Blank Ncpdp Billing PDF Template
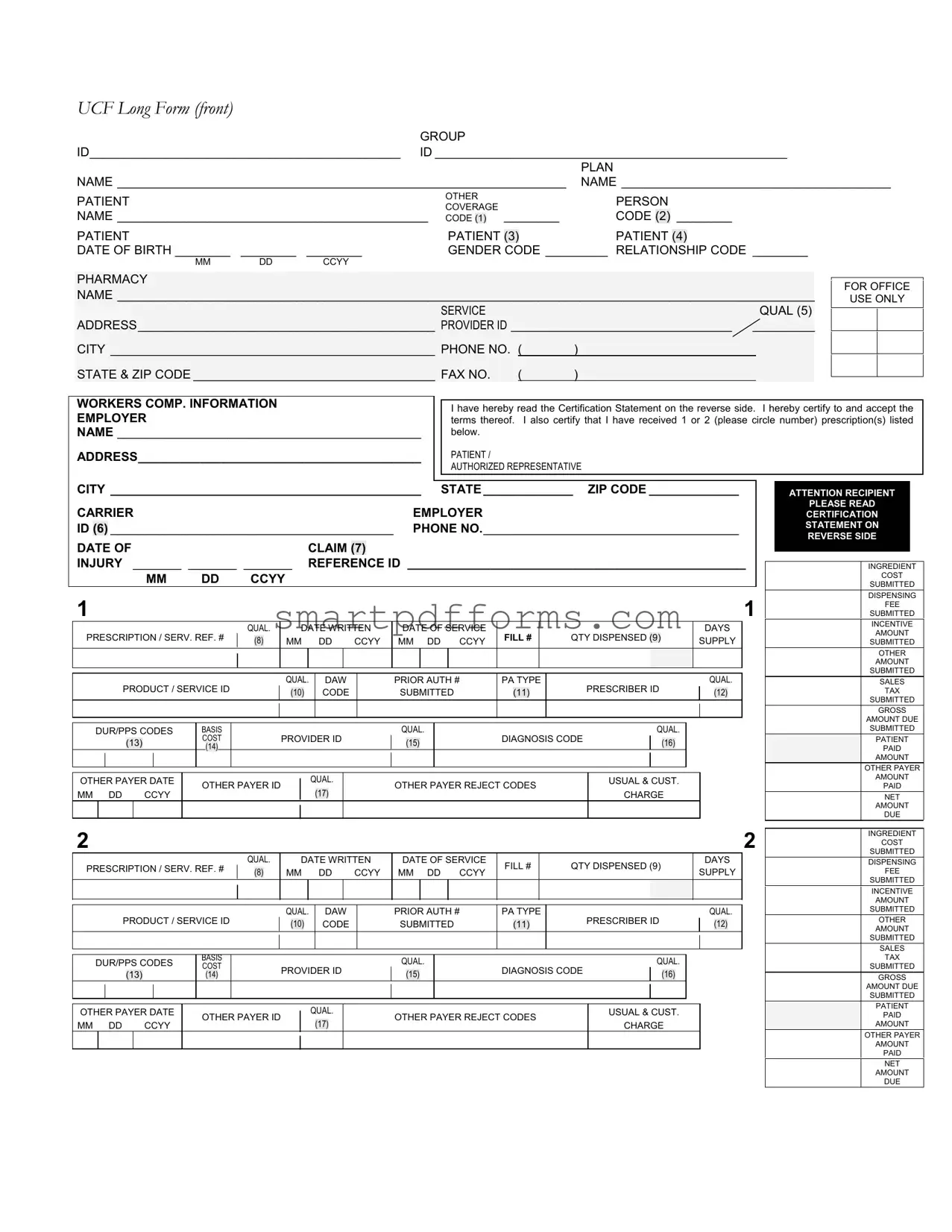
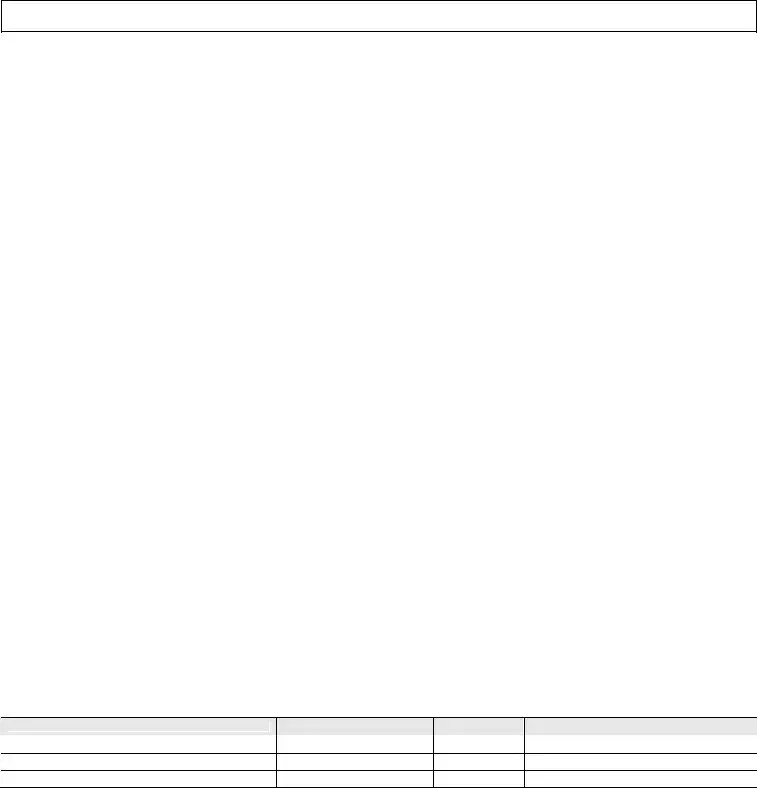
The National Council for Prescription Drug Programs (NCPDP) billing form, notably the UCF Long Form, serves as a multifaceted document central to the pharmacy billing and claims process in the United States. It meticulously records a wide range of information necessary for processing prescription drug claims, covering patient identification, group and plan information, diagnosis and prescriber details, along with specifics about the prescribed medication such as dosage, quantity, and days’ supply. The form also has provisions for workers' compensation information, facilitating claims related to workplace injuries. Its structure allows for the capture of detailed financial aspects, including costs related to the pharmaceutical product, dispensing fees, and any applicable sales tax, while also specifying the amounts paid by the patient or covered by other payers. Moreover, the NCPDP billing form accommodates details for compound prescriptions on the reverse side, ensuring all ingredients are listed for a comprehensive claim. Instructions set on the back highlight the essential steps for filling out the form correctly, emphasizing its role in ensuring accuracy and efficiency in prescription drug billing and reimbursement.
Preview - Ncpdp Billing Form
UCF Long Form (front)
|
|
|
GROUP |
|
|
|
|
|
|
|
|||
