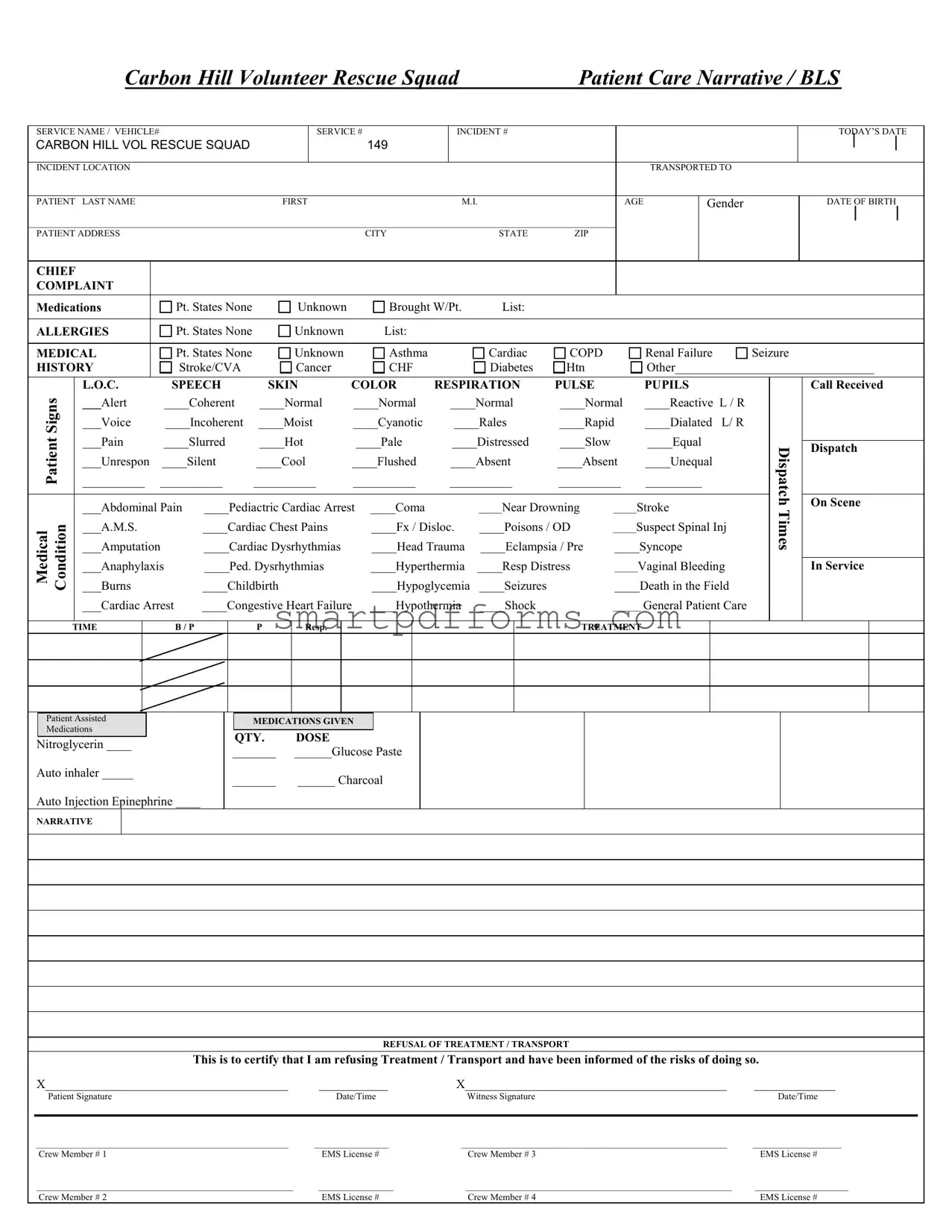
Blank Patient Care Report PDF Template
In the critical encounters between emergency services and patients, the Patient Care Report form stands as an essential document, meticulously crafted to ensure every detail of the patient's condition and the care provided is accurately recorded. Originating from the Carbon Hill Volunteer Rescue Squad, this form encapsulates a variety of information: from basic identifiers like the service name, vehicle number, and incident number, to the more personal details of the patient such as name, age, gender, and medical history. It doesn’t stop there; the form delves into the chief complaint, allergies, and medications, offering a clear snapshot of the patient's health status at the time of the emergency. Additionally, it addresses the medical interventions and treatments administered, including but not limited to, medications given, the dosage, and the patient's response to the treatment. One of the form's critical aspects is the section dedicated to "Refusal of Treatment/Transport", which records a patient's decision to refuse care, ensuring that it’s made with full knowledge of the potential risks involved. This meticulous documentation is not only vital for the continuing care of the patient but also serves as a legal record that can be referred back to if needed. The signatures of the patient (or witness) and the crew members, alongside their EMS license numbers, authenticate the form, adding an extra layer of accountability and transparency to the emergency medical services provided.
