient is discharged.
Even after discharge, Progress Notes retain their significance. They provide valuable insights for outpatient providers continuing the patient's care, assist in auditing and quality control processes, and are crucial in case of readmission. Understanding the care received during hospitalization through these notes allows for a smoother transition to outpatient treatment and helps inform ongoing care strategies.
Key takeaways
Filling out and using the Internal Medicine Progress Note form is an essential task for professionals in the healthcare field. Here are key takeaways to ensure the form is used effectively:
- Ensure accuracy when recording the consult service type, such as Intensivist, Hospitalist, or Teaching Team. This provides clarity on the caregiving context.
- Documenting the Date/Time of the consultation accurately is crucial for maintaining an organized and timely medical record.
- Identification of the Referring MD/Service and the Reason for consult offers insights into the rationale behind the consultation, facilitating better coordinated care.
- The HPI (History of Present Illness) section should be comprehensive, including information obtained from various sources like old charts, patient families, outside facilities, or the primary care provider.
- Accurate documentation of the patient's PMH (Past Medical History), Allergies, Medications, Family History (FH), and Social History (SH), including tobacco, alcohol, and drug use, lays the foundation for understanding the patient's baseline and potential risk factors.
- Completing the Review of Systems (ROS) thoroughly, while noting all negative responses with a focus on systems directly relevant to the current medical issue, supports comprehensive patient assessment.
- The Physical Exam section seeks detailed observations about the patient's condition, including general appearance, vital signs, and system-specific examinations. Normal findings and abnormalities should be clearly noted.
- Labs & Diagnostic Tests results should be recorded accurately to support the assessment and recommendations. They provide objective data that guide clinical decision-making.
- The Assessment/Recommendations section is critical for summarizing the clinician's evaluation, presenting a diagnosis or differential diagnoses, and outlining the care plan, including follow-up and any specific treatment recommendations. Ensuring that the attending physician agrees with the documentation and any addendums noted, validated by their signature, underscores the collaborative and verified nature of patient care.
Adhering to these key takeaways when filling out the Internal Medicine Progress Note ensures that patient care is documented thoroughly and accurately, aiding in the provision of high-quality healthcare.
Popular PDF Forms
Vehicle Inspection Forms - Underline the importance of an operational interior before departure, checking everything from the fuel level to the heat/defrost/AC system.
Dj-le-330 - By providing a space for applicants to explain their reasons for pursuing a career in law enforcement, the form helps identify those with a genuine commitment to public service.