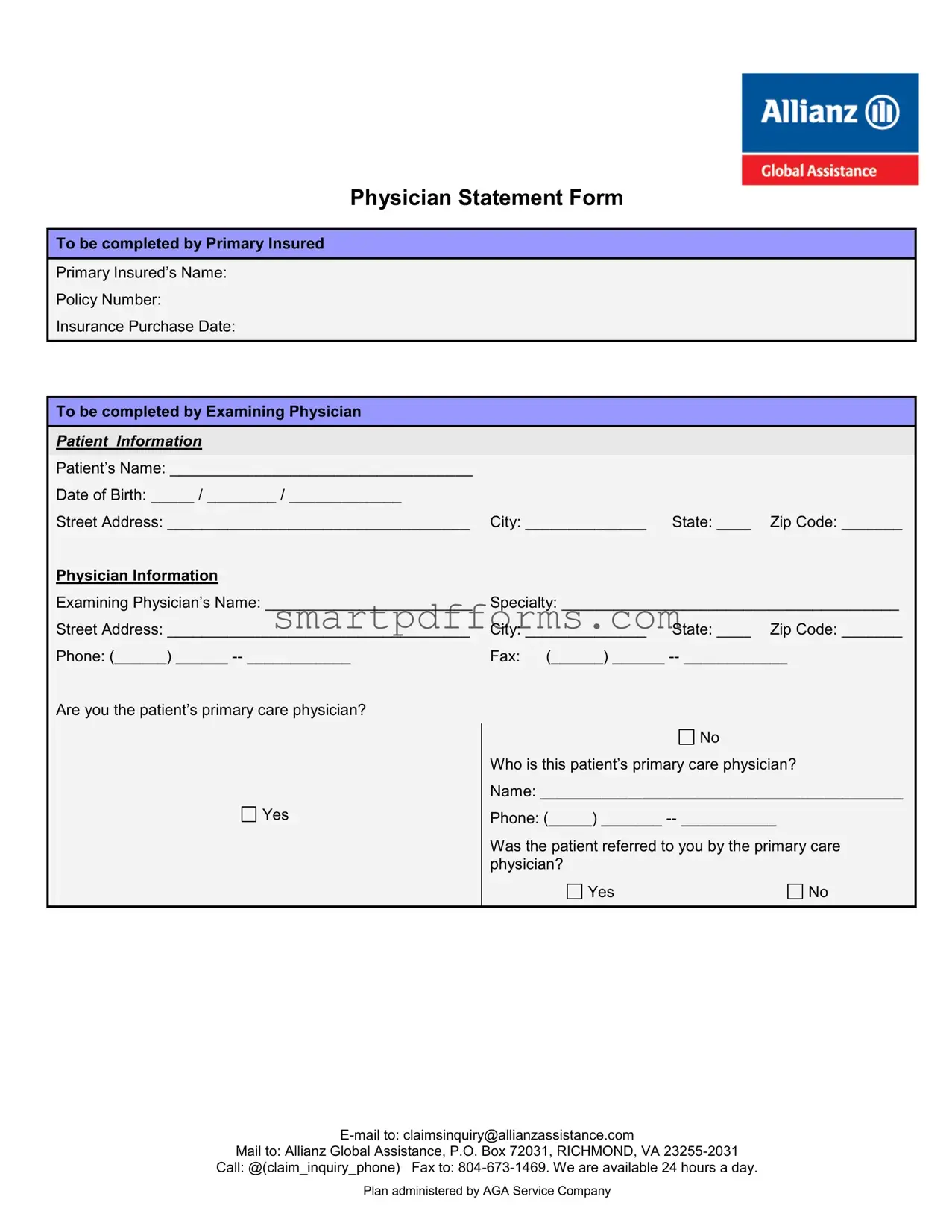
Blank Physician Statement PDF Template
The Physician Statement Form serves multiple functions in maintaining the accuracy and integrity of insurance claims, particularly in the context of travel insurance. This documents is crucial for individuals seeking to submit a claim based on medical grounds; it requires completion by the insured's primary care physician or an examining physician. The form captures detailed patient information, including the insured's name, policy number, and insurance purchase date, as well as the patient's name, date of birth, address, and physician's contact information. Specifically, it calls for a comprehensive report of the patient's diagnosis, the date of examination, any underlying conditions complicating the diagnosed condition, and a history of office visits prior to the insurance purchase. Importantly, this form also requires the physician to indicate whether a medical condition necessitated the cancellation or interruption of the insured's travel plans, providing a space for elaboration on the medical advice given. With the physician's signature and stamp, the form stands as a formal record to support the claimant's case. This careful documentation process aids insurance providers like Allianz Global Assistance in making informed decisions regarding claims, thereby ensuring that the procedure is both fair and efficient for all parties involved.