Preview - Patient Care Report Form
|
|
|
Carbon Hill Volunteer Rescue Squad |
|
Patient Care Narrative / BLS |
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
SERVICE NAME / VEHICLE# |
|
|
|
SERVICE # |
|
INCIDENT # |
|
|
|
|
|
|
|
|
|
TODAY’S DATE |
||||||||
CARBON HILL VOL RESCUE SQUAD |
|
|
|
149 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
INCIDENT LOCATION |
|
|
|
|
|
|
|
|
|
|
|
|
TRANSPORTED TO |
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
PATIENT |
LAST NAME |
|
|
FIRST |
|
|
|
M.I. |
|
|
AGE |
|
Gender |
|
|
|
|
DATE OF BIRTH |
||||||
______________________________________________________________________________________________________________________________ |
|
|
|
|
|
|
|
|
|
|||||||||||||||
PATIENT ADDRESS |
|
|
|
|
|
CITY |
|
|
STATE |
ZIP |
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CHIEF |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
COMPLAINT |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
Medications |
|
Pt. States None |
Unknown |
|
Brought W/Pt. |
List: |
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
ALLERGIES |
|
Pt. States None |
Unknown |
|
List: |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
MEDICAL |
|
Pt. States None |
Unknown |
|
Asthma |
|
|
Cardiac |
COPD |
|
|
Renal Failure |
Seizure |
|
|
|
||||||||
HISTORY |
|
Stroke/CVA |
Cancer |
|
CHF |
|
|
Diabetes |
Htn |
|
|
Other________________________________ |
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
Signs |
|
L.O.C. |
SPEECH |
SKIN |
COLOR |
RESPIRATION |
PULSE |
|
|
PUPILS |
|
|
|
|
Call Received |
|||||||||
|
___Alert |
____Coherent |
____Normal |
____Normal |
|
____Normal |
____Normal |
____Reactive L / R |
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
___Voice |
____Incoherent |
____Moist |
____Cyanotic |
|
____Rales |
____Rapid |
____Dialated L/ R |
|
|
|
|
|
|
|||||||||
Patient |
|
___Pain |
____Slurred |
____Hot |
|
____Pale |
|
____Distressed |
____Slow |
|
|
____Equal |
|
|
Dispatch |
|
On Scene |
|||||||
|
|
|
|
|
|
|
|
|
|
Dispatch |
||||||||||||||
|
|
___Unrespon |
____Silent |
____Cool |
____Flushed |
|
____Absent |
____Absent |
____Unequal |
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
__________ __________ |
__________ |
__________ |
__________ |
__________ |
_________ |
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
___Abdominal Pain |
____Pediactric Cardiac Arrest |
____Coma |
|
|
_____Near Drowning |
_____Stroke |
|
|
Times |
|
|
|
||||||||||
Medical Condition |
|
___A.M.S. |
|
____Cardiac Chest Pains |
|
____Fx / Disloc. |
____Poisons / OD |
_____Suspect Spinal Inj |
|
|
|
|
|
|||||||||||
|
___Burns |
|
____Childbirth |
|
____Hypoglycemia |
____Seizures |
|
____Death in the Field |
|
|
|
|
|
|||||||||||
|
|
___Amputation |
|
____Cardiac Dysrhythmias |
|
____Head Trauma |
____Eclampsia / Pre |
____Syncope |
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
___Anaphylaxis |
____Ped. Dysrhythmias |
|
____Hyperthermia |
____Resp Distress |
_____Vaginal Bleeding |
|
|
|
|
In Service |
||||||||||||
|
|
___Cardiac Arrest |
____Congestive Heart Failure |
____Hypothermia |
____Shock |
|
______ General Patient Care |
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
TIME
B / P
P
Resp.
