Blank Nc Application Medicaid PDF Template
The North Carolina Application for Medicaid, as outlined by the Department of Health and Human Services, serves as a vital gateway to medical assistance for various groups including the Aged, Blind, and Disabled, alongside those seeking Family Planning services. This comprehensive form separates the application process for children and families, ensuring a targeted approach to Medicaid eligibility and access. By requiring applicants to list all family members seeking medical assistance, alongside other household members, the form adopts a household-centric view, albeit with specific instructions not to share sensitive information such as social security numbers, citizenship, or immigration status for non-applicants. This meticulous attention to detail facilitates a thorough understanding of the applicant’s domestic and financial situation without compromising the privacy of individuals not seeking coverage. The process is clearly delineated with options for submitting the application directly to the local Department of Social Services, reflecting a structured pathway towards obtaining crucial medical coverage. Moreover, the document elaborates on eligibility criteria, including special considerations for those 65 and older, blind, physically or mentally disabled, or in need of long-term care or family planning services, thus painting a broad stroke of inclusivity. It also provides a pathway for applicants unsure of their qualifications to seek direct counsel from Medicaid caseworkers, reinforcing the accessible nature of this assistance program. The form further outlines the rights and responsibilities of applicants, such as the application process, necessary documentation, and the importance of honest communication regarding any changes that may affect eligibility. Information on how Medicaid can retroactively cover medical bills, alongside the emphasis on keeping personal information confidential, underscores the program's commitment to both immediate and long-term support for individuals and families navigating financial and medical vulnerabilities. With clear instructions, it demystifies the often complex terrain of applying for Medicaid, reflecting a well-thought-out process designed to facilitate access to necessary health services for North Carolina’s residents.
Preview - Nc Application Medicaid Form
Application for Medicaid
N.C. Department of Health and Human Services
This application is intended for medical assistance for the Aged, Blind and Disabled or those who want Family Planning services. A different application form is available for children and families who need Medicaid. Children under age 21 and adults with children in their care may be eligible for Medicaid without being blind, disabled or age 65 and older. You will need to list all family members who are applying for medical assistance. In addition, to ensure the applicants receive all possible assistance, list other persons in the home. Do not give us social security numbers, citizenship, or immigration status for these other persons.
If you have questions about Medicaid programs for which you may be eligible, please contact the Department of Social Services in the county where you live and ask to speak with a Medicaid caseworker.
Just mail or drop off the completed application at the department of social services in the county where you live. You can find address and phone number in your phone book under “County Government.”
If you want to apply for Work First Family Assistance, Food Stamps, or Special Assistance (to pay for care in an Adult Care Home,) you must see a worker and complete an application at the Department of Social Services.
IMPORTANT NOTICE
IF YOU CHOOSE TO PICK UP THIS APPLICATION AT THE DSS OFFICE:
You or your representative have the right to make an application and have a
If you cannot stay to see a worker to apply for Medicaid, but you want a
If you do not want a
•The date of your application is the date the Department of Social Services gets your complete application.
•Medicaid coverage can be requested for any medical bills incurred up to three months prior to the month of application.
•The date your Medicaid is started is based on the date of your application. If you wait until next month to return your complete application, Medicaid may not be able to help pay for medical services you received in earlier months.
•If you are unable or need help to complete the application or to obtain requested information, contact the department of social services and speak with a Medicaid caseworker.
•You will receive a telephone
Page 1 of 16 |
|
Rev. 08/12 |
|
What is Medicaid?
Medicaid is a health insurance program for those with income below amounts set by the federal and state government or with large unmet medical needs.
Who can get Medicaid?
♦Individuals or couples who are elderly (age 65 or older)
♦Individuals who are visually impaired (blind)
♦Individuals who need help in their home to care for themselves (CAP)
♦Individuals who need help caring for themselves (nursing home or
♦Individuals or couples who are physically or mentally disabled
♦Individuals or couples who would like to receive family planning services
♦Children under age 21 and adults with children in their care
♦Pregnant Women
See page 3 for what the state of North Carolina considers to be disabled and a description of the CAP program.
What will Medicaid pay for?
Medicaid can help pay for certain medical expenses such as:
♦Doctor Bills
♦Hospital Bills
♦Prescriptions (Excluding prescriptions for Medicare beneficiaries effective 01/01/06)
♦Vision Care
♦Dental Care
♦Medicare Premiums
♦Nursing Home Care (LTC)
♦Personal Care Services (PCS), Medical Equipment, and Other Home Health Services
♦In home care under the Community Alternatives Program (CAP)
♦Mental Health Care
♦Most medically necessary services for children under age 21
Who can answer my questions about Medicaid?
You can contact your local county department of social services, call the Medicaid Eligibility Unit through the DHHS Customer Service Center, at
What is the Community Alternatives Program (CAP)?
The Community Alternatives Program (CAP) allows some Medicaid recipients who require institutional care (placement in a hospital, nursing home, or
How do I know if I am disabled?
An individual may be eligible for Medicaid if he is disabled according to the Social Security definition of disability. A child must meet Social Security’s childhood disability rules. If you are disabled you:
♦Are unable to work for at least one year due to your medical problem, or
♦Have a medical problem that may result in death.
If you receive a Social Security (RSDI) or Supplemental Security Income (SSI) check because you are disabled you are automatically considered to meet the disability requirement for Adult Medicaid. Other individuals who apply for Medicaid and are over age 21, under age 65, and do not have children in their care, must be found to be disabled. This requirement does not apply to Family Planning Services only.
Page 2 of 16 |
|
Rev. 08/12 |
|
How do I apply for assistance?
You will need to:
♦Answer the questions in sections 1 through 15 in a legible manner.
♦Sign the application.
♦Bring or mail this application to your county department of social services (DSS) in the county where you live. If you need help locating your county DSS office, please call the DSS office, or the DHHS Customer Service at
♦Provide the needed items to complete your application. If you do not have all of the needed information and need help getting the information, return the application and ask your Medicaid worker at DSS for assistance.
Once your application is received by your county department of social services, a case worker will call you to discuss your application in detail.
