Blank Med Rec And Schedule PDF Template
In the intricate journey of patient care, managing and harmonizing medication across various stages of treatment is paramount. The Med Rec and Schedule form emerges as a critical tool in this process, aiming to meticulously document and reconcile medications for individuals undergoing medical care. This comprehensive form captures a broad spectrum of medication-related information, starting with an all-encompassing list of allergies, spanning from latex to iodine, and importantly includes an option to indicate no known drug allergies. It thoughtfully considers the source of this information, whether directly from the patient, a caregiver, or another designated source, while also acknowledging scenarios where obtaining this data might be challenged by the patient's condition or knowledge. Beyond the immediate identification of potential allergens, the form delves into the specifics of each medication - from prescription drugs to over-the-counter solutions, herbals, and even supplements like vitamins and eye drops - detailing the dosage, route of administration for non-oral drugs, frequency of intake, and critical decisions on whether to start, continue, or stop a medication during the visit. It further facilitates patient engagement and continuity of care by requiring signatures from both the patient (or an authorized representative) and the clinician, thereby underscoring the mutual understanding of the medication plan and ensuring that this vital information cascades effectively to subsequent care providers. The inclusion of a segment for subsequent patient visits underscores the form's role in ongoing care, emphasizing the importance of up-to-date and accurate medication information. Therefore, the Med Rec and Schedule form stands as a cornerstone in the seamless transition of care, fostering clear communication and ensuring the safety and efficacy of medication management across the healthcare continuum.
Preview - Med Rec And Schedule Form
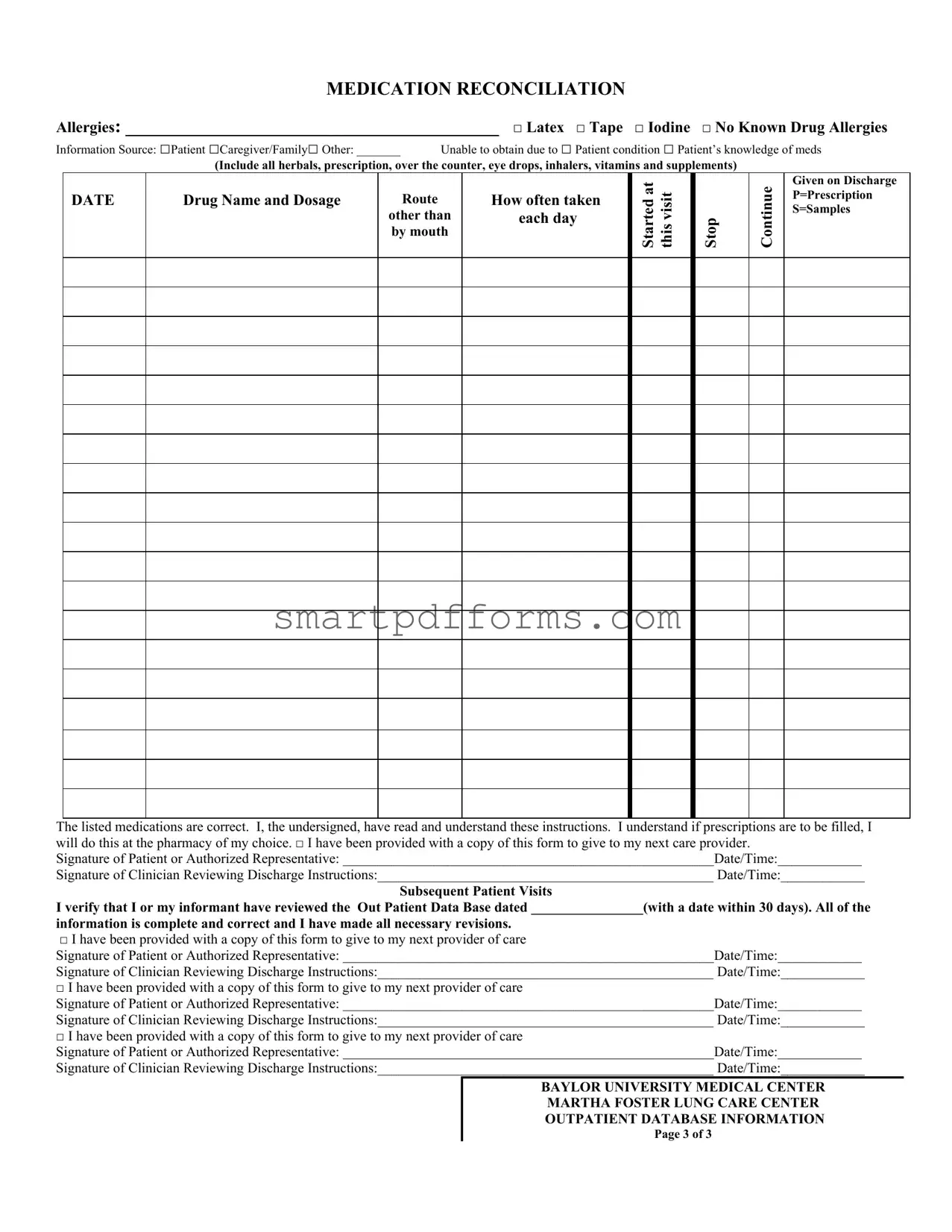
MEDICATION RECONCILIATION
Allergies: ________________________________________ □ Latex □ Tape □ Iodine □ No Known Drug Allergies
Information Source: □Patient □Caregiver/Family□ Other: _______ |
Unable to obtain due to □ Patient condition □ Patient’s knowledge of meds |
(Include all herbals, prescription, over the counter, eye drops, inhalers, vitamins and supplements)
DATE
Drug Name and Dosage
Route
other than by mouth
How often taken each day
Started at this visit
Stop
Continue
Given on Discharge P=Prescription S=Samples
The listed medications are correct. I, the undersigned, have read and understand these instructions. I understand if prescriptions are to be filled, I will do this at the pharmacy of my choice. □ I have been provided with a copy of this form to give to my next care provider.
Signature of Patient or Authorized Representative: _____________________________________________________Date/Time:____________
Signature of Clinician Reviewing Discharge Instructions:________________________________________________ Date/Time:____________
Subsequent Patient Visits
I verify that I or my informant have reviewed the Out Patient Data Base dated ________________(with a date within 30 days). All of the