ID_____________________________________________ |
ID ___________________________________________________ |
||||||||||||
|
|
|
|
|
|
|
|
|
PLAN |
||||
NAME _________________________________________________________________ |
NAME _______________________________________ |
||||||||||||
PATIENT |
|
|
|
OTHER |
|
|
PERSON |
|
|
|
|
||
|
|
|
COVERAGE |
|
|
|
|
|
|
||||
NAME _____________________________________________ |
CODE |
|
|
________ |
CODE |
(2) |
________ |
||||||
(1) |
|||||||||||||
PATIENT |
|
|
|
PATIENT |
|
|
PATIENT |
|
|
||||
|
|
|
(3) |
(4) |
|||||||||
DATE OF BIRTH ________ |
________ |
________ |
|
GENDER |
CODE _________ RELATIONSHIP CODE ________ |
||||||||
MM |
DD |
CCYY |
|
|
|
|
|
|
|
|
|
|
|
PHARMACY
NAME _____________________________________________________________________________________________________
SERVICE |
|
|
QUAL (5) |
ADDRESS___________________________________________ PROVIDER ID ________________________________ _________ |
|||
CITY _______________________________________________ PHONE NO. ( |
) |
|
|
STATE & ZIP CODE ___________________________________ FAX NO. |
( |
) |
|
FOR OFFICE
USE ONLY
WORKERS COMP. INFORMATION
EMPLOYER
NAME ____________________________________________
ADDRESS_________________________________________
I have hereby read the Certification Statement on the reverse side. I hereby certify to and accept the terms thereof. I also certify that I have received 1 or 2 (please circle number) prescription(s) listed below.