What if I need help completing this application?
Visit or call your county DSS. If you do not know where your county DSS is, call the DHHS Customer Service
What do I do after I fill out this application?
I fill out the application?
♦Tear off pages 1 through 8 and keep them for your records.
♦Be sure that you answer all questions in sections 1 through 15.
♦Attach any documentation or verifications needed to process your application if you have them.
♦Remember to sign and date page 18 because your application can not be processed without your signature.
♦Bring or mail the Medicaid application to your county DSS.
How long will it take to process my application?
Once your application is received, we will begin processing it.
♦If you are 65 or older, a child, or caretaker of a child, it can take up to 45 days to process your application.
♦If you are under age 65 and have no child in your care, it can take up to 90 days to process your application.
♦If we need additional information, we will contact you by telephone or mail. The sooner we get the information, the sooner we can let you know if you can get Medicaid.
What are my rights?
♦To apply for Medicaid, and, if found ineligible, you may reapply at any time.
♦To apply for other assistance like Food Stamps or Work First Family Assistance.
♦To have any person help you with this application or participate in the interview for determination of eligibility.
♦To be protected against discrimination on the grounds of race, creed, or national origin by Title VI of the Civil Rights Act of 1964.
♦To have any information given to the agency kept in confidence.
♦To be given information by Social Services about Medicaid and other available assistance.
♦To get assistance from the department of social services in completing this application or in getting information needed to process the application.
♦To withdraw from the Medicaid program at any time.
♦To receive assistance, if found eligible.
♦To have your eligibility for Medicaid considered under all categories.
Page 3 of 16 |
|
Rev. 08/12 |
|
What are my responsibilities?
♦To provide the county department of social services (DSS), as well as state and federal officials, upon request, the information necessary to determine eligibility.
♦To report to the DSS any change in my situation within 10 calendar days of the change.
♦To report to the DSS if I receive benefits in error.
♦To agree, by signing this form, that all information that I have provided is true and a complete statement of fact according to the best of my knowledge and that I understand it is against the law to willfully withhold information or make false statements. I am subject to prosecution if I do.
♦To understand that any Medicaid ID card I receive is to be used only for the person listed on the ID card. I understand it is against the law to give my ID card to someone whose name is not listed on it and that I may be prosecuted for fraud if I let someone else use my ID card.
♦To understand if any resources are transferred out of the applicant’s name without receiving fair market value for the resources, it could result in a period of ineligibility for
♦To understand any child or spousal support (money) which is paid directly to me must be reported to the county department of social services and will be counted as income when determining eligibility for Medicaid benefits for the person for whom it is received.
♦North Carolina must be named remainder beneficiary for annuities purchased after November 1, 2007. Contact the county DSS for more information.
Medical/ Financial Records
I understand that my medical and financial records must be made available to the agency and the State by any provider from whom I have received medical care services. I hereby agree to the release of those records by those providers when requested by the agency and the State. The privacy of this information is protected by law.
Assignment of Rights
I understand that by accepting medical assistance, I agree to give back to the State any and all money that is received by me or anyone listed on this application from any insurance company for payment of medical and/or hospital bills for which the medical assistance program has or will make payment. I agree to assign the State of North Carolina as the Remainder Beneficiary of any annuities that I may have. In addition, I agree that all medical payments or medical support paid or owed due to a court order for me or anyone listed on this application must be sent to the State to repay past or current medical expenses paid by the State. This includes insurance settlements resulting from an accident. I further agree to notify the county department of social services if I or anyone listed on this application is involved in an accident. I understand that this assignment of rights continues as long as I or anyone listed on this application receive Medicaid and is based on federal regulations.
Social Security Numbers
I understand that I must furnish all social security numbers used by me to determine my eligibility for assistance if I am applying for myself. I understand that if anyone else wants to apply for assistance their social security number must also be furnished. I also understand these social security numbers will be used in matching information with the Social Security Administration (SSA), Internal Revenue Service (IRS), Employment Security Commission (ESC), Department of Transportation (DOT), out of state welfare and ESC agencies, and any other agencies, when applicable. If I do not want these social security numbers used in the matches, I understand that I have the right to request my assistance to be denied, terminated or withdrawn.
Estate Recovery Notice
I understand that Federal and State laws require the Division of Medical Assistance (DMA) to file a claim against the estate of certain individuals to recover the amount paid by the Medicaid program during the time the individual received assistance with certain medical services. Ask your Medicaid case worker for specific information regarding which services are applicable to estate recovery.
Page 4 of 16 |
|
Rev. 08/12 |
|
If You Request A Hearing
If you do not agree with a decision we make about your case, you can request a hearing. You can request this in person, by telephone or in writing. You must ask for this hearing within sixty days of when we tell you in writing of our decision on your application. You have the right to examine your case record and documents used before your hearing.
You can have a household member or someone you ask to represent you, like a friend or relative. You also have the right to have an attorney or other legal representative represent you at the hearing. Free legal aid may be available. Call
Citizenship, Identity and Immigration Status
I understand that the county DSS worker will verify citizenship, identity, and immigration status to determine which Medicaid program the applicant may qualify for. Household members listed on the application, but are not applying for Medicaid, will not be subject to this verification. In order to receive services, the applicant’s identity must be confirmed. In order to receive regular Medicaid, the applicant must be a citizen or have a qualified alien status. If citizenship or immigration status makes the applicant not eligible for regular Medicaid, the applicant can apply for Emergency Medicaid services.
If the county DSS worker is unable to verify citizenship, identity, and/or immigration status, the applicant may need to provide additional documentation. If the alien applicant has no documents to establish qualified alien status, contact a county DSS worker for assistance. If not eligible for regular Medicaid, I understand that persons applying for Emergency Medicaid services only are not required to declare or provide documentation of their immigration status or Social Security Number. These individuals must meet all other Medicaid eligibility requirements, and qualify for one of the Medicaid coverage groups.
Residence
I hereby certify under penalty of perjury that I and all the persons for whom I am making an application are living in North Carolina with the intention of remaining permanently or for an indefinite period, in the state seeking employment, or have a job commitment.
