Blank Mc 371 PDF Template
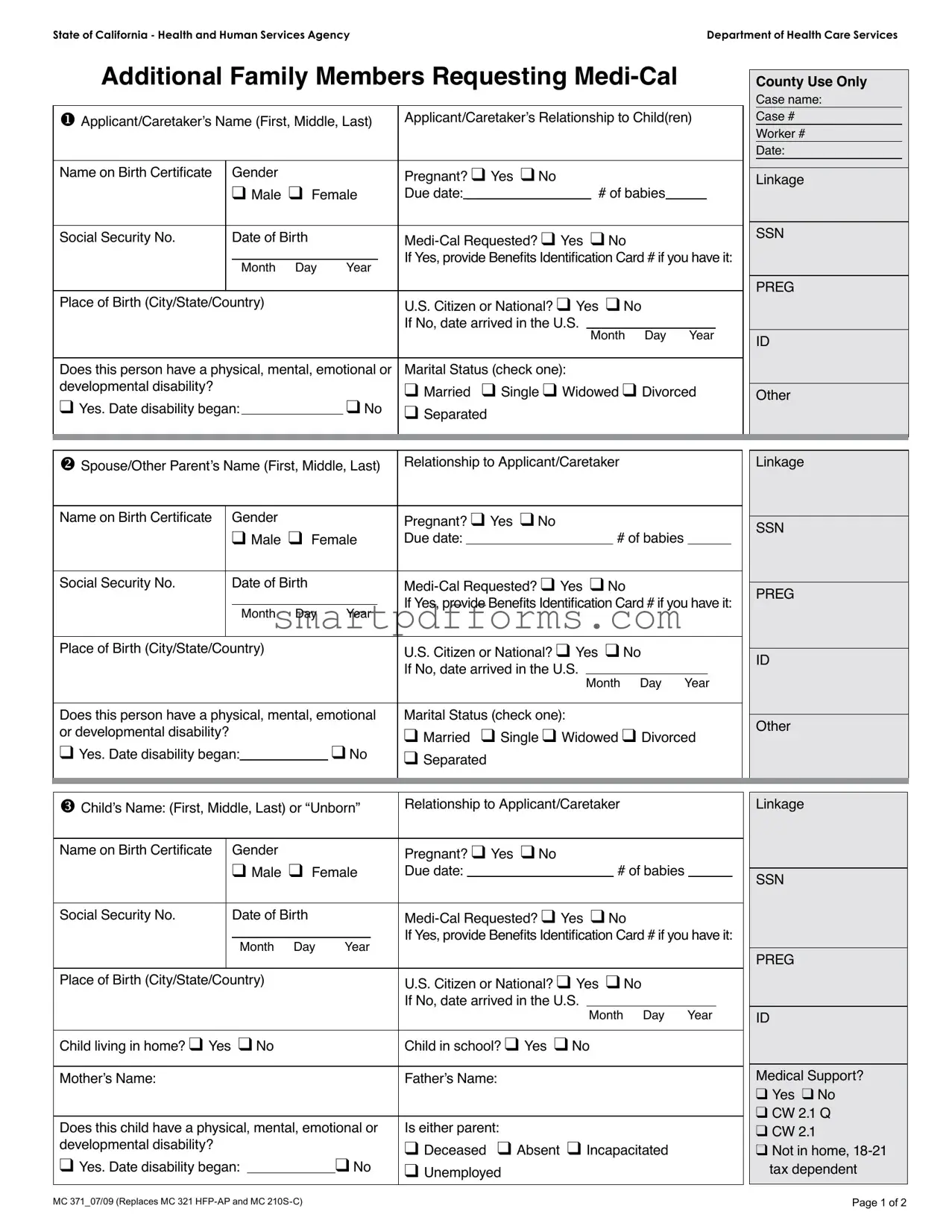
Embarking on the journey to secure Medi-Cal coverage for additional family members marks a pivotal step towards ensuring that everyone has access to essential healthcare services. The State of California - Health and Human Services Agency’s Department of Health Care Services provides a comprehensive form known as the MC 371, designed specifically for families looking to include more members under their Medi-Cal benefits. This form delves into extensive details about each new applicant, ranging from basic information such as names and birthdates, to more nuanced data like marital status, disabilities, and even the presence of health or dental insurance. Moreover, it tackles questions about U.S. citizenship or national status, the applicant's relationship to the caretaker, and potential eligibility for retroactive coverage of medical expenses. The form doesn’t stop at gathering data; it also inquires about family income and monthly expenses to gauge the financial landscape of the household. Meanwhile, it offers applicants a choice regarding the sharing of their information with related health programs like Healthy Families, ensuring a tailored approach to meeting the healthcare needs of Californians. Through completing the MC 371 form, families embark on a structured pathway to access the necessary medical support, highlighting the state’s commitment to health and well-being for all residents.