PATIENT /
AUTHORIZED REPRESENTATIVE
CITY _____________________________________________ STATE _____________ ZIP CODE _____________ |
|||||||
CARRIER |
|
|
|
|
EMPLOYER |
||
ID |
(6) |
_________________________________________ PHONE NO._____________________________________ |
|||||
DATE OF |
|
|
CLAIM |
|
|
||
|
|
(7) |
|||||
INJURY _______ _______ _______ |
REFERENCE ID _________________________________________________ |
||||||
|
|
MM |
DD |
CCYY |
|
|
|
1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
||||
PRESCRIPTION / SERV. REF. # |
|
QUAL. |
|
|
DATE WRITTEN |
DATE OF SERVICE |
FILL # |
|
QTY DISPENSED |
|
|
|
|
|
DAYS |
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(9) |
|
|
|
SUPPLY |
|
||||||||||||||||||||
(8) |
MM |
|
DD |
CCYY |
MM DD CCYY |
|
|
||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
PRODUCT / SERVICE ID |
|
|
|
|
QUAL. |
|
DAW |
|
|
PRIOR AUTH # |
PA TYPE |
|
PRESCRIBER ID |
|
QUAL. |
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
(10) |
|
|
CODE |
|
|
SUBMITTED |
|
(11) |
|
|
|
|
|
(12) |
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
DUR/PPS CODES |
BASIS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
QUAL. |
|
|
|
|
|
|
|
|
QUAL. |
|
|
|
|
|
|
||||||||||||||
|
|
|
|
(13) |
|
|
|
|
COST |
|
|
|
|
|
PROVIDER ID |
|
|
|
(15) |
|
|
|
DIAGNOSIS CODE |
|
|
(16) |
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
(14) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
OTHER PAYER DATE |
|
OTHER PAYER ID |
|
|
|
|
QUAL. |
|
|
|
OTHER PAYER REJECT CODES |
|
USUAL & CUST. |
|
|
|
|
|
|||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||
MM DD |
|
|
|
CCYY |
|
|
|
|
|
|
(17) |
|
|
|
|
|
CHARGE |
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|||||||
PRESCRIPTION / SERV. REF. # |
|
QUAL. |
|
|
DATE WRITTEN |
DATE OF SERVICE |
FILL # |
|
QTY DISPENSED (9) |
|
|
|
|
DAYS |
|
|||||||||||||||||||||||||||||||
|
|
(8) |
|
MM |
|
DD |
CCYY |
MM DD CCYY |
|
|
|
|
SUPPLY |
|
||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
PRODUCT / SERVICE ID |
|
|
|
|
QUAL. |
|
DAW |
|
|
PRIOR AUTH # |
PA TYPE |
PRESCRIBER ID |
|
|
|
|
QUAL. |
|
|||||||||||||||||||||||||
|
|
|
|
|
|
|
|
(10) |
|
|
CODE |
|
|
SUBMITTED |
|
(11) |
|
|
|
|
|
|
(12) |
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DUR/PPS CODES |
BASIS |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
QUAL. |
|
|
|
|
|
|
|
|
|
QUAL. |
|
|
|
|
|
|
||||||||||||||
COST |
|
|
|
|
PROVIDER ID |
|
|
|
DIAGNOSIS CODE |
|
|
|
||||||||||||||||||||||||||||||||||
|
|
|
|
(13) |
|
|
|
|
(14) |
|
|
|
|
|
|
|
|
(15) |
|
|
|
|
|
(16) |
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
OTHER PAYER DATE |
|
OTHER PAYER ID |
|
|
|
|
QUAL. |
|
|
|
OTHER PAYER REJECT CODES |
|
USUAL & CUST. |
|
|
|
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||||||||||||
MM DD |
|
|
|
CCYY |
|
|
|
|
|
|
(17) |
|
|
|
|
|
CHARGE |
|
|
|
|
|||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ATTENTION RECIPIENT
PLEASE READ
CERTIFICATION
STATEMENT ON
REVERSE SIDE
INGREDIENT
COST
SUBMITTED
DISPENSING
FEE
SUBMITTED
INCENTIVE
AMOUNT
SUBMITTED
OTHER
AMOUNT
SUBMITTED
SALES
TAX
SUBMITTED
GROSS
AMOUNT DUE
SUBMITTED
PATIENT
PAID
AMOUNT
OTHER PAYER
AMOUNT
PAID
NET
AMOUNT
DUE
INGREDIENT
COST
SUBMITTED
DISPENSING
FEE
SUBMITTED
INCENTIVE
AMOUNT
SUBMITTED
OTHER
AMOUNT
SUBMITTED
SALES
TAX
SUBMITTED
GROSS
AMOUNT DUE
SUBMITTED
PATIENT
PAID
AMOUNT
OTHER PAYER
AMOUNT
PAID
NET
AMOUNT
DUE
UCF Long Form (back)
IMPORTANT I certify that the patient information entered on the front side of this form is correct, that the patient named is eligible for the benefits and that I have received the medication described. If this claim is for a workers compensation injury, the appropriate section on the front side has been completed. I hereby assign the provider pharmacy any payment due pursuant to this transaction and authorize payment directly to the provider pharmacy. I also authorize release of all information pertaining to this claim to the plan administrator, underwriter, sponsor, policyholder and the employer.
