Blank Sbar PDF Template
In healthcare settings, effective communication is paramount, especially when it comes to patient care transitions. The SBAR (Situation, Background, Assessment, Recommendation) template is a tool designed to facilitate this crucial exchange of information among healthcare professionals. By structuring communication in a concise and organized manner, the SBAR form ensures that critical details about a patient's condition are clearly conveyed and understood. It prompts the provider to include essential information such as the patient's name, age, a brief summary of the primary problem, details of admission or post-operative day number, the primary diagnosis, relevant past medical history, and background data. Moreover, the Assessment section guides the healthcare professional to record current vital signs, relevant nursing assessment data, lab values, and any trends in clinical data, necessitating an evaluation of whether the patient's condition is stable, improving, or worsening. Finally, the Recommendations part of the form invites suggestions on how to advance the plan of care, offering a clear avenue for actionable steps that can be taken to address the patient's needs. This format not only streamlines the communication process but also enhances patient safety by ensuring that all team members have a comprehensive and up-to-date understanding of the patient's condition and care requirements.
Preview - Sbar Form
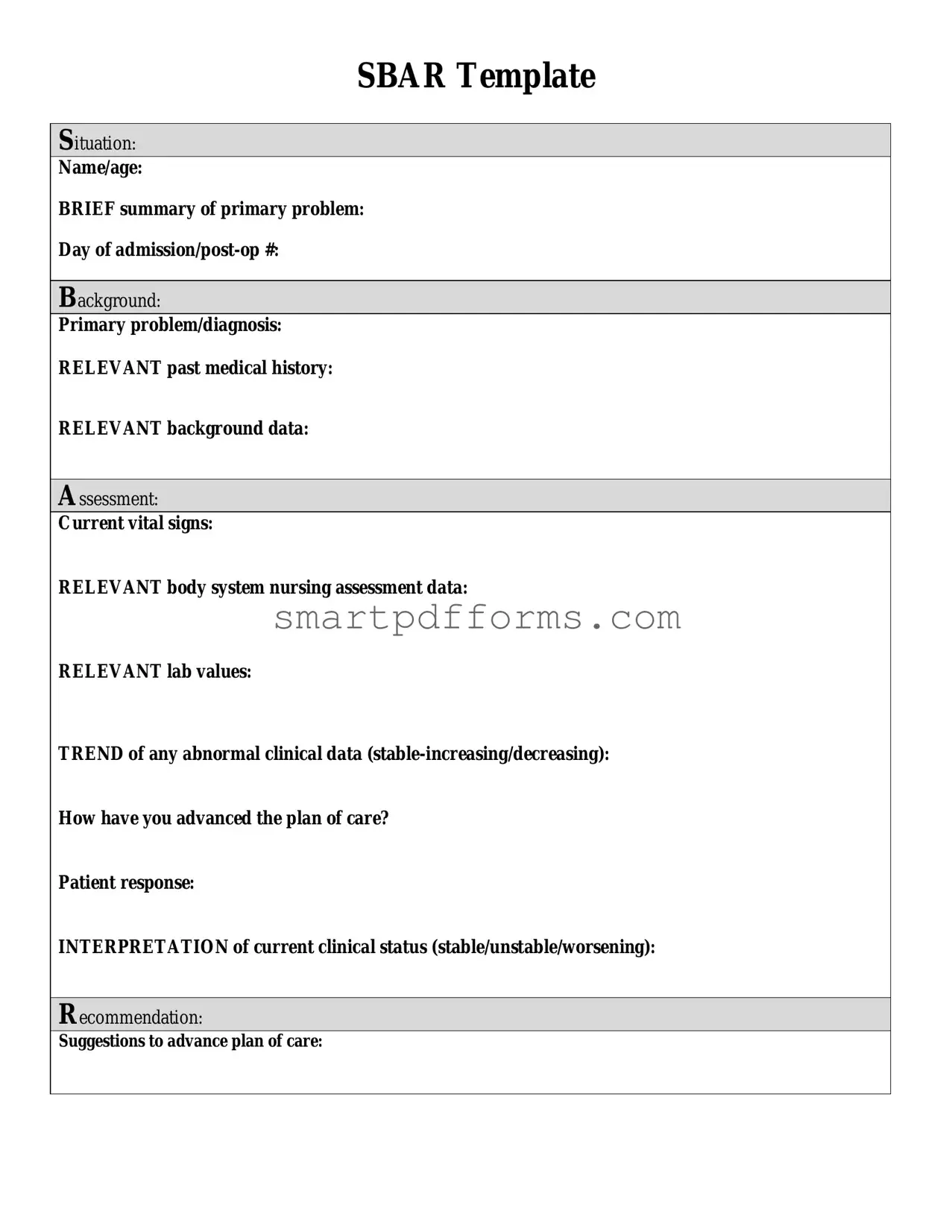
SBAR Template
Situation:
Name/age:
BRIEF summary of primary problem:
Day of
Background:
Primary problem/diagnosis:
RELEVANT past medical history:
RELEVANT background data:
Assessment:
Current vital signs:
RELEVANT body system nursing assessment data:
RELEVANT lab values:
TREND of any abnormal clinical data
How have you advanced the plan of care?