Preview - Mc 371 Form
State of California - Health and Human Services Agency |
Department of Health Care Services |
Additional Family Members Requesting
u Applicant/Caretaker’s Name (First, Middle, Last) |
Applicant/Caretaker’s Relationship to Child(ren) |
|||||||
|
|
|
|
|
|
|
|
|
Name on Birth Certiicate |
Gender |
|
|
Pregnant? q Yes q No |
||||
|
|
q Male q Female |
Due date: _______________ # of babies_____ |
|||||
|
|
|
|
|
|
|
|
|
Social Security No. |
|
Date of Birth |
|
|
||||
|
|
|
|
|
|
If Yes, provide Beneits Identiication Card # if you have it: |
||
|
|
Month Day |
Year |
|||||
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
Place of Birth (City/State/Country) |
|
|
U.S. Citizen or National? q Yes q No |
|||||
|
|
|
|
|
|
If No, date arrived in the U.S. |
|
|
|
|
|
|
|
|
|
Month Day Year |
|
|
|
|
|
|
|
|
||
Does this person have a physical, mental, emotional or |
Marital Status (check one): |
|||||||
developmental disability? |
|
|
|
|
|
q Married q Single q Widowed q Divorced |
||
q Yes. Date disability began: |
|
q No |
q Separated |
|||||
|
||||||||
|
|
|
|
|
|
|
|
|
County Use Only
Case name:
Case #
Worker #
Date:
Linkage
SSN
PREG
ID
Other
v Spouse/Other Parent’s Name (First, Middle, Last) |
Relationship to Applicant/Caretaker |
|
|
|
|
|
Linkage |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Name on Birth Certiicate |
|
Gender |
|
|
Pregnant? q Yes q No |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
SSN |
||||||
|
|
q Male q Female |
Due date: |
|
|
|
# of babies |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Social Security No. |
|
Date of Birth |
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
PREG |
||||||||
|
|
|
|
|
|
If Yes, provide Beneits Identiication Card # if you have it: |
|
|||||||||
|
|
|
|
|
|
|
|
|||||||||
|
|
|
Month Day |
Year |
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Place of Birth (City/State/Country) |
|
|
U.S. Citizen or National? q Yes |
q No |
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
ID |
|||||||||
|
|
|
|
|
|
If No, date arrived in the U.S. |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
Month Day |
Year |
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Does this person have a physical, mental, emotional |
Marital Status (check one): |
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
Other |
|||||||||
or developmental disability? |
|
|
|
|
q Married q Single q Widowed q Divorced |
|
||||||||||
|
|
|
|
|
|
|||||||||||
q Yes. Date disability began: |
q No |
q Separated |
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
w Child’s Name: (First, Middle, Last) or “Unborn” |
Relationship to Applicant/Caretaker |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
Name on Birth Certiicate |
Gender |
|
Pregnant? q Yes q No |
|
|
|
|
|
|||
|
q Male q Female |
Due date: |
|
|
|
# of babies |
|
|
|
||
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
Social Security No. |
Date of Birth |
|
|||||||||
|
_____ _____ ______ |
If Yes, provide Beneits Identiication Card # if you have it: |
|||||||||
|
Month Day |
Year |
|||||||||
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
Place of Birth (City/State/Country) |
|
U.S. Citizen or National? q Yes |
q No |
||||||||
|
|
|
|
If No, date arrived in the U.S. |
|
|
|
|
|
|
|
|
|
|
|
|
|
Month Day Year |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
Child living in home? q Yes q No |
|
Child in school? q Yes q No |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
Mother’s Name: |
|
|
|
Father’s Name: |
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
Does this child have a physical, mental, emotional or |
Is either parent: |
|
|
|
|
|
|||||
developmental disability? |
|
|
|
q Deceased q Absent q Incapacitated |
|||||||
q Yes. Date disability began: |
q No |
q Unemployed |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
Linkage
SSN
PREG
ID
Medical Support? q Yes q No
q CW 2.1 Q q CW 2.1
qNot in home,
MC 371_07/09 (Replaces MC 321 |
Page 1 of 2 |
x |
Is anyone currently covered by health/dental insurance or Medicare? q Yes q No |
q DHCS 6155 |
|
|
|
|
||||||||||||||
|
If so, who? |
|
|
|
|
|
OHC Code: |
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
y |