PLEASE SIGN CERTIFICATION ON FRONT SIDE FOR PRESCRIPTION(S) RECEIVED
INSTRUCTIONS
1.Fill in all applicable areas on the front of this form.
2.Enter COMPOUND RX in the Product Service ID area(s) and list each ingredient, name, NDC, quantity, and cost in the area below. Please use a separate claim form for each compound prescription.
3.Worker’s Comp. Information is conditional. It should be completed only for a Workers Comp. Claim.
4.Report diagnosis code and qualifier related to prescription (limit 1 per prescription).
5.Limit 1 set of DUR/PPS codes per claim.
DEFINITIONS / VALUES
1. OTHER COVERAGE CODE
0=Not Specified |
1=No other coverage identified |
2=Other coverage |
3=Other coverage |
4=Other coverage |
5=Managed care plan denial |
6=Other coverage |
7=Other coverage |
8=Claim is billing for a copay |
2.PERSON CODE: Code assigned to a specific person within a family.
3.PATIENT GENDER CODE
0=Not Specified |
1=Male |
4. PATIENT RELATIONSHIP CODE |
|
0=Not Specified |
1=Cardholder |
3=Child |
4=Other |
5. SERVICE PROVIDER ID QUALIFIER |
|
Blank=Not Specified |
01=National Provider Identifier (NPI) |
03=Blue Shield |
04=Medicare |
06=UPIN |
07=NCPDP Provider ID |
09=Champus |
10=Health Industry Number (HIN) |
12=Drug Enforcement Administration (DEA) |
13=State Issued |
99=Other |
|
6.CARRIER ID: Carrier code assigned in Worker’s Compensation Program.
7.CLAIM/REFERENCE ID: Identifies the claim number assigned by Worker’s Compensation Program.
8.PRESCRIPTION/SERVICE REFERENCE # QUALIFIER
Blank=Not Specified |
1=Rx billing |
9.QUANTITY DISPENSED: Quantity dispensed expressed in metric decimal units (shaded areas for decimal values).
10.PRODUCT/SERVICE ID QUALIFIER: Code qualifying the value in Product/Service ID
00=Not Specified
03=National Drug Code (NDC)
06=Drug Use Review/Professional Pharm. Service (DUR/PPS) 09=HCFA Common Procedural Coding System (HCPCS) 12=International Article Numbering System (EAN)
1=Prior authorization 4=Exemption from copay
7=Aid to Families with Dependent Children (AFDC)
2=Female
2=Spouse
02=Blue Cross 05=Medicaid 08=State License 11=Federal Tax ID 14=Plan Specific
2=Service billing
01=Universal Product Code (UPC) 04=Universal Product Number (UPN) 07=Common Procedure Terminology (CPT4) 10=Pharmacy Practice Activity Classification (PPAC) 13=Drug Identification Number (DIN)
2=Medical Certification 5=Exemption from Rx limits
12.PRESCRIBER ID QUALIFIER: Use service provider ID values.
13.DUR/PROFESSIONAL SERVICE CODES: Reason for Service, Professional Service Code, and Result of Service. For values refer to current NCPDP data dictionary.