Preview - Physician Statement Form
Physician Statement Form
To be completed by Primary Insured
Primary Insured’s Name:
Policy Number:
Insurance Purchase Date:
To be completed by Examining Physician
|
|
PATIENT INFORMATION |
|
|
|
|
|
|
|
|
|
|
|
|
|
Patient’s Name: ___________________________________ |
|
|
|
|
|
|
Date of Birth: _____ / ________ / _____________ |
|
|
|
|
|
|
|
|
|
|
|
|
|
Street Address: ___________________________________ |
City: ______________ |
State: ____ |
Zip Code: _______ |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Physician Information |
|
|
|
|
|
|
Examining Physician’s Name: ________________________ |
Specialty: _______________________________________ |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Street Address: ___________________________________ |
City: ______________ |
State: ____ |
Zip Code: _______ |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Phone: (______) ______ |
Fax: (______) ______ |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Are you the patient’s primary care physician? |
|
|
|
|
|
|
|
|
|
No |
|
|
|
|
Who is this patient’s primary care physician? |
|||
|
|
|
Name: __________________________________________ |
|||
|
|
Yes |
Phone: (_____) _______ |
|||
|
|
|
|
|
|
|
|
|
|
Was the patient referred to you by the primary care |
|||
|
|
|
physician? |
|
|
|
|
|
|
Yes |
|
|
No |
|
|
|
|
|
|
|
Mail to: Allianz Global Assistance, P.O. Box 72031, RICHMOND, VA
Call: @(claim_inquiry_phone) Fax to:
Plan administered by AGA Service Company
Patient’s Diagnosis: |
|
|
Did you perform an actual examination? |
Yes |
No |
Date of the exam: ____ / _____ / _________
Please indicate the primary diagnosis for which you examined the patient:
__________________________________________________________________________________________________
__________________________________________________________________________________________________
Date symptoms first appeared or accident occurred: ____ / _____ / _________ |
|
|
Is this condition a complication of an underlying condition? |
Yes (specify below) |
No |
__________________________________________________________________________________________________
Please list the dates of the patient’s office visits in the 120 days before the insurance purchase date, noted above. Circle the dates where you treated the patient for the above stated condition.