TREATMENT
Patient Assisted
Medications
Nitroglycerin ____
Auto inhaler _____
Auto Injection Epinephrine ____
MEDICATIONS GIVEN
QTY. |
DOSE |
_______ |
______Glucose Paste |
_______ |
______ Charcoal |
NARRATIVE
REFUSAL OF TREATMENT / TRANSPORT
This is to certify that I am refusing Treatment / Transport and have been informed of the risks of doing so.
X_______________________________________ |
___________ |
X__________________________________________ |
_____________ |
Patient Signature |
Date/Time |
Witness Signature |
Date/Time |
|
|
|
|
______________________________________________________ |
________________ |
_________________________________________________________ |
___________________ |
Crew Member # 1 |
EMS License # |
Crew Member # 3 |
EMS License # |
_______________________________________________________ |
________________ |
_________________________________________________________ |
____________________ |
Crew Member # 2 |
EMS License # |
Crew Member # 4 |
EMS License # |
Form Data
| Fact Number | Fact |
|---|---|
| 1 | The Patient Care Report form includes a section titled "Patient Care Narrative / BLS SERVICE NAME / VEHICLE#" which records the specific details of the emergency service provided. |
| 2 | Details such as service number, incident number, and date are captured at the beginning of the form for accurate record-keeping. |
| 3 | The form collects comprehensive patient information including last name, first name, middle initial, age, gender, and date of birth. |
| 4 | Patient address details such as city, state, and ZIP code are documented to ensure proper identification and follow-up. |
| 5 | A section on the form is dedicated to recording the patient's chief complaint, along with their medications, allergies, and detailed medical history. |
| 6 | Observations of the patient's condition, including signs like level of consciousness, speech, skin color, respiration, pulse, and pupils, are meticulously noted. |
| 7 | Timelines including when the call was received, dispatch, arrival on scene, and service times are clearly outlined for accountability and response analysis. |
| 8 | Medical conditions and emergencies, ranging from abdominal pain to cardiac arrest, are listed with checkboxes for quick categorization of the incident. |
| 9 | Information about interventions such as administered medications, their quantity, and dose are included to record the immediate care provided. |
| 10 | The form includes a section for documenting the refusal of treatment or transport, capturing both patient and witness signatures to attest to the decision and its risks. |
Instructions on Utilizing Patient Care Report
Filling out the Patient Care Report form is a meticulous process that requires attention to detail to ensure all information is accurately recorded. This document is typically used by emergency medical services (EMS) personnel to document the care provided to a patient during an emergency call. The details captured in this form are crucial for ensuring continuity of care, facilitating billing procedures, and providing a legal record of the patient's condition and the treatment rendered. By following the steps outlined below, EMS personnel can complete the form efficiently and effectively.
- Start by entering the service name, vehicle number, service number, and incident number in the designated fields at the top of the form.
- Write today's date in the "Today's Date" field.
- Record the incident location and the facility name to which the patient was transported in the respective fields.
- Fill in the patient's last name, first name, middle initial, age, gender, and date of birth in the appropriate sections.
- Enter the patient's address, including city, state, and zip code.
- Identify the chief complaint of the patient and mark the appropriate box: states none, unknown, or brought with patient. List any medications if known.
- Check the relevant boxes to indicate if the patient has allergies. List any known allergies.
- For medical history, mark the boxes that apply to the patient's condition, including asthma, cardiac issues, COPD, renal failure, seizures, stroke/CVA, cancer, CHF, diabetes, hypertension, and others as applicable. Specify other conditions if selected.