Has anyone iled a lawsuit because of an accident or injury? q Yes q No |
q DHCS 6268 |
|
|
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
z Do you or any family member want |
q MC 210 A |
|
|
|
|
|||||||||||||||
|
and wish to apply for |
|
|
|
|
|
Retroactive Coverage |
|||||||||||||
|
List name(s): |
Month(s) of coverage: |
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
Month |
Month |
|
Month |
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
1 |
|
|
2 |
3 |
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Have you or any family member ever been in U.S. military service? q Yes q No |
q CW 5 |
|
|
|
|
|
|
||||||||||||
|
If Yes, who? Name(s): |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
Relationship: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
The |
|
|
|
|
|
|
|
|
|
|
||||||||||
|
• |
We will share your child’s application with Healthy Families if your child no longer qualiies for free |
||||||||||||||||||
do not want us to share it, check here q
• We will share your child’s application with Healthy Kids or similar county program if your child does not qualify for
Family Income: List the income of every person listed in this application. Include child support and spousal support received. (Use a separate line for each source of income.)
Name of person with Income |
Source of Income |
How often is income |
How much is |
Social Security No. |
(Children who are in school do not have to list |
(Job, social security, |
received? |
the income? |
(Optional) |
their income from a job.) |
pension, etc.) |
(Weekly, biweekly, monthly) |
(Total gross |
|
|
|
|
income) |
|
|
|
|
|
|
|
|
|
$ |
|
|
|
|
|
|
|
|
|
$ |
|
|
|
|
|
|
|
|
|
$ |
|
|
|
|
|
|
|
|
|
$ |
|
|
|
|
|
|
|
|
|
$ |
|
|
|
|
|
|
Expenses: List the monthly expenses for all persons listed above.
Child Day Care or Disabled Dependent Care
For (child or dependent’s name):__________________________________________ Age: ______ Amount Paid: _____________
How Often?______________
For (child or dependent’s name):__________________________________________ Age: _______ Amount Paid: ____________
How Often? _____________
Paid to: ________________________________ Paid by: _________________________________ Amount paid:_____________
Paid to: ________________________________ Paid by: _________________________________ Amount paid:_____________
Please note that additional information about your property, income and/or resources may be required if applicable.
I certify that I have read and understand the information above. I also certify that the information I have given on this form is true and correct.
Signature_____________________________________________________________________ Date: ________________
MC 371_07/09 (Replaces MC 321 |
Page 2 of 2 |
Form Data
| # | Fact Name | Description |
|---|---|---|
| 1 | Form Title | MC 371 - Additional Family Members Requesting Medi-Cal |
| 2 | Governing Body | State of California - Health and Human Services Agency, Department of Health Care Services |
| 3 | Form Purpose | To request Medi-Cal for additional family members |
| 4 | Governing Law | Health Care Services in the State of California |
| 5 | Form Revision | Replaces MC 321 HFP-AP and MC 210S-C |
| 6 | Form Sections | Applicant Information, Family Member Details, Disability Information, Marital Status, Insurance, Legal, Income, and Expenses |
| 7 | Unique Features | Allows for the inclusion of pregnancy status and number of babies expected |
| 8 | Privacy Notice | Option to refuse sharing of application information with Healthy Families or similar county programs |
| 9 | Income and Expense Reporting | Requires detailed listing of family income sources and monthly expenses |
| 10 | Certification | Applicants must certify the truthfulness and correctness of the information provided |
Instructions on Utilizing Mc 371
Filling out the MC 371 form is a critical step for individuals in California looking to add family members to their Medi-Cal benefits. This document is used to gather necessary information regarding the additional family members seeking Medi-Cal assistance. Completing this form accurately ensures that the Department of Health Care Services has all the required details to process the application effectively.