|
|
____ / _____ / ___________ |
____ / _____ / ___________ |
____ / _____ / ___________ |
____ / _____ / ___________ |
|
|
|
|
____ / _____ / ___________ |
____ / _____ / ___________ |
____ / _____ / ___________ |
____ / _____ / ___________ |
|
|
|
|
|
|
|
|
|
|
|
|
Did you advise the trip be cancelled or interrupted due to the patient’s medical condition? |
|
|
|
||
|
|
Yes Date: ___ / ___ / _________ |
|
No |
|
|
|
|
|
Please explain why you made this recommendation. |
Please explain why you did not make this recommendation. |
|
|
||
|
|
Provide details on the circumstances and medical diagnosis |
Provide details on the circumstances and medical diagnosis |
|
|
||
|
|
of the patient that you consider relevant to the insured’s |
of the patient that you consider relevant to the insured’s |
|
|
||
|
|
decision to cancel or interrupt their trip due to injury or |
decision to cancel or interrupt their trip due to injury or |
|
|
||
|
|
illness. |
|
illness. |
|
|
|
|
|
________________________________________________ |
________________________________________________ |
|
|
||
|
|
________________________________________________ |
________________________________________________ |
|
|
||
|
|
________________________________________________ |
________________________________________________ |
|
|
||
|
|
________________________________________________ |
________________________________________________ |
|
|
||
|
|
|
|
|
|
|
|
|
|
________________________________________________ |
________________________________________________ |
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
If the patient is the insured, on what date did he/she become medically unable to travel? |
___ / ___ / ________ |
|
|
||
|
|
|
|
|
|
|
|
By my signature and stamp below, I hereby certify that the above is true and correct
Physician Signature: _________________________________________________ Date ____/____/______
Physician Stamp:
Mail to: Allianz Global Assistance, P.O. Box 72031, RICHMOND, VA
Call: @(claim_inquiry_phone) Fax to:
Plan administered by AGA Service Company
Form Data
| Fact Name | Fact Detail |
|---|---|
| Form Purpose | The Physician Statement Form is used for the submission of medical information to support insurance claims. |
| Sections Included | This form includes sections to be completed by both the Primary Insured and the Examining Physician, detailing the insured’s information and the patient’s diagnosis. |
| Submission Methods | It can be submitted via email, mail, phone, or fax, providing flexibility and convenience for the user. |
| Medical Information | The form requests detailed medical information including the primary diagnosis, ICD-9 code, and the history of the patient’s visits. |
| Governing Law | While this form is utilized by Allianz Global Assistance, it is designed to be compliant with general health information laws and privacy standards applicable to medical documentation and insurance claims. |
Instructions on Utilizing Physician Statement
Filling out the Physician Statement form is a straightforward process, yet careful attention to detail is crucial for its accuracy and completeness. The information requested in this form plays a vital role in the evaluation of a claim related to health concerns affecting insurance coverage. By following the steps below, you can ensure that the form is filled out correctly and efficiently, expediting the review process. Once filled, this form should be sent to the appropriate party, based on the provided contact options, to move forward with the claims process.
- Section to be completed by Primary Insured:
Start by entering the Primary Insured’s Name, Policy Number, and the Insurance Purchase Date in the respective fields. - Section to be completed by Examining Physician:
In the Patient Information segment, insert the Patient’s Name, Date of Birth, Street Address, City, State, and Zip Code. - Under Physician Information, fill in the Examining Physician’s Name, Specialty, Street Address, City, State, Zip Code, Phone number, and Fax number. Specify whether you are the patient’s primary care physician by checking the appropriate box and if not, provide the name and phone number of the primary care physician.
- Answer if the patient was referred to you by their primary care physician by marking Yes or No.
- Document the Patient’s Diagnosis including whether you performed an actual examination, the date of the exam, the primary diagnosis, ICD-9 Code, the date symptoms first appeared or the accident occurred, and if the condition is a complication of an underlying condition. If yes, provide details.
- List the dates of the patient's office visits in the 120 days before the insurance purchase date and circle the dates where the patient was treated for the stated condition.
- Indicate if you advised the trip be cancelled or interrupted due to the patient's medical condition, the date of such recommendation, and explain your reasoning or why such advice was not given. Include details on the circumstances and medical diagnosis relevant to the insured's decision to cancel or interrupt their trip.
- If applicable, state the date when the patient became medically unable to travel.
- Finally, the physician must sign and date the form and include their official stamp.
After filling out the form completely, select the most convenient method—email, mail, call, or fax to submit the document to the designated address or number provided. This submission is a critical step to ensure the claim is processed promptly and accurately.
Obtain Answers on Physician Statement
Who needs to complete the Physician Statement form?