Patient response:
INTERPRETATION of current clinical status (stable/unstable/worsening):
Recommendation:
Suggestions to advance plan of care:
Form Data
| Fact Number | Detail |
|---|---|
| 1 | The SBAR form is utilized to facilitate effective communication among healthcare professionals about a patient's condition. |
| 2 | "Situation" in the SBAR template requires the patient's name, age, and a brief summary of the primary problem. |
| 3 | "Background" provides context including the primary problem/diagnosis, relevant past medical history, and any relevant background data. |
| 4 | In the "Assessment" section, current vital signs, relevant body system nursing assessment data, and lab values are recorded, alongside trends in clinical data. |
| 5 | The form requires an interpretation of the patient's current clinical status as stable, unstable, or worsening under "Assessment." |
| 6 | "Recommendation" seeks suggestions on advancing the plan of care, highlighting the collaborative aspect of patient management. |
| 7 | SBAR stands for Situation, Background, Assessment, and Recommendation, structuring communication to ensure clarity and effectiveness. |
| 8 | This communication tool is widely implemented in healthcare settings to improve safety and quality of patient care. |
| 9 | Its use is not limited to any specific healthcare profession; nurses, doctors, and other healthcare workers utilize it. |
| 10 | The template can be adapted for use in various states and settings, though specific governing laws may apply to healthcare documentation. |
Instructions on Utilizing Sbar
Filling out an SBAR form—a tool used in healthcare to facilitate prompt and appropriate communication—is a critical task that requires accuracy and conciseness. This form assists in structuring communication between healthcare professionals by addressing four key areas: Situation, Background, Assessment, and Recommendation. It ensures that the patient's current state, history, assessment data, and the recommendations for care are clearly presented. To complete the SBAR form effectively, follow these steps to ensure that all necessary information is communicated in an organized manner.
- Situation:
- Name/age: Enter the full name of the patient and their age.
- BRIEF summary of primary problem: Summarize the main reason for the current health issue or hospital admission.
- Day of admission/post-op #: Specify the admission date or the number of days post-operation.
- Background:
- Primary problem/diagnosis: State the diagnosed condition or primary health problem of the patient.
- RELEVANT past medical history: Include significant past medical history that influences the current situation.
- RELEVANT background data: Add any other relevant background information like allergies, previous treatments, etc.
- Assessment:
- Current vital signs: List the most recent vital signs (e.g., blood pressure, heart rate).
- RELEVANT body system nursing assessment data: Provide details of the nursing assessment focusing on the systems affected by the primary problem.
- RELEVANT lab values: Mention significant lab results that impact the assessment or treatment plan.
- TREND of any abnormal clinical data (stable-increasing/decreasing): Describe any changes in the patient's condition, noting improvements or deteriorations.
- How have you advanced the plan of care? Outline actions taken to address the patient's needs as per the care plan.
- Patient response: Document the patient's response to the interventions made.
- INTERPRETATION of current clinical status (stable/unstable/worsening): Assess and categorize the patient's present clinical status.
- Recommendation:
- Suggestions to advance plan of care: Propose any recommendations or modifications to the current plan of care to address ongoing or new issues.