information is complete and correct and I have made all necessary revisions.
□I have been provided with a copy of this form to give to my next provider of care
Signature of Patient or Authorized Representative: _____________________________________________________Date/Time:____________
Signature of Clinician Reviewing Discharge Instructions:________________________________________________ Date/Time:____________
□I have been provided with a copy of this form to give to my next provider of care
Signature of Patient or Authorized Representative: _____________________________________________________Date/Time:____________
Signature of Clinician Reviewing Discharge Instructions:________________________________________________ Date/Time:____________
□I have been provided with a copy of this form to give to my next provider of care
Signature of Patient or Authorized Representative: _____________________________________________________Date/Time:____________
Signature of Clinician Reviewing Discharge Instructions:________________________________________________ Date/Time:____________
BAYLOR UNIVERSITY MEDICAL CENTER
MARTHA FOSTER LUNG CARE CENTER
OUTPATIENT DATABASE INFORMATION
Page 3 of 3
Form Data
| Fact Name | Description |
|---|---|
| Form Purpose | The form is designed for medication reconciliation to manage and record a patient's medication information, including allergies and how regularly each medication is taken. |
| Allergy Information | Patients can list their allergies, specifically noting if they are allergic to latex, tape, iodine, or have no known drug allergies. |
| Information Source | Information can be provided by the patient, caregiver/family, or another specified source, with options to note if the information couldn't be obtained and why. |
| Medication Details | For each medication, details such as drug name and dosage, route (if not oral), frequency, and whether it was started at the visit, should continue, or is given on discharge are recorded. It also distinguishes between prescriptions and samples. |
| Confirmation of Medication List Accuracy | The form includes a statement for the patient or authorized representative to sign, confirming they have reviewed the medication list for accuracy and understand the instructions provided. |
| Copy Provision for Next Care Provider | It specifies that a copy of the completed form should be provided to the patient to give to their next care provider, ensuring continuity of care. |
| Governing Law(s) | While specific governing laws might vary by location, the form adheres to healthcare documentation and patient care standards, likely influenced by HIPAA regulations for patient information confidentiality and accuracy. |
Instructions on Utilizing Med Rec And Schedule
Filling out the Med Rec And Schedule form is an important step in ensuring accurate medication management. This form helps to reconcile medications during healthcare visits, ensuring that there's a clear record of allergies, medications currently being taken, and changes in medication regimes. It serves as a crucial tool for communication between patients, caregivers, and healthcare providers. The ultimate objective is to enhance patient care by reducing medication errors and improving outcomes. To successfully complete this form, follow the steps outlined below.