A=Reason for Service |
B=Professional Service Code |
C=Result of Service |
14. BASIS OF COST DETERMINATION |
|
|
Blank=Not Specified |
00=Not Specified |
01=AWP (Average Wholesale Price) |
02=Local Wholesaler |
03=Direct |
04=EAC (Estimated Acquisition Cost) |
05=Acquisition |
06=MAC (Maximum Allowable Cost) |
07=Usual & Customary |
09=Other |
|
|
15. PROVIDER ID QUALIFIER |
|
|
Blank=Not Specified |
01=Drug Enforcement Administration (DEA) |
02=State License |
03=Social Security Number (SSN) |
04=Name |
05=National Provider Identifier (NPI) |
06=Health Industry Number (HIN) |
07=State Issued |
99=Other |
16. DIAGNOSIS CODE QUALIFIER
Blank=Not Specified |
00=Not Specified |
02=International Classification of Diseases (ICD10) |
03=National Criteria Care Institute (NDCC) |
05=Common Dental Term (CDT) |
|
99=Other |
|
01=International Classification of Diseases (ICD9)
04=Systemized Nomenclature of Human and Veterinary Medicine (SNOMED) 07=American Psychiatric Association Diagnostic Statistical Manual of Mental Disorders (DSM IV)
17. OTHER PAYER ID QUALIFIER
Blank=Not Specified |
01=National Payer ID |
02=Health Industry Number (HIN) |
03=Bank Information Number (BIN) |
04=National Association of Insurance Commissioners (NAIC) |
09=Coupon |
99=Other |
|
|
COMPOUND PRESCRIPTIONS – LIMIT 1 COMPOUND PRESCRIPTION PER CLAIM FORM.
Name
NDC
Quantity
Cost
Form Data
| Fact Name | Description |
|---|---|
| Form Usage | This form is utilized for the billing of pharmacy claims, allowing detailed submission of prescription costs and patient information. |
| Patient Identification | It includes fields for identifying patient details such as name, ID, group ID, and date of birth, ensuring the accurate processing of claims. |
| Prescription Details | Prescribers can list each medication, detailing the date written, quantity dispensed, and days supply, along with a unique prescription/service reference number. |
| Provider and Pharmacy Information | The form collects comprehensive information on the service provider, including pharmacy name, address, and provider ID, facilitating direct communication and payment. |
Instructions on Utilizing Ncpdp Billing
Once you have the NCPDP Billing form in front of you, it's crucial to approach filling it out with attention to detail. This form is a key component in processing pharmacy billing and claims. The sections are designed to capture all necessary information about the prescription, patient, pharmacy, and billing specifics. Completing the form accurately ensures a smooth transaction for all parties involved. Below are the steps to fill out the form correctly.
- Begin by entering the Group ID at the top of the form. This identifies the insurance group covering the patient.
- Fill in the ID number, commonly known as the subscriber or member ID, followed by the Plan Name to specify the insurance plan details.
- Under Patient Information, write the patient's name, and if the coverage is under another person, include their details in the corresponding section.
- For each patient listed, input the Date of Birth (MM DD CCYY format) and Gender Code, using the provided codes for gender identification.
- Indicate the Relationship Code to the subscriber to specify the patient's relationship to the policyholder.
- Enter the Pharmacy Name, Service Quality, Address, City, State & Zip Code, and Provider ID. Include the pharmacy's Phone and Fax Numbers.
- If this claim involves workers' compensation, fill out the Employer Name, Address, and pertinent details under the "Workers Comp. Information" section.
- In the Prescription/Service Reference # section, list each prescription's details, including Date Written, Date of Service, Fill #, Quantity Dispensed, and Days Supply.
- Specify the Product/Service ID, including the DAW (Dispense as Written) and Prior Authorization # if applicable.
- Record the prescribing Provider ID and associated Diagnosis Code for each prescription according to the qualifiers listed.
- For billing to another payer before this claim, include the Other Payer Date, ID, and Reject Codes.
- Finally, sign the certification statement, indicating you have read it and understand the claim being submitted.
Tip: Ensure that all sections of the form relevant to your claim are filled in completely. This minimizes the chance of the claim being delayed or rejected due to missing information. After completing the form, review all details for accuracy before submitting it to the insurance carrier or pharmacy benefits manager.
Obtain Answers on Ncpdp Billing
Filling out healthcare forms can sometimes feel like navigating a maze. One such form is the NCPDP billing form, commonly used in pharmacy billing. Let's answer some common questions about this form to make things a bit clearer.
- What is the NCPDP Billing Form?
The NCPDP Billing Form, also known as the Universal Claim Form (UCF), is a standardized document used by pharmacies to submit medication claims to insurance companies or payers. This form captures detailed information necessary for the processing of pharmacy bills, including patient, prescriber, and insurance details, as well as specific data about the prescribed medication or service.
- Why is the Group ID and Plan Name important on the form?
Both the Group ID and Plan Name are crucial because they help identify the patient's health insurance plan. This information ensures that the claim is submitted to the correct insurance company and that the benefits are appropriately applied based on the patient's coverage. Without this information, there could be delays in claim processing or denials.
- What does the "Patient Other Person Coverage" section mean?