To verify North Carolina residency, provide two different documents from the following list:
♦A valid North Carolina driver license or other identification card issued by the North Carolina Division of Motor Vehicles.
♦A current North Carolina rent, lease, mortgage payment receipt, or current utility bill in the name of the applicant or the applicant’s legal spouse, showing a North Carolina address.
♦A current North Carolina motor vehicle registration in the applicant’s name and showing the applicant’s current North Carolina address.
♦A document verifying that the applicant is employed in North Carolina.
♦One or more documents proving that the applicant’s home in the applicant’s prior state of residence has ended, such as closing of a bank account, termination of employment, or sale of a home.
♦The tax records of the applicant or the applicant’s legal spouse, showing a current North Carolina address.
♦A document showing that the applicant has registered with a public or private employment service in North Carolina.
♦A document showing that the applicant has enrolled his children in a public or private school or a child care facility located in North Carolina.
♦A document showing that the applicant is receiving public assistance (such as Food Stamps) or other services which require proof of residence in North Carolina. Work First and Energy Assistance do not currently require proof of NC residency.
♦Records from a health department or other health care provider located in North Carolina which shows the applicant’s current North Carolina address.
Page 5 of 16 |
|
Rev. 08/12 |
|

♦A written declaration from an individual who has a social, family, or economic relationship with the applicant, and who has personal knowledge of the applicant’s intent to live in North Carolina permanently, for an indefinite period of time, or residing in North Carolina in order to seek employment or with a job commitment.
♦A current North Carolina voter registration card.
♦A document from the U.S. Department of Veteran’s Affairs, U.S. Military or the U.S. Department of Homeland Security, verifying the applicant’s intent to live in North Carolina permanently or for an indefinite period of time, or that the applicant is residing in North Carolina to seek employment or has a job commitment.
♦Official North Carolina school records, signed by school officials, or diplomas issued by North Carolina schools (including secondary schools, colleges, universities, community colleges), verifying the applicant’s intent to live in North Carolina permanently or for an indefinite period of time, or that the applicant is residing in North Carolina to seek employment or has a job commitment.
♦A document issued by the Mexican consular or other foreign consulate verifying the applicant’s intent to live in North Carolina permanently or for an indefinite period of time, or that the applicant is residing in North Carolina to seek employment or has a job commitment.
*If you do not have two of these documents, contact the county DSS for assistance.
MEDICAL TRANSPORTATION ASSISTANCE
NOTICE OF RIGHTS
The following information regarding medical transportation was explained to me. I understand that:
♦If I receive Medicaid or have presumptive eligibility and do not have a way to get to the doctor or to other medical services, social services will help me arrange suitable transportation.
♦I can receive transportation assistance only after I am authorized for Medicaid or found to be presumptively eligible.