By following these steps, healthcare providers can complete the SBAR form with the necessary details to ensure a clear, concise, and effective communication of the patient's current state and needs. This structured approach promotes better understanding and collaboration among team members, leading to improved patient care outcomes.
Obtain Answers on Sbar
Frequently Asked Questions about the SBAR Form
What is an SBAR form?
An SBAR form is a standardized communication tool used in healthcare settings. It stands for Situation, Background, Assessment, and Recommendation. The form helps clinicians communicate effectively about a patient's condition, ensuring that vital information is conveyed in a clear, concise, and systematic way.
Who uses the SBAR form?
The SBAR form is used by healthcare professionals, including nurses, doctors, and other medical staff. It's commonly used during handoffs between shifts and when a situation requires a brief yet comprehensive exchange of information about a patient's care.
What information is included in the "Situation" section of the form?
The "Situation" section includes the patient's name and age, a brief summary of the primary problem, and the day of admission or post-operation number. This part provides an immediate context of the patient's condition.
What does the "Background" section encompass?
In the "Background" section, relevant details such as the primary problem or diagnosis, relevant past medical history, and other pertinent background data are included. This section gives a snapshot of the patient's medical history related to the current condition.
How comprehensive should the "Assessment" section be?
The "Assessment" section requires current vital signs, relevant body system nursing assessment data, relevant lab values, and trends of any abnormal clinical data (whether stable, increasing, or decreasing). Additionally, it asks about the patient response and an interpretation of their current clinical status, identifying them as stable, unstable, or worsening. This section is meant to provide a current overview of the patient's physical condition and any changes to it.
What is the purpose of the "Recommendation" section?
The "Recommendation" section is aimed at suggesting ways to advance the plan of care for the patient. It may include recommendations for further tests, changes in treatment, or any other actions believed to benefit the patient's recovery. This is where the healthcare professional can propose their next steps based on their assessment.
How does the SBAR form improve patient care?
The SBAR form improves patient care by promoting a standardized method of communication among healthcare professionals. It ensures that all crucial aspects of a patient's condition are discussed in an efficient and understandable manner, thereby reducing errors, enhancing patient safety, and facilitating better clinical outcomes.
Common mistakes
Filling out the SBAR (Situation, Background, Assessment, Recommendation) form is a crucial aspect of healthcare documentation, ensuring effective communication among healthcare professionals regarding patient care. However, common mistakes can hinder the form's effectiveness. Here are eight of these mistakes:
Omitting patient identifiers such as name and age can lead to confusion, especially in facilities where multiple patients might have similar issues or diagnoses.
Providing a non-concise summary of the patient's primary problem in the Situation section can overwhelm the reader with unnecessary information, obscuring the main issues.
Failure to mention the day of admission or post-operative day number may result in a lack of temporal context for the patient's current status.
Omitting relevant past medical history in the Background section can lead to a misunderstanding of the patient's overall health condition and potentially overlook important risk factors.
In the Assessment section, leaving out current vital signs, relevant body system nursing assessment data, or not accurately reporting pertinent lab values can significantly detract from a comprehensive understanding of the patient's condition.
Not documenting the trend of abnormal clinical data (whether stable, increasing, or decreasing) fails to provide a trajectory of the patient's status, which is critical for determining the urgency and type of intervention needed.
Skipping the patient's response to the plan of care or interventions can lead to a gap in understanding the effectiveness of current treatment strategies.
In the Recommendation section, being vague or not offering clear suggestions to advance the plan of care can result in inaction or inappropriate actions taken, potentially endangering the patient's health.
It is essential for healthcare workers to be meticulous when filling out the SBAR form to ensure clear, concise, and actionable communication that enhances patient care and safety.
Documents used along the form
When managing patient care, particularly in settings such as hospitals and clinics, healthcare professionals often use a variety of forms and documents alongside the SBAR (Situation, Background, Assessment, Recommendation) form. This structured method of communication is essential for providing concise and effective information transfer. However, to ensure comprehensive care, the SBAR form is usually accompanied by other documents, each serving a unique purpose in the patient care process. Below is a list of other forms and documents frequently used in conjunction with the SBAR form.
- Medication Administration Record (MAR): A comprehensive record tracking all medications administered to a patient, noting the time, date, dosage, and route. This document is crucial for maintaining medication accuracy and timing.