- Detail the patient's vital signs and observed symptoms, including level of consciousness, speech, skin color, respiration, pulse, and pupils. Use the provided scale and descriptive terms, indicating left/right where necessary.
- Document the call received, dispatch, on scene, and dispatch times in the respective fields.
- Select the medical conditions relevant to the patient's current state from the provided list, marking the appropriate box.
- For treatments administered, record the time, blood pressure, pulse, respiration, and any medications given along with quantities and doses.
- In the narrative section, provide a detailed account of the incident, patient's condition, and the care provided.
- If the patient refuses treatment or transport, ensure the refusal section is completed with the patient's signature, the date/time, and a witness signature with date/time.
- Finally, fill in the crew member details, including names and EMS license numbers, for up to four crew members.
Once completed, the form should be reviewed for accuracy and completeness. It's essential that all sections are filled out thoroughly to provide a comprehensive picture of the patient's emergency care event. This document serves not only as a medical record but also as a critical tool for quality assurance, legal protection, and educational purposes within the EMS community.
Obtain Answers on Patient Care Report
What is a Patient Care Report (PCR) form, and why is it important?
A Patient Care Report form is a comprehensive document used by emergency medical services (EMS) personnel to record all aspects of care and treatment provided to a patient during an EMS response. This form includes details such as the patient's medical history, the nature of their complaint, assessment findings, care provided on scene or en route to a healthcare facility, and medications administered. The PCR is essential for several reasons:- It ensures continuity of care by informing hospital staff and other healthcare providers about the patient's condition and the interventions performed.
- It serves as a legal document that can be used in court to demonstrate the actions taken by EMS personnel.
- It aids in quality improvement efforts by allowing EMS services to review and refine their care processes.
Who fills out the Patient Care Report form?
Typically, the EMS personnel who attended to the patient are responsible for filling out the Patient Care Report form. This includes paramedics and emergency medical technicians (EMTs). The crew member who had the primary responsibility for the patient during the response usually takes the lead in completing the form, ensuring that all necessary information is accurately and thoroughly documented. In some cases, other crew members may contribute information based on their observations and actions.What information is required in the Chief Complaint section of the form?
The Chief Complaint section of the PCR form captures the primary reason or conditions that prompted the patient or bystanders to seek emergency medical help. This section typically includes:- The patient’s stated reason for calling EMS, if able to communicate.
- Any symptoms the patient is experiencing.
- Observations made by the EMS crew, such as visible injuries or signs of distress.
How do EMS personnel record treatments and medications given to the patient?
The Treatment section of the PCR form is designed to document all interventions, procedures, and medications administered to the patient during the EMS response. EMS personnel record each action taken, including:- The type of treatment (e.g., CPR, wound care, splinting).
- Any medications given, including the name, dosage, and route of administration.
- The patient's response to treatments and medications.
What is the Refusal of Treatment/Transport section, and when is it used?
The Refusal of Treatment/Transport section is used when a patient decides not to accept the medical care or transport to a healthcare facility offered by the EMS crew. This section is critically important because it:- Documents the patient's decision to refuse care or transport after being informed of the potential risks.
- Includes the patient's signature (or that of a legal guardian if the patient is a minor or unable to consent) to acknowledge understanding and acceptance of these risks.
- Provides a witness signature (often another crew member) to confirm that the patient was competent to make the decision and was informed adequately.
Can the information on a PCR form be shared with anyone other than healthcare providers?
The information on a PCR form is subject to the privacy regulations established under the Health Insurance Portability and Accountability Act (HIPAA). As such, it is considered protected health information (PHI) and must be handled appropriately. While the primary purpose of the PCR is to inform subsequent healthcare providers about the patient's pre-hospital care, sharing this information with non-healthcare entities or individuals without the patient's consent can violate HIPAA rules. However, there are exceptions under specific circumstances, such as legal investigations or when required by law, where the PCR might be shared beyond healthcare entities.How long do EMS agencies keep Patient Care Reports?