The Physician Statement form should be filled out by the examining physician of the individual who is applying for an insurance claim. The first section is to be completed by the primary insured person, which includes their basic information such as name, policy number, and insurance purchase date. The subsequent sections require detailed information from the examining physician including the patient’s information, physician’s information, and specific details about the patient’s diagnosis, treatment, and recommendation regarding travel.
What information is required from the examining physician?
The examining physician is required to provide comprehensive details about the patient. This includes the patient’s name, date of birth, address, and the physician’s details such as name, specialty, contact information, and whether they are the patient’s primary care physician. Importantly, the form asks whether the patient was referred by their primary care doctor, details about the diagnosis including the ICD-9 code, onset of symptoms, treatment history within the 120 days prior to the insurance purchase, and whether the physician recommended cancellation or interruption of the patient’s travel plans due to their medical condition.
How does the physician submit their findings?
The completed form can be submitted through various channels to ensure convenience and efficiency. The physician can send the form via email to claimsinquiry@allianzassistance.com, by mail to Allianz Global Assistance, P.O. Box 72031, RICHMOND, VA 23255-2031, or by fax to 804-673-1469. The form highlights that assistance and further inquiries can be addressed 24 hours a day, indicating support for both the physician and the patient in completing and submitting the necessary documentation.
What happens if the patient was advised against travel due to their condition?
In the scenario where the examining physician advised the patient to cancel or interrupt their trip due to a medical condition, the physician must provide details explaining this recommendation. This includes the date the advice was given, the medical diagnosis, and circumstances leading to this conclusion. Such information is crucial for the insurance provider to assess the validity of the claim and make an informed decision regarding the policyholder's claim. If the patient decides to cancel or interrupt their travel plans based on the physician's advice, providing detailed and accurate information will support their claim for insurance benefits.
Common mistakes
When filling out the Physician Statement form, accuracy and thoroughness are crucial. However, several common mistakes can complicate or delay the processing of the form. Being aware of these pitfalls can ensure a smoother experience:
-
Not verifying patient information: It's essential to double-check the patient's name, date of birth, and address against their medical records to prevent any discrepancies.
-
Overlooking the policy number and insurance purchase date: These details are crucial for the insurance company to connect the form with the right policy.
-
Incomplete physician information: Leaving out the examining physician's name, specialty, or contact details can delay the process, as the insurance company may need to follow up for more information.
-
Skipping primary care physician details: If another doctor referred the patient, it's important to include the primary care physician's name and contact info.
-
Failing to note referral status: Not clarifying whether the patient was referred by the primary care physician can lead to confusion about the context of the examination.
-
Incomplete diagnosis and examination details: The primary diagnosis, ICD-9 code, and information on whether an actual examination was performed are all essential for a comprehensive understanding of the patient's condition.
- The necessity of clearly stating the primary diagnosis cannot be overstated.
- Forgetting to include the ICD-9 code can obscure the diagnosis’ specifics.
- Omitting the examination date leaves a crucial timeline question unanswered.
-
Not detailing the progression: The dates of office visits and the connection of those visits to the stated condition are vital to establish a timeline and relevance of the medical issue.
-
Omitting advice on trip cancellation: Whether or not the trip was advised to be cancelled or interrupted due to medical reasons is critical for insurance claims.
-
Not providing reasoning: If the recommendation was made to cancel or continue the trip, explaining the medical reasoning behind this advice is necessary for the insurance company's assessment.
-
Signature and stamp errors: A missing physician's signature, date, or official stamp can invalidate the entire document, necessitating resubmission.
By being mindful of these common mistakes and addressing them in the Physician Statement form, both physicians and patients can facilitate a smoother and more efficient process for insurance claims.
Documents used along the form
When dealing with health-related claims, especially in the insurance sector, the Physician Statement Form serves as a foundational document. This form provides crucial medical evidence from a healthcare provider about a patient's condition, which is used to assess insurance claims. To support a comprehensive and accurate evaluation of the claim, other documents are often required in addition to the Physician Statement Form. These documents contribute to verifying the claim and providing a complete overview of the patient's health status and the circumstances leading to the insurance claim.