- Advance Directive: A legal document that outlines a patient's preferences regarding medical treatment and interventions, in case they become unable to make decisions for themselves. This often includes a living will and power of attorney for healthcare.
- Patient Admission Form: A document filled out upon a patient's admission to a facility, detailing personal information, medical history, and the reason for admission. It's the starting point for patient care and record-keeping.
- Care Plan: An individualized plan developed for each patient, outlining goals for treatment, nursing interventions, and expected outcomes. It is used by the healthcare team to ensure coordinated, patient-centered care.
- Fluid Balance Chart: A record keeping track of all fluid intake and output for a patient. This includes drinks, IV fluids, urine output, and any other measurable fluids, ensuring proper hydration levels are maintained.
- Laboratory Test Results: Reports detailing the outcomes of various laboratory tests conducted on a patient, such as blood work, urinalysis, or cultures. These results provide invaluable data for diagnosing and monitoring conditions.
- Vital Signs Chart: A record of a patient's vital signs (including temperature, pulse, respiration rate, and blood pressure) tracked over time. This provides insight into a patient's condition and any potential changes.
- Nursing Notes: Detailed notes taken by nurses providing care. These include observations, the treatment provided, patient responses, and any significant changes in condition. It ensures continuity of care among healthcare providers.
- Discharge Summary: A comprehensive summary prepared when a patient is discharged from the facility. It includes an overview of the stay, treatment received, condition at discharge, and follow-up care instructions.
- Incident Report: A form used to document any unusual or unexpected events affecting patient care or safety. This could involve medication errors, falls, or procedural complications, helping in quality improvement efforts.
Together with the SBAR form, these documents ensure a holistic approach to patient care, facilitating communication among healthcare professionals and streamlining the documentation process. Ensuring each document is accurately filled out and updated is crucial in maintaining high-quality patient care and safety standards.
Similar forms
The SOAP Note is quite similar to the SBAR form. SOAP stands for Subjective, Objective, Assessment, and Plan. Just like the SBAR, the SOAP Note is used in healthcare settings to communicate a patient's status and care plan. Both documents start with a summary of the current situation or the patient's complaint (Subjective in SOAP, Situation in SBAR), include an overview of data such as vital signs and lab values (Objective in SOAP, Background and Assessment in SBAR), proceed with an assessment of the patient's condition, and conclude with a recommendation or plan for care. This structure ensures that healthcare providers have a clear, concise format for exchanging information, enabling effective and efficient care.
The ADPIE Note, which stands for Assessment, Diagnosis, Planning, Implementation, and Evaluation, parallels the SBAR format closely. Both models are systematic approaches used in nursing to streamline patient care. The Assessment phase aligns with SBAR's Situation and Assessment sections, capturing the patient's current condition. Diagnosis and Planning correlate with SBAR's Background, where the diagnosis and relevant past medical history are noted, guiding the plan of care. Implementation in ADPIE is akin to SBAR's Recommendation, suggesting next steps in treatment. Lastly, ADPIE's Evaluation can compare to reflecting on the patient response and clinical status in SBAR, ensuring ongoing patient care optimization.
The ISBAR format is an iteration of SBAR, with the addition of Identification at the very beginning. This means that before explaining the Situation, the healthcare provider identifies themselves, the patient, and their role in the patient's care. This slight modification enhances clarity and ensures that the information is correctly attributed in complex healthcare environments. Beyond this addition, ISBAR follows the same structure as SBAR, focusing on critical information exchange to facilitate effective communication among medical professionals and ultimately improving patient outcomes.
Handoff Communication Tools in healthcare, such as I-PASS, also share similarities with the SBAR format. These tools aim to ensure safe and efficient transfer of patient care information between healthcare providers. I-PASS, for instance, an acronym for Illness severity, Patient summary, Action list, Situation awareness and contingency planning, and Synthesis by receiver, closely mirrors the SBAR structure. It begins with an overview of the patient's situation, includes background information and an assessment, and concludes with recommendations or actions to be taken. This structured approach minimizes the risk of information loss during shift changes or patient transfers, a core principle that underpins the SBAR model as well.