The duration for which EMS agencies must retain Patient Care Reports varies by jurisdiction and is often defined by state laws or regulations. Typically, agencies are required to keep these records for a number of years, which can range from 5 to 10 years or more after the date of service. Retention periods are established to ensure that records are available for legal, regulatory, and quality improvement purposes. Some jurisdictions might require longer retention periods for records involving minors. It's important for EMS agencies to be familiar with and adhere to their specific state's retention requirements.
Common mistakes
Filling out the Patient Care Report (PCR) form accurately is crucial in providing high-quality patient care and ensuring that all relevant medical information is properly documented. However, there are common mistakes that can lead to inaccuracies in these vital records. Here's a breakdown of some of these errors:
- Incorrect or incomplete incident location: It's crucial to provide the full and precise location of the incident to ensure proper documentation and facilitate any necessary follow-up actions.
- Leaving the patient's demographic information blank: Every field including the patient's last name, first name, middle initial, age, gender, and date of birth should be filled out completely to avoid any confusion about the patient's identity.
- Not specifying the patient’s chief complaint accurately: This information guides medical personnel in understanding the patient's primary health concerns and should be described with as much detail as available.
- Failing to list all known medications, allergies, and medical history:
- Medications: Every medication the patient is taking, including dosages when known, should be listed. If the patient states none or is unknown, this should be explicitly recorded.
- Allergies: Known allergies should be meticulously noted. If none are stated or known, this should be clearly indicated.
- Medical History: All known medical history including conditions like asthma, diabetes, or hypertension needs to be thoroughly recorded. An unclear medical history can affect patient care decisions.
- Improper recording of vital signs and symptoms: Accurate recording of the patient's vital signs (e.g., blood pressure, pulse) and observed symptoms (e.g., level of consciousness, skin color) is essential for diagnosing and treating the patient.
- Omitting narrative descriptions: The narrative section should contain a detailed account of the incident, care provided, and the patient's response to treatment. Skipping details can lead to gaps in understanding the patient's condition and care.
- Misuse of medical condition codes: Incorrectly using codes for the patient's medical condition(s) can lead to misinterpretations of the patient's needs and the urgency of the situation.
- Incorrect or incomplete treatment and medications given: It's important to document all treatments administered and medications given, including quantities and doses, to ensure continuity of care and to validate the medical interventions taken.
- Not properly documenting refusal of treatment or transport: If the patient refuses treatment or transport, this must be meticulously documented, including witness signatures, to protect medical personnel legally and to record the patient's decision.
- Failure to verify and sign the form by the crew members: The PCR is not complete until all attending crew members have verified the information and signed the form with their EMS license numbers. This step is crucial for the legal and medical integrity of the document.
Thorough and careful completion of the PCR form is fundamental in ensuring effective patient care and maintaining accurate medical records. Attention to detail can significantly impact the quality of care and the efficiency of medical services provided.
Documents used along the form
When dealing with emergency medical services (EMS), the Patient Care Report (PCR) form is just one of the essential documents used to ensure comprehensive patient care and legal compliance. Besides offering a detailed account of the incident and medical interventions, it's part of a broader set of documents that serve various purposes, from legal documentation to inter-agency communication. Each of these documents plays a critical role in patient care, operational effectiveness, and legal protection for healthcare providers.
- Medical Necessity Form: This document is used to justify the need for the provided medical services. It outlines why the treatment or transport was necessary based on the patient's condition at the time of service.
- Advance Directive Form: This critical document includes any living wills, health care proxies, or DNR (Do Not Resuscitate) orders the patient has made. It's vital for ensuring that the patient's wishes are respected during medical emergencies.
- Refusal of Care Form: Besides the brief section in the PCR, a more detailed refusal of care document may be used. It outlines the patient's decision to refuse specific treatments or transportation after they have been informed of the potential risks and consequences.
- Insurance Information Form: This document collects detailed insurance information from the patient or their family, which is crucial for billing and reimbursement processes.
- Transfer of Care Form: When a patient is transferred from one care setting to another (such as from an ambulance to a hospital), this form documents the exchange. It ensures continuity of care by providing receiving healthcare professionals with immediate access to the patient's care history and current condition.