- Medical Records Release Form: This form authorizes the release of a patient's medical records to the insurance company. It ensures the confidentiality of sensitive information while allowing the insurer to obtain a detailed medical history.
- Claimant Statement Form: Completed by the insured, this form gives an account of the incident or health condition leading to the claim. It includes personal insights and descriptions of the symptoms and impacts.
- Proof of Loss Form: Essential for insurance claims, this document provides verified details concerning the extent and nature of the loss or damage incurred. It serves as a formal claim submission.
- Authorization for Release of Information: Similar to the Medical Records Release Form, this document permits broader access to information, including employment, financial, and other personal data relevant to the claim.
- Accident Report Form: If the insurance claim involves an accident, this form details the incident's circumstances, including dates, locations, and any third parties involved.
- Treatment Plan: Provided by the healthcare provider, this outlines the proposed medical treatments for the condition or injury related to the claim. It includes procedures, medications, and expected outcomes.
- Attending Physician’s Statement (APS): More detailed than the initial physician's statement, the APS provides an in-depth analysis of the patient's condition, treatment history, and prognosis. It's especially important for complex cases.
The combination of these documents, along with the Physician Statement Form, creates a comprehensive dossier that enables insurance companies to make informed decisions regarding claims. Each document plays a vital role in illustrating the patient's health scenario, offering a multifaceted view that supports fairness and accuracy in claim resolution. Handling these forms with care and precision ensures that the process is both thorough and efficient, ultimately benefiting all parties involved.
Similar forms
Medical Records Release Form: Similar to the Physician Statement form, a Medical Records Release Form is used to document and authorize the release of a patient's medical records. Both forms include patient information, such as name, date of birth, and address, and require details about the healthcare provider. While the Physician Statement is specific to a physician's findings, the Medical Records Release asks for permission to share the patient's history with other entities.
Disability Claim Form: A Disability Claim Form, like the Physician Statement, gathers detailed information regarding a patient's medical condition, as reported by a healthcare professional. Both documents feature sections on the diagnosis, treatment history, and the patient’s ability to work or perform daily activities. They are essential for assessing benefits eligibility, and in both cases, accuracy and professional verification are paramount.
Life Insurance Application: Although primarily a document filled out by individuals seeking insurance coverage, Life Insurance Applications share similarities with the Physician Statement form, particularly in sections that require disclosing medical conditions or undergoing a medical examination. Both involve providing health information that affects insurance decisions, and both may involve physician insights into the applicant's health status.
Pre-Authorization Request Form: This type of form is used by healthcare providers to request approval from an insurance company before proceeding with treatment. Similar to the Physician Statement, a Pre-Authorization Request Form includes patient identifiers and detailed medical information, such as diagnosis and proposed treatment plans. Both serve as crucial documents for insurance companies to make informed decisions regarding coverage.
Travel Insurance Claim Form: Like the Physician Statement form, a Travel Insurance Claim Form is used in the context of insurance, specifically for claims related to travel interruptions due to medical reasons. Both documents require detailed medical information, including the diagnosis and treatment dates, to support a claim. They are critical for proving the legitimacy of a claim based on health concerns impacting travel.
Dos and Don'ts
When filling out a Physician Statement form, attention to detail and accuracy are vital. Below is a curated list of dos and don'ts to ensure the process is smooth and successful.
- Do verify the patient's personal information (name, date of birth, address) for accuracy to avoid any mismatches in records.
- Do ensure that the examining physician's details are filled out completely, including name, specialty, address, and contact information.
- Do accurately state whether the physician filling out the form is the patient's primary care physician and provide the relevant details if not.
- Do make sure the diagnosis, including the ICD-9 code, is clearly stated and matches the patient's condition and symptoms.
- Do provide detailed information about the patient's office visits, particularly in the 120 days preceding the insurance purchase date, highlighting any visits related to the diagnosed condition.