♦Medical transportation expenses that I am responsible for paying can be used to meet a deductible, including transportation expenses for anyone who is financially responsible for me.
♦I have the right to ask for help with transportation. I understand that if transportation is provided, it will be to the nearest appropriate medical provider of my choice, by the least expensive method suitable to my individual needs.
♦I, or someone acting on my behalf, may contact DSS by mail, phone, or in person to ask for help with transportation to the doctor or other medical services.
♦Except for emergencies, I must request transportation assistance as far in advance of my appointments as possible. Otherwise, my appointment(s) may have to be rescheduled.
♦I understand that I am not eligible for transportation assistance:
if I am authorized for
while my application is pending (before a decision is made) while I am on a deductible for Medicaid; OR
while I am authorized for NC Health Choice.
•I have the right to a written notice of decision on my request within 10 work days, and I have the right to have a local hearing to appeal the decision if I disagree.
NOTE: You will need 2 first class stamps to mail this application. If you include additional information (pay stubs, bank statements, etc.) with the Medicaid application, additional postage may be needed. It is recommended that you contact the post office to verify the amount of postage needed.
*Tear off pages 1 through 6 and keep them for your records.
Page 6 of 16 |
|
Rev. 08/12 |
|
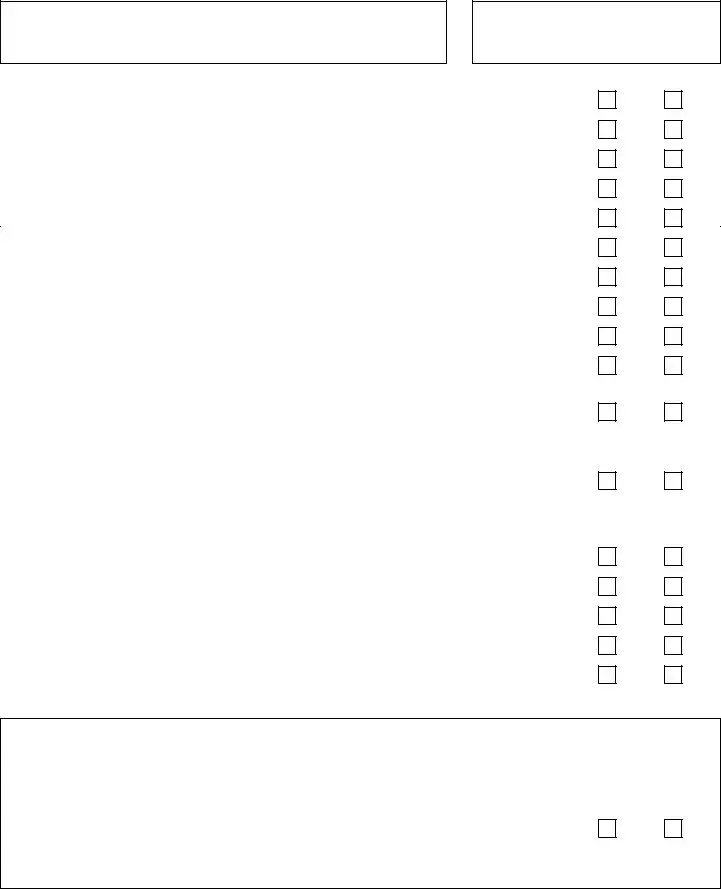
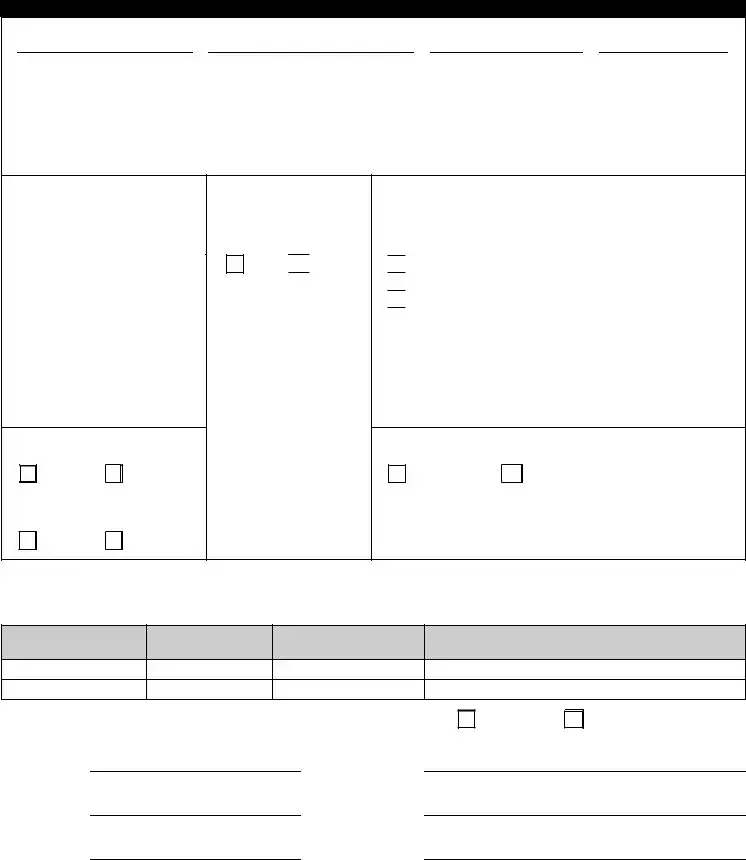
Application for Adult Medicaid
North Carolina Department of Health and Human Services
For Official Use Only
County DSS: ________________________
Date Received:_______________________
Case #: _____________________________
DSS _______ |
Aging _______ |
Mail In________ |
I am applying for Medicaid for myself. |
|
|
|
|
Yes |
No |
|||||
I am applying for Medicaid for my spouse. |
|
|
|
|
Yes |
No |
|||||
I am age 65 or older. |
|
|
|
|
|
|
|
Yes |
No |
||
My spouse is age 65 or older. |
|
|
|
|
|
|
|
Yes |
No |
||
I am blind. |
|
|
|
|
|
|
|
Yes |
No |
||
My spouse is blind. |
|
|
|
|
|
|
|
Yes |
No |
||
I am disabled. |
|
|
|
|
|
|
|
Yes |
No |
||
My spouse is disabled |
|
|
|
|
|
|
|
Yes |
No |
||
My child is disabled. |
|
|
|
|
|
|
|
Yes |
No |
||
I am applying for Medicaid for a child or children in my care. List children below: |
Yes |
No |
|||||||||
|
|
|
|
|
|
|
|
|
Citizen? |
Yes |
No |
Name |
DOB |
Sex |
|
Social Security |
|
|
|||||
|
Number |
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
Citizen? |
Yes |
No |
Name |
DOB |
Sex |
|
Social Security |
|
|
|||||
|
Number |
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|||||
I need help with nursing home care. |
|
|
|
|
Yes |
No |
|||||
My spouse needs help with nursing home care. |
|
|
|
|
Yes |
No |
|||||
I am applying for the Community Alternatives Program (CAP). |
Yes |
No |
|||||||||
My spouse is applying for the Community Alternatives Program (CAP). |
Yes |
No |
|||||||||
My child is applying for the Community Alternatives Program (CAP). |
Yes |
No |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
Medicaid Family Planning Waiver Services
To be eligible for Medicaid Family Planning Waiver services, you must be a woman age 19 through 55 or a man age 19 through 60 and have not had a medical procedure that would prevent you from having a baby or fathering a baby.