- Incident Report Form: Used to document any unusual incidents during the call, such as injuries to the EMS crew, equipment failures, or deviations from standard protocol. These reports are crucial for internal review and legal protection.
Together, these documents create a comprehensive and legally sound record of patient care, from prehospital services through to hospital care and billing. By understanding each document's role and ensuring they are properly completed and filed, healthcare providers can guarantee the highest standard of care, streamline operational procedures, and maintain compliance with healthcare regulations.
Similar forms
The Patient Care Report form shares similarities with several other documents used in different fields. Although these documents serve various purposes, they all require detailed, structured information and some level of formal reporting. Here are six such documents:
- Police Incident Report: Similar to the Patient Care Report, a Police Incident Report collects detailed information about an event, including the individuals involved, the location, and a narrative of what occurred. Both documents provide an official record of the event for future reference, accountability, and legal purposes.
- Medical History Form: This form, used in medical settings, gathers comprehensive information about a patient's medical history, medications, and allergies, much like the Patient Care Report does. Both forms are crucial for ensuring that individuals receive appropriate and safe care based on their medical backgrounds.
- Emergency Action Plan: An Emergency Action Plan outlines the steps to be taken in case of an emergency. Like the Patient Care Report, it includes clear, structured information to guide immediate responses and ensure safety, although it is more about planning and response rather than documentation after the fact.
- Medical Research Data Collection Sheet: Used in clinical trials and medical research, this document collects data on participants' health outcomes, treatments received, and side effects, similar to how the Patient Care Report records treatments given and patient responses. Both serve the purpose of documenting and analyzing the effects of medical interventions.
- Insurance Claim Form: This form is submitted to request reimbursement or coverage of medical expenses, similar to how parts of the Patient Care Report might be used to justify the medical necessity of treatments provided. Both require detailed documentation of the service provided, patient information, and a rationale for the services.
- School Incident Report: Similar to the Patient Care Report, a School Incident Report documents incidents involving students, such as injuries or behavioral issues, providing a detailed account of the event, participants, and any actions taken. Both are important for ensuring a clear record is kept for administrative and safety reasons.
Dos and Don'ts
When completing the Patient Care Report form, accuracy and attention to detail are paramount. This document plays a crucial role in ensuring continuity of care, legal documentation, and sometimes, in billing processes. To assist in filling out this form effectively, here are some critical dos and don'ts to bear in mind.
Do:
- Provide comprehensive and accurate patient information: This includes full name, age, gender, and address. Accurately recording this data ensures that the patient’s medical record is complete and coherent.
- Detail the medical history and current medications: If the patient states they have no known allergies or medical conditions, document this clearly. However, if conditions or medications are noted, list them meticulously to inform future medical decisions.
- Describe the incident and patient’s condition clearly: Use objective language to describe the patient's initial condition, symptoms, and any changes that occur. Recording the specifics of the incident location, chief complaint, and vital signs at the scene can be invaluable.
- Record all treatments administered: Include medications given, dosages, and any other interventions. It is vital to document the rationale behind chosen treatments and the patient’s response to them.
Don't:
- Leave sections blank: If a section does not apply, indicate this with a notation such as “N/A” or “None.” Blank sections can lead to questions about the thoroughness of the assessment or the care provided.
- Use ambiguous language: Avoid subjective or vague descriptions. Be precise in your documentation to ensure that anyone reading the report can clearly understand the patient’s condition and the actions taken.
- Include unnecessary personal opinions: The patient care report is a medical document; as such, it should remain professional and objective. Personal observations unrelated to patient care should be omitted.
- Forget to record refusal of treatment or transport: If a patient refuses treatment or transport, it is crucial to document this decision thoroughly, including the patient’s signature, to protect against potential legal repercussions.
By following these guidelines, healthcare providers can ensure that their Patient Care Reports are both accurate and effective in contributing to the well-being and safety of their patients.
Misconceptions
Patients and healthcare professionals alike often carry misconceptions about the Patient Care Report (PCR) form, a critical document in emergency medical services (EMS). Understanding these misconceptions is essential for accurate, comprehensive patient care and documentation.