Steps to Fill Out the MC 371 Form:- Start by entering the applicant/caretaker’s full name (first, middle, last) in the designated area.
- Specify the applicant/caretaker’s relationship to the child(ren) being added.
- For each child or family member being added, provide their name as it appears on their birth certificate.
- Indicate the gender of the child or family member by checking the appropriate box for male or female.
- If the individual is pregnant, check "Yes" and provide the due date and the number of babies expected.
- Enter the Social Security Number and Date of Birth (Month, Day, Year) for each person.
- Mark "Yes" or "No" to indicate if Medi-Cal is being requested for that individual. If "Yes", provide the Benefits Identification Card number if available.
- Fill in the Place of Birth (City/State/Country), and specify if the individual is a U.S. Citizen or National. If "No", state the date of arrival in the U.S.
- Check the marital status that applies to each adult being added to the form.
- Answer if the person has any physical, mental, emotional, or developmental disabilities by marking "Yes" or "No". If "Yes", include the date the disability began.
- For the "County Use Only" section, leave it blank as it will be filled by the department.
- Provide information about the spouse or other parent (if applicable), including their full name, relationship to the applicant/caretaker, and other relevant details as earlier steps suggest.
- Detail any children’s information, including living, schooling status, and if they have any disabilities. Also, specify the parent’s status if they are deceased, absent, incapacitated, or unemployed.
- Answer whether anyone in the household is covered by health/dental insurance or Medicare.
- Indicate if anyone has filed a lawsuit due to an accident or injury.
- State if there’s a desire for Medi-Cal to cover medical expenses in the last three months and list any family members also seeking coverage.
- Disclose if any family member has ever been in U.S. military service.
- Choose whether to authorize sharing the application with Healthy Families or similar programs.
- List family income details for every person included in this application, specifying the source of income, frequency, and the total gross income.
- Itemize monthly expenses, such as child daycare or disabled dependent care, court-ordered child support, and spousal support.
- Review the form to ensure all information is accurate, then sign and date the certification at the bottom of the second page.
Once the MC 371 form is thoroughly completed and signed, it should be submitted to the relevant department as instructed. This form is a crucial document for managing and updating Medi-Cal benefits for additional family members, ensuring that they receive the healthcare assistance they need.
Obtain Answers on Mc 371
What is the purpose of the MC 371 form?
The MC 371 form is designed for use in the state of California, primarily to facilitate the addition of family members who are requesting Medi-Cal benefits. This includes capturing detailed information about each family member, such as personal identification, citizenship status, health details, and financial information to evaluate eligibility for Medi-Cal.
Who should fill out the MC 371 form?
The form should be filled out by an applicant or caretaker who is applying for Medi-Cal benefits on behalf of themselves and/or additional family members. It's important that this individual provides accurate and comprehensive information about each family member seeking coverage.
What information do I need to provide on the MC 371 form?
Information required includes the names, social security numbers, birth details, citizenship status, and medical and financial information of all family members for whom Medi-Cal coverage is being requested. Details about any disabilities, employment status of parents, current health or dental insurance coverage, and any previous military service must also be provided.
Is U.S. citizenship required for Medi-Cal eligibility as indicated on the MC 371?
No, U.S. citizenship is not a requirement for all applicants. The form asks for citizenship status to determine eligibility under various criteria but also requests information regarding residency for those who are not U.S. citizens or nationals. Therefore, non-citizens also have opportunities for coverage but must provide additional details such as their date of arrival in the U.S.
Can I apply for Medi-Cal coverage retroactively using the MC 371 form?