Do you wish to apply for the Medicaid Family Planning Waiver? |
|
Yes |
No |
|||
If yes, for whom |
|
|
Social Security # |
|
|
|
Page 7 of 18 |
|
Rev. 08/12 |
|
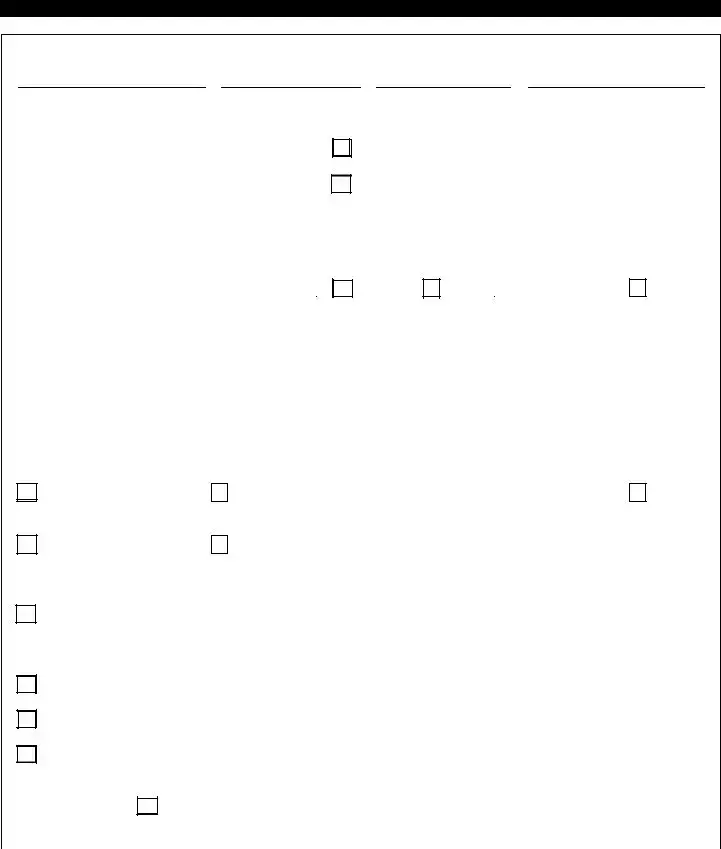
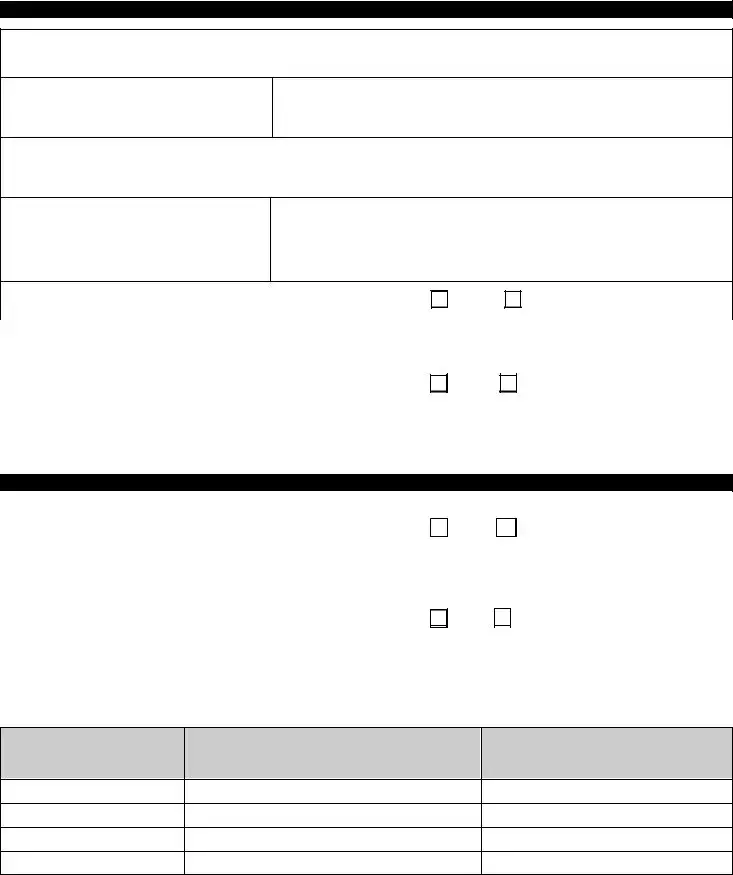
1. Tell us about you.
Applicant’s Name
|
|
|
First |
|
|
|
|
|
|
Middle |
|
|
|
|
|
|
Maiden |
|
|
|
|
Last |
|
|
|
|
|
|||||||||
Social Security Number |
|
|
|
|
|
|
|
|
|
|
Sex |
|
|
Date of Birth |
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Male |
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
/ |
|
|
/ |
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(Not required if you are not applying for Medicaid |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
Female |
|
|
|
Month |
Date |
|
Year |
||||||||||||||||||||||||||
for yourself, you are applying for Medicaid |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
someone else, or you are applying for Emergency |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
Medicaid.) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
Please indicate your race(s) |
|
|
|
|
|
|
|
Hispanic/Latino? |
Do you speak English? |
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
|
No |
|
|
Yes |
|
|
No |
|||||||
Asian= A |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
White or Caucasian = W |
|
|
|
|
|
|
|
If yes, specify by circling |
What language do you prefer to |
|||||||||||||||||||||||||||
Black or African American = B |
|
|
|
|
|
|
|
the code below: |
|
|
speak if not English? |
|
|
|
|
|
||||||||||||||||||||
American Indian or Alaska Native = I |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
Native Hawaiian or |
|
|
|
|
|
|
|
|
|
|
Hispanic Cuban= C |
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||
Other Pacific Islander = P |
|
|
|
|
|
|
|
Hispanic Mexican= M |
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hispanic Puerto Rican= P |
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hispanic Other= H |
|
|
|
|
|
|
|
|
|
|
|
|||||||
Are you a Veteran? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I am a U.S. Citizen. |
|
|
|
|
|
||||||||||||
|
|
|
Yes |
|
|
|
|
|
No |
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
|
No |
||||||||||||
Have you served in the armed forces? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
Yes |
|
|
|
|
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ARE YOU: |
|
|
|
|
|
|
|
|
|
|
If you live with your spouse: |
|
|
|
|
|
|
|
||||||||||||||||||
|
|
|
Married |
|
|
|
|
|
|
|
|
|
|
Spouse’s Name: |
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
Widowed |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
First |
Middle |
Maiden |
Last |
|
|
|
|
|
|||||||||
|
|
|
Single |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Date of Birth: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
Divorced |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Sex: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
Separated (When? |
|
) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Do you live with your spouse? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
Yes |
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
*Complete section 2 on the next page, only if you want to apply for Adult Medicaid for your spouse.
Page 8 of 16 |
|
Rev. 08/12 |
|
2. Tell us about your spouse.
|
|
|
First |
|
|
Middle |
Maiden |
|
Last |
|||||||
Social Security Number |
Sex |
|
Date of Birth |
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
Male |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(Not required if your spouse does not |
|
|
Female |
|
Month |
Date |
|
|
Year |
|||||||
want Medicaid.) |
|
|
|
|
|
|
|
|
|
|
||||||
Please indicate your spouse’s race(s) ______
Asian= A
White or Caucasian = W Black or African American= B American Indian or Alaska Native= I
Native Hawaiian or Other Pacific Islander= P
Is your spouse a Veteran?
Yes |
No |
Has the spouse served in the armed forces?
Yes |
No |
Hispanic/Latino?
Yes 
 No
No
If yes, specify by circling the code below:
Hispanic Cuban= C
Hispanic Mexican= M
Hispanic Puerto Rican=P
Hispanic Other= H
Does your spouse speak English?