It's Just Paperwork: A common misconception is that the PCR is merely bureaucratic paperwork. In reality, it provides a crucial narrative of the patient's condition, treatments administered, and the outcome of those treatments. This document supports clinical decision-making and legal documentation.
Only Medical Histories Matter: While medical histories are important, the PCR collects a broad spectrum of information, including current medications and allergies, which can be critical in an emergency. This comprehensive approach helps ensure tailored and safe patient care.
Patient Refusal is Not Important: Documenting a patient's refusal of treatment or transport on the PCR is exceedingly important. It not only provides legal protection for EMS providers but also ensures there is a record of patient autonomy being respected, alongside the risks that were communicated.
Any EMS Personnel Can Complete the Form: Although all EMS personnel are trained in documentation, the responsibility typically falls on the attending or lead medic at the scene. This ensures consistency and accuracy in the details reported.
Details of the Scene Are Irrelevant: The specifics of the incident scene can offer invaluable context for medical professionals who later review the PCR. Details such as the environment of a cardiac arrest or the mechanics of a vehicle collision can influence patient assessment and treatment strategies.
Electronic Forms Have Made PCRs Error-proof: Transitioning to electronic PCRs (ePCRs) has certainly improved legibility and accessibility. However, they are not immune to errors. Accurate data entry is critical to maintain the reliability of the information.
Only Negative Outcomes Need Extensive Documentation: It's a misconception that only procedures that resulted in unfavorable outcomes require detailed documentation. Every intervention, regardless of its outcome, should be meticulously recorded to provide a complete picture of the patient's care journey.
PCRs Are Only Useful for Legal and Billing Purposes: Beyond their necessity for legal protection and billing processes, PCRs serve a vital educational role. Reviewing these reports can highlight areas for improvement in patient care and EMS protocols.
Clarifying these misconceptions is key in appreciating the PCR's role in emergency medical services. Accurate completion and understanding of the PCR ensure the delivery of high-quality patient care, support legal processes, and facilitate continuous improvement in EMS practices.
Key takeaways
Completing the Patient Care Report form accurately is crucial for documenting the care and services provided to a patient by emergency medical services personnel. Here are seven key takeaways about filling out and using this form:
- Ensure accuracy and completeness: Accurate information is the foundation of quality patient care and necessary for legal and regulatory compliance. Ensure all sections, including patient details, incident information, clinical observations, and interventions, are filled out completely.
- Detail the patient's medical history and current condition: Including a comprehensive medical history—such as known illnesses, medications, and allergies—alongside the chief complaint, helps in providing context for the patient’s current condition and potentially guiding treatment.
- Record objective observations: Document clear and objective observations of the patient's condition, including signs of consciousness, speech clarity, skin color, respiration, pulse, and pupil reaction. These details are critical for assessing the patient’s state and determining the appropriate care.
- Describe interventions and medications administered: Note all medical interventions, including medications given, their quantity, and dose. This information is crucial for ongoing care, avoiding medication errors, and understanding the patient’s response to treatment.
- Include refusal of treatment or transport if applicable: If a patient refuses treatment or transport, it is essential to document this decision thoroughly, including the patient's understanding of the risks involved. Ensure the patient and a witness sign the refusal section to acknowledge this choice.
- Use clear, professional language: The Patient Care Report serves as an official document and may be reviewed by various healthcare professionals and legal bodies. Use clear, objective, and professional language to ensure that the report is easily understood by all who read it.
- Sign and date the report: The EMS crew members involved in the patient’s care must sign and date the report, providing their license numbers. This step is vital for accountability and verification purposes.
Properly completing the Patient Care Report is a critical part of emergency medical services. It not only ensures continuity of care by providing valuable information to healthcare providers but also serves as a legal document that can protect the EMS crew and the service organization.
Popular PDF Forms
Tennessee Unemployment Tax - Significant for maintaining the integrity of the unemployment insurance system in Tennessee.
B2b State Farm Claims - Specially crafted to assist in the resolution of insurance claims by allowing repair shops to detail extended vehicle repair needs to State Farm.