Yes, there is a section on the form where applicants can request Medi-Cal to cover medical expenses for the three months prior to the application, if eligible. This requires the listing of the names for whom retroactive coverage is sought, along with the specific months of coverage needed.
What does the section regarding sharing information with Healthy Families or similar programs mean?
This section indicates that the Medi-Cal program may share your child’s application information with the Healthy Families program or similar county programs if your child no longer qualifies for free Medi-Cal or does not qualify for full-scope Medi-Cal. Checking the box in this section means you opt out and do not consent to share this information.
How is income and expenses information used in the MC 371 form?
The income and expenses section is crucial for determining your family’s financial eligibility for Medi-Cal. It factors in all sources of income and monthly expenses, including child or dependent care, court-ordered child support, and spousal support. This helps assess whether the household meets the financial criteria for Medi-Cal benefits.
What should I do if a family member has a disability?
If a family member has a physical, mental, emotional, or developmental disability, you should indicate this on the form by checking the appropriate box and providing the date the disability began. This information is important for assessing eligibility and the type of benefits the family member may receive.
How do I submit the MC 371 form once completed?
After ensuring all information on the MC 371 form is accurate and complete, you should follow the submission instructions provided by the Department of Health Care Services or the local agency handling Medi-Cal applications. This might include mailing the form to a specific address or submitting it in person at a local office.
Common mistakes
Filling out the MC 371 form, which is vital for obtaining Medi-Cal benefits, requires careful attention to detail. Unfortunately, several common mistakes can lead to unnecessary delays or even denial of benefits. Here are eight typical errors to avoid:
Not fully completing the form. Every question is there for a reason, and leaving sections blank can lead to processing delays. It's crucial to provide all requested information to the best of your knowledge.
Missing signatures and dates. The form requires a signature and a date at the end to certify that the information provided is accurate and complete. Forgetting to sign or date the form can render it invalid.
Incorrectly reporting family income. This section requires accurate reporting of all sources of income for every family member listed in the application. Overlooking or inaccurately reporting income can affect eligibility.
Forgetting to list all family members needing coverage. Ensure that every family member who requires Medi-Cal coverage is listed on the form, including infants or newly adopted children.
Providing incorrect Social Security numbers. The Social Security number is a critical piece of information used to verify identity and eligibility. Any errors in these numbers can lead to significant delays.
Failure to indicate current health or dental insurance. If anyone in the household has existing coverage, it must be disclosed. This information is essential for determining how Medi-Cal can coordinate benefits.
Overlooking the retroactive coverage section. If you wish to have medical expenses covered for the three months prior to application, this section must be completed. Missing out on retroactive coverage can mean missing out on valuable benefits.
Not checking the boxes for information sharing. These boxes are important if you do not want your child’s application information shared with other health programs. Neglecting to check these can lead to your information being shared without your explicit consent.
While the MC 371 form might seem straightforward, these common mistakes can complicate the process. Ensuring all information is complete, accurate, and thoroughly reviewed before submission will help in the smooth processing of your Medi-Cal application.
Documents used along the form
When applying for Medi-Cal in California using the MC 371 form, which assists in adding additional family members requesting Medi-Cal benefits, it's often necessary to submit more than just this form to ensure a smooth and comprehensive application process. Accompanying documents can provide vital additional information, verify claims made in the application, and help expedite the approval process. Understanding these accompanying documents is crucial for anyone navigating the intricacies of Medi-Cal eligibility and application.
- DHCS 6155 - Health Insurance Information: This form is crucial for those who are currently covered under another health insurance policy. It gathers information about any existing health or dental insurance coverage for any family member included in the Medi-Cal application. Submitting this alongside the MC 371 form ensures that the Department of Health Care Services is aware of all potential sources of coverage, which can affect Medi-Cal eligibility and benefits coordination.
- DHCS 6268 - Perinatal Coverage: For pregnant individuals seeking Medi-Cal services, this form is essential. It specifically addresses the need for perinatal service coverage, providing detailed information about the pregnancy and expected healthcare needs. This form supports the MC 371 form's sections on pregnancy, helping ensure comprehensive coverage from prenatal to postpartum care.