This section is used when a patient has coverage under another person, such as a parent or spouse. It requires information about the person who holds the insurance policy covering the patient. This helps in identifying the right policy under which the pharmacy claim should be filed and ensures proper processing and payment of the claim.
- How do I fill out the "Prescription / Serv. Ref. #" and related prescription information?
The "Prescription / Serv. Ref. #" is a unique identifier assigned to each prescription. It's crucial for tracking and processing the claim.
Next, include the "Date Written" and "Date of Service" to indicate when the prescription was prescribed and when the medication was dispensed.
"Fill #", "Qty Dispensed", and "Days Supply" sections specify the fill sequence, quantity of medication dispensed, and how long the medication will last the patient, respectively.
Finally, the "Product / Service ID" and other related fields provide specific details about the prescribed medication, including its identification, any prior authorization, and the prescribing provider's information.
Together, this information facilitates accurate billing and helps in the speedy processing of the pharmacy claim.
- Can you explain the significance of the "Other Payer Amount Paid" and "Net Amount Due" fields?
These fields are critical for claims involving coordination of benefits, where another insurance plan might cover a portion of the costs. The "Other Payer Amount Paid" reflects any amount already covered by another insurer. The "Net Amount Due" is the remaining amount that the primary insurer or patient is responsible for paying. Accurately completing these fields ensures that the claim is processed correctly and reflects the true cost responsibility among all parties involved.
Understanding and correctly filling out the NCPDP Billing Form is essential for the efficient processing of pharmacy claims. It can help avoid delays and ensure that patients receive their medications without unnecessary complications.
Common mistakes
When filling out the NCPDP Billing Form, attention to detail is crucial for ensuring accurate and successful billing. However, common mistakes can impede this process. Here are four errors often encountered:
Incorrectly filling in identification fields: The GROUP ID, ID, and PLAN NAME sections are essential for the identification of the insurance coverage. Mistakes in these areas can lead to claim rejections.
Overlooking patient demographics: Fields such as PATIENT NAME, DATE OF BIRTH, GENDER CODE, and RELATIONSHIP CODE must be precisely completed. Inaccuracies in these fields can lead to discrepancies in patient identification and coverage verification.
Failure to accurately detail prescription information: The form requires specific details about the prescription, including the PRESCRIPTION/SERVICE REF. #, DATE WRITTEN, DATE OF SERVICE, and DAYS SUPPLY. Neglecting to accurately complete these sections can result in processing delays or denials.
Forgetting to include provider and pharmacy information: The PHARMACY NAME, SERVICE QUAL, PROVIDER ID, and DIAGNOSIS CODE are vital for associating the claim with the correct provider and ensuring the pharmacy is reimbursed. Leaving these areas blank or inaccurately filling them can hinder the billing process.
To minimize these errors, thoroughly review all sections before submission, double-check for accuracy, and ensure that no required detail is overlooked. By being diligent, both the patient and the pharmacy benefit from a smoother billing process.
Documents used along the form
When managing pharmacy billing and prescription claims, the NCPDP (National Council for Prescription Drug Programs) Billing Form plays a crucial role in streamlining the process. However, this form doesn't stand alone in the healthcare billing ecosystem. Several other documents often accompany it, ensuring accuracy, compliance, and coordination across different healthcare entities. Let's explore some of these essential forms and documents.
- Prior Authorization Request Form: Used to obtain approval from a health plan before a specific prescription is filled. This ensures the medication is covered under the patient's plan.
- Prescription Drug Claim Form: This form is utilized by patients or healthcare providers to request reimbursement for prescription medications that have been purchased.
- Pharmacy Invoice: Provides a detailed record of the transaction, including medication costs, dispensing fees, and taxes. Pharmacies submit this document for reimbursement.
- Medication Administration Record (MAR): A comprehensive record that tracks all medications administered to a patient, ensuring proper dosage and adherence.
- Compound Prescription Form: Needed when a pharmacist needs to mix ingredients to fill a prescription, detailing each component and its cost.
- Medical Necessity Form: Justifies the need for a specific medication or treatment, often required for high-cost drugs or therapies not typically covered.
- Health Insurance Card: Essential for verifying the patient's coverage details, including plan ID, group number, and benefits.
- Workers' Compensation Claim Form: Required for injuries or conditions related to workplace incidents, detailing the employer's information and the nature of the injury.