- Start by listing any Allergies the patient has in the provided space, including if they are allergic to latex, tape, iodine, or if they have no known drug allergies.
- Indicate the Information Source by checking the appropriate box: Patient, Caregiver/Family, or Other (specify if selected). Also, note reasons if unable to obtain medication information, such as the patient's condition or lack of knowledge about their medications.
- Under the section marked Medication Reconciliation, start filling in the details for each medication:
- Dates when the medication was started or if it started at the current visit.
- The name of each drug and its dosage.
- How the medication is taken if not by mouth (e.g., inhalation, injection).
- How often the medication is taken each day.
- Tick the appropriate box to indicate if the medication is to be stopped, continued, or if given on discharge. Also, note whether the medication is a prescription (P) or sample (S).
- Confirm that the medications listed are correct, and acknowledge understanding by having the patient or authorized representative sign and date at the bottom of the form.
- Make sure the clinician reviewing the discharge instructions also signs and dates the form.
- For subsequent patient visits, verify information by reviewing the Out Patient Data Base. Ensure that the date within 30 days is entered, and consider any necessary revisions. The patient or authorized representative and the clinician should again sign and date the form.
After completing the form, it is essential to provide a copy to the patient or authorized representative to share with their next care provider. This fosters continuity of care and ensures all healthcare providers are informed of the patient's current medication regimen and allergies, contributing to safer and more effective care.
Obtain Answers on Med Rec And Schedule
What is the purpose of the Med Rec And Schedule form?
The Med Rec And Schedule form serves to ensure that there is a complete and accurate record of a patient’s medication history, including any allergies, the sources of this information, and specific medication instructions. This form is crucial in coordinating care among different healthcare providers and avoiding medication errors, especially during transitions like hospital discharge.
Who can provide the information needed for the Med Rec And Schedule form?
Information for the Med Rec And Schedule form can be provided by the patient, a caregiver or family member, or another source if specified. However, it's important to note that sometimes information cannot be obtained due to the patient’s condition or their knowledge of their medications.
What kinds of medications should be listed on the form?
All types of medications need to be listed on the form, including prescription medications, over-the-counter drugs, herbal supplements, vitamins, eye drops, and inhalers. This comprehensive recording ensures that all aspects of a patient’s medication regimen are considered and managed properly.
What does it mean when medications are marked to 'Stop' or 'Continue'?
On the Med Rec And Schedule form, medications marked as 'Stop' are those that the healthcare provider has decided should not be part of the patient's medication regimen moving forward. Those marked as 'Continue' are to be kept in the patient's medication schedule. This distinction helps in managing and updating the patient’s medication regimen accurately.
What should be done if prescriptions are to be filled?
If prescriptions are to be filled following the instructions on the Med Rec And Schedule form, patients are responsible for having them filled at the pharmacy of their choice. This notation on the form reminds patients that they must take action to ensure they receive their prescribed medications.
How are subsequent patient visits documented on the form?
For subsequent patient visits, the form includes a section where the patient or their representative verifies that they have reviewed their Out Patient Data Base with a date within 30 days. Any necessary revisions to the medication list must be made during these reviews to ensure the information remains complete and correct. Copies of this updated form should be given to the next provider of care, as indicated by checking the appropriate box.
Common mistakes
When completing the Med Rec And Schedule form, several common errors can affect the clarity and accuracy of your medical records. Recognizing and avoiding these mistakes is essential for ensuring your healthcare team understands your needs and conditions accurately.
Not listing all allergies, including less common ones like latex, iodine, or tape, can lead to adverse reactions during treatment.
Forgetting to specify the information source, whether it's the patient, caregiver, or another source, can lead to confusion about the reliability of the provided data.
Omitting over-the-counter medications, vitamins, and supplements from the list can result in dangerous drug interactions.
Leaving out the dosage details for each medication risks incorrect administration, potentially leading to underdosing or overdosing.
Not indicating the route of administration for medications taken in ways other than by mouth (e.g., inhalers, injections) can lead to misunderstandings in how to correctly take the medication.
Skipping the frequency details—how often each medication is taken—prevents a clear schedule from being established, which is crucial for effective treatment and avoidance of conflicts between medications.
Failing to mark whether a medication was started at this visit, will be continued, or given only on discharge leaves out critical information for ongoing care management.
Not verifying the listed medications by leaving the signature section blank undermines the form’s validity and may lead to administrative delays or medical errors.
Forgetting to provide a date puts the form's information at risk of being considered outdated, affecting future healthcare decisions.