 Yes
Yes
 No
No
What language does your
spouse prefer to speak if not English?
My spouse is a U.S. Citizen.
Yes |
No |
(Not required if your spouse does not want regular Medicaid or if applying for emergency Medicaid.)
*Please provide documentation of citizenship, identity and/or qualified immigration status for any person applying for Medicaid. Persons applying for Emergency Medicaid services only are not required to provide documentation of citizenship or immigration status.
First
Middle
Last
Alien Registration Number
Applicant Only
Does anyone live with you other than your spouse? |
Yes |
No |
If YES,
Who?Relationship:
If YES,
Who?Relationship:
If YES,
Who?Relationship:
Page 9 of 16 |
|
Rev. 08/12 |
|
3. Tell us where you live.
Mailing Address (include apartment number, in care of, etc.)
City, State, County, Zip Code
Home Phone (or number where you can be reached between 8am – 5pm)
Give the address where you actually live, if different than your mailing address:
Do you live in a nursing home? If yes, please indicate the name of the home, city and phone number.
Name:
City:
Phone Number:
Do you and your spouse intend to remain in North Carolina? |
Yes |
|
No |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4. Tell us about your dependents. |
|
|
|
|
||
Does anyone live with you and depend on you (or your spouse) |
|
|
|
|||
to provide at least |
|
Yes |
|
No |
||
If YES, Who? |
|
|
|
|
||
|
|
|
Date of |
|
|
|
Relationship: |
|
|
Birth |
|
|
|
5. Tell us if you or your spouse have any unpaid medical bills.
Do you, your spouse, or children need help paying medical bills |
|
|
for services received during the last three calendar months? |
Yes |
No |
If YES, please provide a copy of the medical bills from the last three months or fill out the information below.
Do you, your spouse, or children have any old, unpaid (medical bills you have not paid yet) medical bills?
♦The medical bills must be less than 2 years old, or
♦ If the medical bills are over 2 years old, you must have |
Yes |
|
No |
made a payment on them within the past 2 years. |
|
|
|
If YES, please provide us with a copy of the medical bills you are being billed for or fill out the information below. Bills used to meet a deductible will not be paid by Medicaid.
*If you do not have copies of your medical bills, please fill out the chart below.
Who owes the bill(s) Please give us the Patient’s name
List the name of the doctor, clinic, hospital, telephone number and city where treated.
Date of medical treatment
Page 10 of 16 |
|
Rev. 08/12 |
|
Form Data
| Fact Name | Detail |
|---|---|
| Intended Applicants | This application is for medical assistance for the Aged, Blind and Disabled, or those seeking Family Planning services. |
| Eligibility for Children and Families | A different application is available for children and families, with certain individuals potentially eligible for Medicaid without being blind, disabled, or older than 65. |
| Submission Process | The application must be completed and submitted to the Department of Social Services in the applicant’s county. |
| Additional Assistance Programs | Applications for Work First Family Assistance, Food Stamps, or Special Assistance must be made in person at the Department of Social Services. |
| Application Date Importance | The date the Department of Social Services receives the complete application is considered the application date. |
| Medicaid Coverage Period | Medicaid can help pay for medical bills incurred up to three months before the month of application. |
| Help with Application | If assistance is needed to complete the application or to obtain required information, contact the Department of Social Services. |
| Medicaid Eligibility Contacts | Questions about eligibility can be answered by local county social services or the DHHS Customer Service Center. |
| Processing Time | Processing times vary: up to 45 days for the elderly, children, or caretakers of a child, and up to 90 days for others under 65 without a child in their care. |
| Applicant Rights and Responsibilities | Applicants have the right to apply for Medicaid, to have help with the application, to be protected against discrimination, and to have their information kept confidential. They are responsible for providing necessary information and reporting any changes in their situation. |
Instructions on Utilizing Nc Application Medicaid
After you complete the Application for Medicaid from the N.C. Department of Health and Human Services, it is essential to understand the process that follows. By filling out this form, you are applying for medical assistance specifically designed for the Aged, Blind, and Disabled or those seeking Family Planning services. Once the form is submitted to the Department of Social Services in your county, it will be reviewed by a caseworker. If additional information is required, you can expect a follow-up communication. Keep in mind that the application date is crucial, as it influences coverage for prior medical bills and determines the start of your Medicaid benefits. Furthermore, if assistance is needed at any stage or further information is necessary, reaching out to the Department of Social Services for guidance is encouraged.
- Read through the entire application form to familiarize yourself with the type of information required.
- In sections 1 through 15, fill in your responses clearly and accurately. This includes personal information, health status, financial circumstances, and any other specifics asked.
- Ensure you do not provide social security numbers, citizenship, or immigration status for individuals in your home not applying for Medicaid.
- If applying for others besides yourself, list all family members who need medical assistance.
- Sign the application form. Remember, an unsigned application cannot be processed.
- Gather and attach any necessary documentation or verifications that support your application if you have them available. This may include medical records, proof of income, or bills related to medical expenses.
- Detach and retain pages 1 through 8 for your records as instructed in the application guidelines.
- Mail or deliver the completed form to the county Department of Social Services office where you reside. It is advisable to find the contact details for your local office ahead of time to avoid delays.
- If you require help completing the application or need to obtain specific information, contact your county's Department of Social Services and request assistance from a Medicaid caseworker.
- After submission, wait for a follow-up call from a caseworker at your county Department of Social Services. They will explain the next steps and may request additional information.
Expect the processing of your application to take some time, depending on your application's specifics. In the meantime, ensure you have provided all the required information to avoid further delays. If your circumstances change after submitting the application, promptly inform your caseworker. Being active and responsive throughout this process aids in achieving a smooth and efficient assessment of your eligibility for Medicaid benefits.
Obtain Answers on Nc Application Medicaid
Who is eligible to apply for Medicaid in North Carolina?