- MC 210 A - Statement of Facts: This comprehensive form provides a full picture of an applicant's financial, residential, and familial situation. It's a critical document for initial Medi-Cal applications and updates, serving to establish or confirm eligibility for the program. When adding new family members through the MC 371 form, the MC 210 A helps verify the household's current situation and any changes affecting eligibility.
- CW 5 - Child Welfare Services: This form is particularly relevant for families involved with the child welfare system. It's used to communicate between the Department of Health Care Services and Child Welfare Services, ensuring that children in foster care or involved with welfare services have accurate Medi-Cal coverage. Submitting this form with the MC 371 can highlight any special considerations or expedite processing for children with active child welfare cases.
Together, these forms create a comprehensive application package for Medi-Cal, streamlining the process of adding family members and adjusting coverage as needed. Applicants are encouraged to gather and prepare these documents with care, ensuring that all information provided is accurate and current. A complete and well-prepared set of documents not only facilitates a smoother application process but can also lead to a quicker decision on Medi-Cal benefits, ensuring timely access to necessary health care services.
Similar forms
MC 210 A - Application for Medi-Cal: This form is used to apply for Medi-Cal benefits and includes similar sections such as personal information, household income, expenses, and an agreement to share information with other health programs. It closely aligns with the MC 371 form in terms of gathering applicant information for Medi-Cal eligibility.
DHCS 6155 - Health Insurance Information: This form collects information about any existing health or dental insurance coverage an applicant or their family members may have. It is similar to sections of the MC 371 form where applicants are asked about current health/dental insurance or Medicare coverage.
DHCS 6268 - Third Party Liability Notification: This form is utilized when an applicant has a lawsuit related to an accident or injury, which could affect their Medi-Cal benefits. It mirrors the MC 371 in terms of querying about lawsuits due to accident or injury and their potential impact on Medi-Cal eligibility.
CW 2.1 - Questionnaire for California’s Public Health Insurance Programs: This form screens for eligibility across different health programs, closely resembling the inclusive approach of the MC 371 form in assessing the needs of additional family members requesting Medi-Cal coverage.
CW 5 - Military Service Questionnaire: This specific document asks about any U.S. military service among family members, which is also a queried aspect in the MC 371 form. It aids in determining eligibility for certain benefits that military families might receive.
MC 321 HFP-AP - Application for the Healthy Families Program: Previously used for applying to the Healthy Families Program, this form collected detailed family income and health information, akin to the MC 371 form’s objective of establishing eligibility for state health services.
MC 210S-C - Statement of Facts for Child Health and Disability Prevention (CHDP) Program: This form was designed to collect information about children’s health and disability status for the CHDP program, in a manner similar to how the MC 371 requests detailed information about children and other family members for Medi-Cal eligibility.
Dos and Don'ts
When filling out the MC 371 form for Additional Family Members Requesting Medi-Cal, attention to detail is crucial for an accurate and prompt processing of your application. Below are some essential dos and don'ts to guide you through the process:
Dos:
- Provide complete and accurate information for all fields relevant to your family's situation. This includes names, birth dates, social security numbers, and Medi-Cal Requested sections.
- Check the appropriate boxes for questions such as U.S. Citizen or National, marital status, and whether the person has a physical, mental, emotional, or developmental disability.
- If applicable, include the Benefits Identification Card number for any family member previously or currently enrolled in Medi-Cal.
- Fill out the section regarding any health or dental insurance coverage accurately, including the OHC Code if known.
- For the Retroactive Coverage section, if you wish to have Medi-Cal cover past medical expenses, ensure to list the names and months correctly.
- Sign and date the form to certify that the information provided is true and complete.
Don'ts:
- Do not leave any required fields blank. If a question does not apply, mark it as "N/A" (not applicable) instead of skipping it.
- Avoid guessing on important details like Social Security numbers or dates; inaccuracies can delay processing or affect eligibility.
- Do not overlook the sections about past military service and wishes about sharing information with the Healthy Families Program. Your choices here are important.
- Refrain from providing partial information about income and expenses. The Family Income and Expenses sections are critical for determining eligibility and benefits level.
- Do not forget to indicate if any family member has had an accident or injury that led to a lawsuit. This information is necessary for comprehensive coverage considerations.