Not keeping a copy of the form for personal records or to share with the next care provider can lead to gaps in the continuity of care.
Mitigating these mistakes ensures the Med Rec And Schedule form accurately reflects your current medications and health conditions, safeguarding your well-being through precise and timely care coordination.
Documents used along the form
When managing healthcare, particularly relating to medication management and patient care transitions, several forms and documents usually accompany the Medication Reconciliation and Schedule (Med Rec And Schedule) form. These documents help ensure a seamless and coordinated care process, enhancing both the safety and the efficacy of medication administration.
- Patient Consent Form: This document is vital for authorizing healthcare providers to share and discuss the patient's medical information with other professionals involved in their care. It ensures the patient's privacy rights are respected while enabling comprehensive care coordination.
- Healthcare Proxy or Medical Power of Attorney (POA) Form: This legal document designates another person to make healthcare decisions on behalf of the patient if they become unable to do so. It’s crucial for situations where patients are incapacitated or otherwise unable to articulate their healthcare preferences.
- Advanced Directive or Living Will: This document outlines the types of medical treatments and life-sustaining measures a patient wishes or does not wish to receive if they're unable to communicate their decisions due to illness or incapacity. It guides healthcare providers in honoring the patient's healthcare preferences.
- Discharge Summary: A comprehensive summary that provides details about the patient's hospital stay, including the reason for admission, the care received, medications prescribed at discharge, and follow-up care instructions. This document is critical for the next care provider to understand the patient's recent medical history.
- Emergency Contact Information: A form that lists the patient's emergency contacts, including names, relationships to the patient, and contact information. This document is essential for healthcare providers to quickly communicate with relatives or caregivers in case of an emergency.
- Insurance Information Form: Contains details about the patient’s health insurance coverage, policy numbers, and contact information for the insurance company. This document is necessary for processing claims and ensuring that healthcare services are appropriately billed.
Together with the Med Rec And Schedule form, these documents create a comprehensive patient profile that enhances caregiver communication, supports decision-making, and ensures that patient care is aligned with individual health goals and legal preferences. Having a complete set of these forms can significantly impact the quality of care provided, ensuring that it's both effective and respects the patient's wishes.
Similar forms
Patient History Forms: Similar to the Med Rec And Schedule form, Patient History forms systematically collect a patient's personal health history, allergies, and previous treatments. Both require information from the patient or a caregiver and serve as a critical tool for informing healthcare providers about a patient's past to make informed decisions.
Prescription Order Forms: These forms, used by doctors to prescribe medications, share similarities with the medication aspect of the Med Rec And Schedule form. Both document the drug name, dosage, and instructions for use. However, the Med Rec And Schedule form also includes a reconciliation process to ensure current medication lists are accurate and comprehensive.
Consent Forms for Treatment: Consent forms, which must be signed before any medical procedure or treatment, are akin to the Med Rec And Schedule form in that both require a patient's or authorized representative’s signature to proceed. Each plays a vital role in confirming the patient's understanding and agreement to the proposed medical interventions or medication plan.
Discharge Summaries: Discharge summaries provide a comprehensive account of a patient's hospital stay, including medication prescribed at discharge, similar to sections of the Med Rec And Schedule form that list medications to continue or start post-visit. Both are vital for transitioning care from a hospital to home or another care setting, ensuring continuity and safety in medication management.
Medical Referral Forms: Like the Med Rec And Schedule form, Medical Referral Forms are used to transition a patient's care between healthcare providers. Both types of documents ensure that the receiving party has accurate and up-to-date information on the patient’s medical condition, including medication details, thereby facilitating a seamless continuation of care.
Dos and Don'ts
When filling out the Med Rec And Schedule form, it's important to approach the task with attention to detail and clarity, ensuring the information provided is accurate and comprehensive. Below are essential do's and don'ts to consider:
Do:
- Ensure that all medication information, including over-the-counter drugs, vitamins, and supplements, is listed accurately. This includes the drug name, dosage, route of administration (if other than by mouth), and frequency of intake.
- Clearly indicate any allergies, checking the appropriate boxes for common allergens like latex, tape, and iodine, and specifying any known drug allergies.
- Specify the information source at the beginning of the form, whether it is the patient, caregiver/family, or another source, to provide context on the reliability and origin of the provided data.
- Sign and date the form as required in both the initial medication reconciliation section and subsequent patient visit sections to verify the accuracy of the listed information and compliance with discharge instructions.
Don't:
- Overlook the importance of listing all medications, including seemingly insignificant ones like herbal supplements or over-the-counter treatments, as they can have significant interactions with prescribed medications.