Medicaid in North Carolina is designed to assist various groups including the aged (65 or older), the blind, individuals who require help caring for themselves (those needing long-term care or home care), the physically or mentally disabled, individuals who want family planning services, children under the age of 21, and adults with children in their care. Pregnant women may also qualify. The specific criteria for being considered disabled align with the Social Security definition, which includes being unable to work for at least one year due to a medical condition or having a condition that is expected to result in death.
What expenses does Medicaid cover?
Medicaid can help cover a wide range of medical expenses. These include doctor and hospital bills, prescription drugs (with certain limitations), vision and dental care, Medicare premiums, nursing home care, personal care services, medical equipment, other home health services, mental health care, and services under the Community Alternatives Program (CAP) for eligible individuals.
How do you apply for Medicaid assistance in North Carolina?
Applying for Medicaid requires completing sections 1 through 15 of the application form in a readable manner, signing the form, and bringing or mailing it to the Department of Social Services (DSS) in your county. It’s essential to provide all necessary documentation to support your application. If you require assistance in completing the application or obtaining needed information, the DSS can help. Once submitted, a caseworker will reach out to discuss your application further.
What are the responsibilities of a Medicaid applicant?
Applicants must provide all required information to DSS, report any changes in their situation within ten days, and report if they receive benefits in error. It's also crucial to agree that all information provided is accurate to the best of the applicant’s knowledge, and to understand the legal obligations related to Medicaid ID card usage, reporting of resources, and child or spousal support. Transferring assets without fair market compensation could lead to a period of ineligibility.
What happens if you disagree with a decision made about your Medicaid application?
If you disagree with a decision regarding your Medicaid application, you have the right to request a hearing. This request can be made in person, by telephone, or in writing within sixty days of receiving the decision. Before the hearing, you have the right to examine your case record, and you may have someone represent you, including legal representation. Free legal aid might be available for those who qualify.
What does the Medicaid application process involve regarding citizenship and residency verification?
The county DSS worker will verify the citizenship, identity, and immigration status of the applicant to determine eligibility for specific Medicaid programs. Applicants not applying for Medicaid do not need to undergo this verification. Regular Medicaid requires U.S. citizenship or qualified alien status. If ineligible for regular Medicaid due to citizenship or immigration status, applicants may apply for Emergency Medicaid services. Proof of North Carolina residency is also required, with various documents accepted to establish this.
Common mistakes
When filling out the North Carolina Application for Medicaid, individuals often make mistakes that can delay or negatively impact their application process. Being aware of these common errors can help applicants submit their applications more accurately, ensuring they receive the assistance they need without unnecessary setbacks.
Not listing all family members who are applying for medical assistance. It's vital to include every eligible family member to ensure comprehensive coverage.
Including social security numbers, citizenship, or immigration status for non-applicants in the household. The form specifically instructs not to provide this sensitive information for non-applicants.
Applying with the wrong form. The Application for Medicaid in N.C. is intended for the Aged, Blind, and Disabled or those seeking Family Planning services. Families and children should use a different form, tailored to their specific eligibility criteria.
Delaying the submission of the completed application. Timing is crucial; waiting to submit can preclude the applicant from receiving benefits for past medical bills incurred up to three months before the application date.
Omitting necessary documentation. Failure to attach required documentation or verifications can stall the application process. If uncertain about the required documents, applicants should contact their county Department of Social Services for guidance.
Not signing and dating the application. An unsigned application cannot be processed, further delaying the evaluation and potential approval of benefits.
By avoiding these mistakes, individuals can streamline their Medicaid application process, enhancing their chances of obtaining timely and accurate assistance.
Documents used along the form
When applying for Medicaid through the North Carolina Department of Health and Human Services, several documents and forms might accompany your application to ensure a smooth and complete processing of your request for medical assistance. The complexity of Medicaid eligibility and the array of services covered mean that providing thorough and accurate information is crucial. Here are some essential forms and documents often required alongside the NC Application for Medicaid:
- Proof of Income Documentation: This includes documents like your most recent pay stubs, tax returns, or letters from Social Security, employer statements, or unemployment benefits notices. This information helps determine financial eligibility for Medicaid.
- Proof of Identity and Citizenship: Documents such as a birth certificate, passport, or state-issued identification card are necessary to establish your identity and U.S. citizenship or lawful presence, which are requirements for Medicaid eligibility.
- Proof of Residence: Utility bills, lease agreements, or mortgage statements serve to verify that you reside in North Carolina, ensuring you're applying in the correct state for Medicaid services.
- Medical Records or Doctor’s Statements: If you're applying due to a disability, medical records, and documentation from healthcare providers regarding your condition can be crucial for establishing eligibility under certain Medicaid categories.
- Medicare Information: For individuals who are dually eligible for Medicaid and Medicare, documentation related to Medicare Parts A, B, C, or D, including your Medicare card, is important to coordinate benefits properly.
These documents play a significant role in the assessment of your Medicaid application. Each type of documentation helps to paint a complete picture of your eligibility by demonstrating financial need, residency, identity, and any special circumstances that may affect your eligibility like disability or dual eligibility with Medicare. It’s key to provide this information promptly to avoid delays in the processing of your application and to ensure that you receive the benefits for which you qualify.
Similar forms
The Supplemental Nutrition Assistance Program (SNAP) Application is similar because it also requires applicants to list family members living in the household, their income, and other personal details to determine eligibility for aid. Like the Medicaid form, applicants for SNAP must provide accurate information and may need to undergo a verification process.
The Temporary Assistance for Needy Families (TANF) Application shares similarities, as it is designed for families in need, requiring information on all family members, their finances, and circumstances. Both applications assess needs to provide essential services for well-being.
The Child Health Insurance Program (CHIP) Application is similar because it targets a specific group within Medicaid – children and sometimes their families. It requires detailed information about the household's composition and income to evaluate eligibility for health coverage.
Disability Benefits Application Forms from the Social Security Administration are similar, especially regarding the sections that ascertain disability status. Both require thorough medical documentation and personal information to establish eligibility for benefits.
The Section 8 Housing Choice Voucher Program Application is another comparable document because it requires applicants to list household members, income, and other personal details to determine eligibility for housing assistance. It emphasizes providing truthful and complete information for aid consideration.