- Do not submit the form without reviewing it for completeness and accuracy to minimize the chances of a delayed or denied application.
Filling out the MC 371 form carefully and truthfully is the first step towards securing Medi-Cal benefits for additional family members. By following these guidelines, applicants can ensure that their requests are processed efficiently and effectively.
Misconceptions
Misconceptions about the MC 371 form, a document necessary for adding additional family members to a Medi-Cal application in California, can create confusion. It's essential to clear up these misunderstandings to streamline the application process. Here are nine common misconceptions and their explanations:
- It's only for current Medi-Cal recipients. This is incorrect. The MC 371 form is designed for anyone requesting to add family members to their Medi-Cal application, regardless of their current enrollment status in Medi-Cal.
- The form is too complex to fill out without professional help. While it's detailed, the MC 371 form is designed to be filled out by applicants. It provides instructions for each section, and additional help is available through the Department of Health Care Services if needed.
- U.S. citizenship is a must for all family members added. This is not the case. The form allows for the inclusion of non-citizens, asking for the date of arrival in the U.S. to determine eligibility for certain newcomers.
- Every family member must have a Social Security Number (SSN) to be added. While having an SSN can expedite the process, the form accommodates situations where a SSN is unavailable or inapplicable, especially for newborns or recent migrants.
- Pregnancy status is irrelevant on this form. Contrarily, pregnancy is a significant factor in Medi-Cal eligibility and benefits determination, with specific sections dedicated to pregnant applicants and their due dates.
- Only biological children can be added with this form. The MC 371 form is inclusive, allowing for the addition of any child under the care of the applicant, including adopted children or stepchildren, as indicated by the relationship section.
- Income and assets of the applicants are not considered. The form demands detailed income information for every family member listed, impacting eligibility and coverage. There's a dedicated section for reporting family income and expenses.
- Applying for retroactive coverage is not an option. Applicants can request Medi-Cal to cover medical expenses for up to three months prior to their application, a fact that's explicitly addressed in the form.
- Medical or dental insurance nullifies the need for Medi-Cal. Having other health insurance does not automatically disqualify someone from receiving Medi-Cal benefits. The form even includes sections to disclose current health or dental insurance coverage.
Understanding the MC 371 form correctly is crucial for accurately requesting Medi-Cal for additional family members, ensuring that eligible individuals receive the benefits they need.
Key takeaways
Here are the key takeaways about filling out and using the MC 371 form for Additional Family Members Requesting Medi-Cal:
- Accuracy is Critical: Ensure all the information provided on the form is accurate; this includes names, dates, and Social Security numbers. Mistakes can delay processing.
- Family Information: The form gathers details about family members requesting Medi-Cal. This includes relationship to the applicant, birth details, and U.S. citizenship status.
- Medical and Disability Information: You must disclose if any additional family member has a physical, mental, emotional, or developmental disability.
- Marital and Parental Status: Marital status, as well as parent-specific information such as living status, employment, and medical support, is required.
- Income and Expenses: Detailed information regarding family income and expenses must be provided. This includes sources of income and monthly expenses like child or disabled dependent care and court-ordered supports.
- Insurance Information: If anyone is covered by health/dental insurance or Medicare, this must be disclosed on the form.
- Retroactive Coverage: Applicants can request Medi-Cal to cover medical expenses for the last three months prior to applying.
- Privacy and Sharing Information: The form outlines conditions under which your information may be shared with other health programs. There's an option to opt-out if you do not want your information shared.
- Signature Required: The form must be signed and dated to certify that the information provided is true and correct.
Completing the MC 371 form meticulously and truthfully ensures a smoother process in requesting Medi-Cal for additional family members. If you have any questions or need clarification, it's advisable to reach out for assistance.
Popular PDF Forms
Metroaccess - The application warns against mailing or faxing submissions; only in-person submissions are accepted.
How Does Gift of Equity Work - A record that benefits homebuyers with family support, specifying the transfer of equity as a gift and legally documenting its no-repayment condition.
Ntsa Form C - It includes sections for both the seller and buyer to fill out their details, vehicle particulars, and transfer details.