The interplay between the NCPDP Billing Form and these additional documents ensures a comprehensive and integrated approach to managing and processing prescription claims. From securing prior authorizations to substantiating medical necessity and facilitating reimbursement, each form contributes to a smooth, efficient healthcare delivery ecosystem, directly impacting patient care and pharmacy operations.
Similar forms
The NCPDP (National Council for Prescription Drug Programs) Billing form is a standardized template used mainly in the pharmacy sector for the submission of drug claims to insurance companies. This form facilitates detailed reporting and billing of pharmaceutical services to ensure accurate reimbursement. Several other documents share similarities with the NCPDP Billing form, each serving an essential role within different sectors of healthcare and insurance processing. Here are ten such documents:
- Medical Insurance Claim Form (CMS-1500): Similar to the NCPDP form, the CMS-1500 is used by healthcare providers to claim payments from health insurance companies, but it focuses on medical, not pharmacy, services. Both forms require detailed patient information and provider details for claim processing.
- Dental Claim Form: Used by dental professionals to seek reimbursements from dental insurance providers. Like the NCPDP form, it includes details about the provider, patient, and services rendered but is tailored towards dental treatments.
- Universal Claim Form: This form is utilized across various healthcare sectors for insurance claim processing, similar to the NCPDP form's role in the pharmacy sphere. Both require comprehensive details about the services provided, including dates and specific codes.
- Workers' Compensation Claim Form: Employed to report an injury or illness related to work for workers' compensation insurance. It shares the need for detailed patient (employee) information, employment details, and the specifics of the injury or treatment with the NCPDP form.
- Automobile Accident Personal Injury Insurance Claim Form: Used following an auto accident to claim for injuries. Like the NCPDP Billing form, it gathers comprehensive details about the claimant's injuries, treatments received, and the healthcare providers involved.
- Home Health Care Insurance Claim Form: For claiming insurance payments for home health care services. Both this form and the NCPDP Billing form collect detailed service descriptions and provider information to ensure accurate reimbursements.
- Long-term Care Insurance Claim Form: This document is essential for claiming benefits under long-term care insurance policies. Like the NCPDP form, it requires detailed reporting on the services provided, including dates and charges, to support the claim.
- Vision Care Insurance Claim Form: Used by optometrists and ophthalmologists to bill for vision care services. Both forms need specific details about the services, including codes and costs, to accurately process the claim.
- Medicare Part D Prescription Drug Claim Form: Specifically designed for Medicare Part D claims, it's similar to the NCPDP Billing form in that it focuses on pharmacy-related claims. Both require detailed medication, dosage, and cost information for processing.
- Healthcare Flexible Spending Account (FSA) Reimbursement Form: Employed by individuals to get reimbursed for out-of-pocket healthcare expenses from their FSA. It shares the requirement for detailed expense documentation, including provider and service information, with the NCPDP Billing form.
Each document, while tailored to its specific sector of healthcare or insurance, shares the core principle of requiring detailed information to support claims. This principle ensures that providers are reimbursed correctly for their services and products, highlighting the importance of accurate and comprehensive documentation in healthcare and insurance processes.
Dos and Don'ts
When filling out the NCPDP Billing form, it's crucial to ensure all information is accurate and complete to prevent any issues with your claim. Here are key dos and don'ts to keep in mind:
- Do double-check the accuracy of all IDs entered, including the Group ID, ID, and Plan Name, to ensure they match the information given by your insurance provider.
- Do carefully review the Certification Statement on the reverse side before signing, to confirm that you understand and agree to the terms.
- Do fill in the Patient, Pharmacy, and Prescription sections completely, providing all required details such as Patient Date of Birth, Gender Code, Relationship Code, Pharmacy Name, and Address, as well as details for each prescription including Date of Service, Quantity Dispensed, and Product/Service ID.
- Do enter the correct codes in designated areas, such as the Prior Authorization Type Code and Service Provider ID Qualifier, to ensure your claim is processed correctly according to the guidelines.
- Don't leave any required fields blank. If a section does not apply, use the designated code for "Not Specified" or "No other coverage identified" as appropriate.
- Don't guess when it comes to codes like the Diagnosis Code Qualifier or Other Payer ID Qualifier. Refer to the definitions/values section for clarification if needed.
- Don't list multiple compound prescriptions on a single claim form. Instead, use a separate form for each compound prescription as instructed.
- Don't enter incorrect information in the Worker's Comp. Information section. This section should only be completed if the claim is related to a workers' compensation injury.