The Free Application for Federal Student Aid (FAFSA) shares similarities with the Medicaid application in terms of needing detailed family financial information to determine eligibility for assistance, in this case, financial aid for education.
Dos and Don'ts
Filling out the North Carolina Application for Medicaid carefully is crucial to ensure that the process is smooth and successful. The following are key dos and don'ts that every applicant should keep in mind:
Do:
- Read the entire application carefully before beginning to fill it out to understand what information is required.
- Complete all sections from 1 through 15 legibly, ensuring that your handwriting is clear and readable.
- Gather and attach all necessary documentation or verifications needed to process your application if available.
- Sign and date the application on page 18, acknowledging that your application cannot be processed without your signature.
- Immediately seek help from your county department of social services if you are unable or need help to complete the application or to obtain requested information.
- Contact the Department of Social Services in your county if you have questions about Medicaid programs for which you may be eligible.
- Use the DHHS Customer Service toll-free number for assistance in locating your county DSS office or for other inquiries.
- Include all family members who are applying for medical assistance in the application to ensure all possible assistance is identified.
- Report changes in your situation to the DSS within 10 calendar days of the change.
- Review your rights and responsibilities as outlined in the application to understand the process and requirements fully.
Don't:
- Leave any sections incomplete; answer all questions to the best of your knowledge to avoid delays in processing.
- Provide social security numbers, citizenship, or immigration status for non-applicants living in the home, as it is not required.
- Forget to check for specific information regarding which services are applicable to estate recovery.
- Delay your application submission, as Medicaid coverage can be requested for medical bills incurred up to three months prior to the month of application.
- Be unclear about the purpose of your visit if you choose to apply in person at the DSS office. Specify whether you want a face-to-face interview.
- Hesitate to ask for an appointment if you cannot stay to see a worker to apply for Medicaid on the day you visit the DSS office.
- Use the Medicaid card for anyone not listed on the ID card to avoid prosecution for fraud.
- Transfer resources out of the applicant’s name without receiving fair market value, as it could result in a period of ineligibility.
- Fail to report if you or anyone on the application is involved in an accident, as this could have implications for your Medicaid coverage.
- Omit any child or spousal support which is paid directly to you, as this must be reported to the county department of social services.
Misconceptions
Understanding the North Carolina Application for Medicaid can sometimes be challenging, leading to misconceptions that can affect eligibility and the application process. Here are ten common misconceptions about the NC Medicaid Application form:
- It’s only for the elderly. Medicaid serves not just the elderly but also the blind, disabled, those needing family planning services, and families with children under 21 who may qualify based on other criteria.
- You must provide Social Security numbers for everyone in your household. The form specifically states not to provide Social Security numbers, citizenship, or immigration status for people in the household not applying for Medicaid.
- It’s the same application for everyone. There is a separate application form for children and families, different from the form for the Aged, Blind, and Disabled or those seeking Family Planning services.
- The application process is too complicated. Assistance is available both for completing the application and obtaining the necessary information. Applicants can contact their local Department of Social Services for help.
- You need to visit the office in person to apply. Although in-person application and interviews are available – and can even be requested the same day – mailing the completed application is also an option.
- Medicaid coverage starts the day you submit the application. Coverage can be requested for medical bills incurred up to three months before the application date, but starting coverage depends on the date the Department of Social Services receives the complete application.
- Medicaid won't cover past medical bills. Applicants can request coverage for eligible medical expenses incurred up to three months before the month of application.
- Applying for Medicaid is a one-time opportunity. Individuals have the right to apply for Medicaid anytime, and if found ineligible, they can reapply.
- Medicaid applications can take forever to process. Applications for the elderly, children, or caretakers of a child are processed within 45 days; others could take up to 90 days.
- If not applying for regular Medicaid, applicants must declare their immigration status. Applicants for Emergency Medicaid services only are not required to declare or provide documentation of their immigration status or Social Security Number.
Understanding these points clearly can help navigate the NC Medicaid application process more effectively, ensuring that applicants receive the benefits for which they are eligible without undue delay or hardship.
Key takeaways
Applying for Medicaid in North Carolina is a step toward ensuring you and eligible family members can access medical assistance. Whether you're seeking help for the elderly, blind, disabled, or for family planning services, understanding the process can make it smoother. Here's what you need to know:
- Who's eligible: The application covers assistance for the Aged, Blind and Disabled, along with those seeking Family Planning services. Different forms exist for children and families, highlighting varied eligibility criteria including age, disability status, and need for family planning.
- Application process: It's important to list all family members applying for assistance. However, for non-applicants in your household, steer clear of including sensitive information like social security numbers or immigration status.
- Submitting the application: Once filled, you can submit your application to the Department of Social Services (DSS) in your county. Assistance isn't just limited to Medicaid; inquire about other programs you may qualify for as well.
- Interview rights: Applicants have the right to a face-to-face interview on the same day they visit DSS for medical or financial help. If unable to stay, an appointment can be scheduled.
- Retroactive coverage: Medicaid coverage might be available for medical bills incurred up to three months before the application month. This emphasizes the benefit of submitting your application promptly.
- Support for completion: Help in filling out the application or gathering needed information is available. If you need assistance, don't hesitate to contact DSS.
- Processing timeline: The review period can vary. Applications involving elderly individuals, children, or caretakers may be processed within 45 days, others might take up to 90 days.
- Your rights and responsibilities: Applicants have certain rights, including nondiscrimination and confidentiality, and responsibilities like providing accurate information and reporting changes in circumstances. Understanding these is crucial for maintaining eligibility.
Each step in the Medicaid application process is crucial, from understanding eligibility to timely submission and respecting your rights and responsibilities. If you have questions or need clarification, contacting your local DSS or exploring the provided resources can offer guidance and support.
Popular PDF Forms
Form H1836-a - This document facilitates communication between physicians and the Health and Human Services Commission (HHSC) regarding a patient’s work capability.
Where Can I Get the Disability Forms - Detailed instructions provided on the second page are designed to help avoid delays in the processing of claims.