- Don't leave the section about the patient's primary diagnosis vague or incomplete; be specific to ensure proper processing of the claim.
- Don't forget to indicate whether the condition is a complication of an underlying condition, and if so, provide detailed information about the underlying condition.
- Don't overlook the importance of specifying whether you advised cancelling or interrupting the trip due to the patient's medical condition, including the reasoning behind your recommendation or lack thereof.
- Don't neglect to sign and stamp the document at the end, as this certifies the accuracy and authenticity of the information provided.
Adhering to these guidelines will help ensure that the Physician Statement form is filled out thoroughly and accurately, facilitating a smoother claims process.
Misconceptions
There are several misconceptions about the Physician Statement Form used in insurance claims, especially when it comes to travel insurance or medical insurance claims. Understanding these misconceptions is crucial for both patients and physicians to ensure the process goes smoothly and efficiently.
Only the Primary Care Physician can fill it out: A common misconception is that this form must be completed by the patient's primary care physician (PCP). In reality, any examining physician who has assessed the patient's condition can complete this form. The key requirement is that the physician has enough knowledge of the patient's medical condition to provide accurate information.
It's only about verifying a diagnosis: While confirming the patient's diagnosis is important, the Physician Statement Form serves multiple purposes. It provides a comprehensive picture of the patient's health status, including the onset of symptoms, examination dates, and the impact of the condition on the patient's ability to travel or perform daily tasks. This detail assists insurance companies in making informed decisions regarding claims.
The form is optional for filing a claim: Many people believe that submitting this form is at their discretion. However, for most insurance claims related to health or travel, this form is a critical component of the claim process. Its completion is often mandatory to progress with the claim, as it verifies the medical reason behind the claim.
Any medical documentation can replace the form: People sometimes assume that they can substitute this form with other medical records or notes from the physician. While additional documents can support the form, they cannot replace it. The structured format of the Physician Statement Form is designed to extract specific information that other documents might not provide.
It must be physically mailed to the insurer: Finally, there's a misconception about how to submit this form. While mailing is an option, many insurance companies now accept digital submissions via email or fax. This flexibility helps speed up the claim process, making it more convenient for both the patient and the physician.
Clearing up these misconceptions ensures that both patients and healthcare providers can handle the Physician Statement Form efficiently, leading to smoother insurance claim processes.
Key takeaways
Completing the Physician Statement form accurately is crucial for insurance claims related to health issues affecting travel plans. Here are six key takeaways to ensure the process is handled effectively:
- Accurate Patient Information: It's imperative to fill out the patient's name, date of birth, and contact information accurately to avoid any confusion or claim processing delays.
- Detailed Examination Record: The examining physician must record a thorough examination, including the primary diagnosis and whether the condition could be a complication of an underlying issue. This detailed account supports the insurance claim's validity.
- Clear Documentation of Advice Against Travel: If the physician advises the patient to cancel or interrupt their trip, this must be explicitly noted, including the reasons and the date the advice was given. This documentation is vital evidence supporting the claim.
- History of Patient Visits: Listing dates of the patient's office visits, particularly those relating to the condition in question, within 120 days before the insurance purchase provides critical context for the insurer to assess the claim.
- Reporting Procedure: The form outlines specific ways to submit the completed document, including via email, mail, phone, or fax, ensuring flexibility in submission according to what's most convenient for the physician or patient.
- Physician Verification: The requirement for the physician's signature and stamp at the bottom of the form serves as a formal attestation to the information's accuracy and truthfulness, which is a fundamental requirement for claim processing.
By following these guidelines carefully, patients and physicians can ensure a smoother process in filing and supporting a claim with the insurer, enhancing the likelihood of a favorable outcome.
Popular PDF Forms
Sf 600 Army - The SF 600 form is integral in managing the medical records maintained at hospital or medical facilities.
Bol Pdf - The document’s details enable regulatory compliance, providing all necessary information for legal transportation of goods.