Misconceptions
When discussing the complexities of the NCPDP Billing Form, a myriad of misconceptions commonly arise, predominantly due to its multifaceted nature and the specificity required in filling it out accurately. This form serves as a pivotal document in the healthcare and pharmaceutical sectors, facilitating the billing process between pharmacies and payers for medication dispensation under various conditions and plan types. Unraveling these misconceptions is crucial for professionals in healthcare, pharmacy, and insurance fields to ensure the efficient and correct processing of claims.
Misconceptions about the NCPDP Billing Form:
The form is universally understood and easy to complete without error. In reality, the NCPDP Billing Form's complexity and specificity require detailed knowledge and understanding, often leading to errors if not filled out with care.
It is solely used for billing purposes. Although billing is the primary function, the form also facilitates communication about patient eligibility, prescription details, and other payer contributions, serving a multi-faceted role in patient care and service reimbursement.
All sections of the form must be filled out for every claim. Specific fields are conditional, depending on factors such as whether the claim is for a worker's compensation case or contains a compound prescription, indicating the form's adaptability to various scenarios.
Prior Authorization Type Codes are optional. This section is vital for specific medications or treatments, requiring approval before the service is rendered, ensuring that all necessary permissions are obtained to expedite claim processing.
Every prescribed medication fits neatly into the Product/Service ID Qualifier categories. The reality is that new medications or those not easily categorized require careful consideration to ensure accurate classification, impacting the reimbursement process.
The Diagnosis Code section is only for medical conditions. This section can also include codes for various circumstances that affect the prescription's dispensation, such as worker's compensation or family planning, highlighting its broad applicability beyond medical diagnosis.
One form per patient is sufficient for multiple prescriptions. If compound medications are prescribed, each compound prescription requires a separate form to detail each ingredient's specifics, necessitating multiple forms for accurate processing.
Provider ID and Prescriber ID fields are interchangeable. While both identifiers are crucial, they serve different purposes: the Provider ID relates to the pharmacy or facility submitting the claim, and the Prescriber ID specifically identifies the healthcare professional who wrote the prescription, distinguishing roles within the claim.
Other Payer ID section is irrelevant if the patient has no secondary insurance. This section can include information about any tertiary payers or assistance programs beyond primary and secondary insurance, underscoring the importance of capturing all potential payment sources.
Dispelling these misconceptions fosters a deeper understanding of the NCPDP Billing Form, ensuring more accurate and efficient claims processing. By recognizing the specific nuances and requirements of this document, healthcare providers, pharmacists, and insurers can better navigate the complexities of billing and reimbursement within the healthcare system.
Key takeaways
Understanding the NCPDP Billing Form is crucial for effective pharmacy billing and claims processing. Here are ten key takeaways to ensure accuracy and compliance:
- The Group ID section is vital for identifying the health plan group under which the patient is covered; ensure this information is accurately filled.
- Patient Identification (ID) is a unique number assigned to every individual under a plan. Mistakes here can lead to claim rejections.
- Accuracy in filling out the Plan Name helps in ensuring that the claim is directed to the correct health insurance provider.
- The form has distinct fields for Patient Name and Other Person Coverage Name, highlighting the flexibility in coverage, including dependents or additional insured individuals.
- Date of Birth, Gender Code, and Relationship Code are critical demographic details that impact claim processing, especially for plans with age or relationship-specific benefits.
- Providing the correct Pharmacy Name and Provider ID is essential for claims to be attributed to the correct service provider.
- The form includes workers' compensation information fields, which should only be completed if the claim is related to a workplace injury.
- Every prescription listed requires Service Reference numbers, Quantities Dispensed, and Days Supply, which are vital for calculating the benefit and for inventory control.
- Diagnosis Codes (ICD10) and related qualifiers must be reported with specificity to ensure that the claim aligns with medical necessity requirements.
- Attention to Other Payer ID and Other Payer Reject Codes can expedite the processing of claims involving coordination of benefits.
Conclusively, meticulous attention to detail and a thorough understanding of the form’s requirements can significantly minimize errors in claim submissions. Additionally, staying updated with changes in billing codes and payer requirements is essential for compliance and prompt payment.
Popular PDF Forms
8500-7 - This form is a key document in the certification and ongoing fitness assessment of aviation professionals.
Ldss 3370 - A thorough completion of the Address Area is necessary for the LDSS-3370 form to account for the applicant’s and household members’ residences.
Global Entry Application - Foreign nationals residing in the U.S. must include details of their resident status as part of their application.