- Forget to check the boxes corresponding to the patient’s allergy information; an unchecked box could lead to incorrect assumptions about a patient’s sensitivity or allergic conditions.
- Leave sections incomplete, such as not specifying the ‘Other’ information source or failing to indicate whether the patient condition allows for accurate medication information retrieval.
- Fail to provide a copy of the completed form to the patient or authorized representative if indicated, as this could disrupt continuity of care and communication with subsequent healthcare providers.
Misconceptions
Understanding the Medical Reconciliation and Schedule (Med Rec And Schedule) form is pivotal in ensuring that patients receive comprehensive and safe healthcare. However, several misconceptions exist regarding its use and purpose. Clarifying these misunderstandings is essential for both healthcare professionals and patients.
- Misconception 1: The Med Rec And Schedule form is only used for prescription medications.
This is incorrect. The form also includes over-the-counter medications, herbals, vitamins, supplements, eye drops, and inhalers, ensuring a comprehensive overview of a patient's medication regimen.
- Misconception 2: Information on allergies is not crucial if the patient has no known drug allergies.
Even if a patient has no known drug allergies, documenting this information on the form is vital, as it confirms that the topic has been addressed and clarifies the patient's allergy status for future healthcare providers.
- Misconception 3: The Med Rec And Schedule form is solely the responsibility of the healthcare provider.
While healthcare providers play a critical role in completing and reviewing the form, patients and their caregivers are also crucial sources of information and must actively participate in the reconciliation process to ensure accuracy.
- Misconception 4: The form is static and only needs to be filled out once.
The form should be updated regularly to reflect any changes in medication regime, including new prescriptions, changes in dosage, or medications that have been discontinued. This ensures ongoing accuracy and safety in the patient's care.
- Misconception 5: If you're discharged from care, you don't need to provide the form to your next care provider.
On the contrary, providing a copy of the form to the next care provider is crucial for maintaining continuity of care and avoiding potential medication errors.
- Misconception 6: The signatures on the form are just a formality.
Signatures of both the patient (or authorized representative) and the clinician reviewing the discharge instructions serve as a verification that the medication information has been reviewed, understood, and agreed upon by both parties, ensuring a mutual understanding of the treatment plan.
- Misconception 7: The form is unnecessary if the patient uses a single pharmacy.
Even if medications are filled at a single pharmacy, the Med Rec And Schedule form is still essential. It provides a consolidated record of all medications and supplements being taken, which can aid in identifying potential interactions and ensuring proper medication management across all healthcare providers.
By understanding and correcting these misconceptions, patients and healthcare professionals can work together more effectively to ensure safe and accurate medication management. This collaborative effort is key to enhancing patient safety and care outcomes.
Key takeaways
Understanding the Med Rec And Schedule form is crucial for ensuring that the information it contains is accurate and complete. Here are four key takeaways to guide patients and their families when dealing with this important document:
- Comprehensive Medication Listing: It's vital to list all forms of medications, including prescriptions, over-the-counter drugs, herbals, eye drops, inhalers, vitamins, and supplements. This thoroughness helps prevent potential drug interactions and ensures the patient's safety.
- Source of Information: Accurately indicating whether the medication information was provided by the patient, a caregiver or family member, or another source is essential for validating the credibility of the information recorded. It is also important to note if there were any limitations in obtaining this information, such as the patient's condition or knowledge.
- Medication Reconciliation and Continuity of Care: The form includes sections for documenting allergies, tracking whether medications were started, continued, or stopped during the visit, and if they were given on discharge. This process, known as medication reconciliation, is crucial for ensuring continuity of care, especially when transferring a patient to another healthcare provider or setting.
- Verification and Acknowledgement: The form requires signatures from both the patient (or an authorized representative) and the clinician reviewing discharge instructions. This step not only acknowledges that the patient has received and understands the instructions but also confirms that they have been provided with a copy of the form to share with their next care provider. This is a critical step for empowering patients and facilitating communication between different care providers.
The Med Rec And Schedule form serves as a vital tool in managing a patient's medication regimen accurately and safely. By thoroughly completing and understanding each section, patients and healthcare providers can work together effectively to ensure the best possible outcomes.
Popular PDF Forms
Sds Category Canada - By fulfilling each checklist item, applicants can confidently submit their Study Permit application, minimizing potential issues.
Esther Beth Moore - Explore the nuanced teachings of the Book of Esther with Beth Moore, highlighting the transformative journey of faith and womanhood.