Dos and Don'ts
Filling out the SBAR (Situation, Background, Assessment, and Recommendation) form is crucial for effective communication in healthcare settings. Here are some essential do's and don'ts to consider:
- Do provide concise and relevant information. The SBAR form is designed for clarity and efficiency, so keep your summaries brief and to the point.
- Don't include unnecessary details. Avoid cluttering the form with information that is not directly relevant to the patient's current situation and care needs.
- Do verify all the data you enter. Accuracy is key in healthcare communication. Always double-check names, dates, and medical information to prevent errors.
- Don't use medical jargon or abbreviations that may not be widely understood. Stick to clear, straightforward language to ensure the information is accessible to all members of the care team.
- Do highlight critical changes in the patient's condition. Use the assessment section to clearly state any significant shifts in vital signs, lab values, or overall status.
- Don't forget to mention the patient's response to the current plan of care. This feedback is critical for evaluating the effectiveness of interventions and adjusting the care plan accordingly.
- Do make clear and actionable recommendations. Be specific about any changes or continuations in the care plan, including suggested tests, treatments, or consultations with specialists.
- Don't leave sections blank. If a field is not applicable, mark it as N/A. An incomplete form might lead to misunderstandings or the assumption that crucial information was overlooked.
Correctly filling out the SBAR form is essential for providing high-quality patient care. It ensures that all members of the care team are informed and aligned in their understanding and approach to patient care. By following these guidelines, you can contribute to a more efficient and effective healthcare communication process.
Misconceptions
The SBAR (Situation, Background, Assessment, Recommendation) form is a standardized communication tool widely used in healthcare settings to facilitate clear and concise information transfer about a patient's condition. However, common misconceptions about the SBAR form may lead to its underutilization or misuse. Let's debunk some of these myths.
- Misconception #1: The SBAR form is only for nurses. While it's true that the SBAR technique originally gained popularity within the nursing community, its utility extends far beyond. Physicians, therapists, and other healthcare professionals can also leverage the SBAR structure to streamline communication and improve patient outcomes.
- Misconception #2: SBAR is too time-consuming to fill out. The purpose of the SBAR form is to save time by organizing crucial patient information into a concise, easy-to-understand format. While it may take a few minutes to complete, the clarity it brings to patient communication often saves much more time in the long run.
- Misconception #3: The SBAR form is just for emergencies. Though the SBAR format excels in critical situations by helping healthcare professionals quickly and efficiently share vital information, it's equally helpful in non-emergency settings. Routine updates between shifts or departments can also benefit from the structured approach of SBAR.
- Misconception #4: Using the SBAR form means you're questioning a doctor's judgment. Some healthcare professionals hesitate to use SBAR communication with physicians, fearing it might appear as if they are questioning the doctor's expert judgment. In reality, SBAR is a tool for clarity and ensuring no vital piece of information is missed or misunderstood. It supports the collaborative effort to care for the patient effectively, not undermines it.
- Misconception #5: SBAR is only useful if you have all the information. One of the biggest misconceptions about the SBAR form is that it can only be used if every single field can be completed with the latest information. Actually, the form is designed to highlight the most critical and relevant information at a given time. It's okay if some sections are brief or not applicable; the focus should be on communicating what is known.
- Misconception #6: SBAR communication removes the need for face-to-face interaction. While the SBAR form improves the efficiency and clarity of information transfer, it doesn't replace the need for direct interaction among healthcare team members. Face-to-face or verbal communication is often necessary to discuss nuances that the written form cannot capture. Use SBAR as a complement to, not a replacement for, personal interaction.
Understanding these misconceptions about the SBAR form can significantly impact the effectiveness of communication in healthcare settings. When used correctly, the SBAR tool enhances teamwork, streamlines workflow, and most importantly, improves patient care.
Key takeaways
Filling out and using the SBAR form is critical for ensuring clear and concise communication in clinical settings. Here are key takeaways for utilizing this form effectively:
- Start with a clear identification of the situation by providing the patient’s name and age along with a brief summary of the primary problem. This helps in setting the context right from the beginning.
- Detail the patient's background with emphasis on the primary problem or diagnosis, together with relevant past medical history and background data. This section builds a foundation for understanding the patient's current condition in the context of their overall health history.
- Give a comprehensive assessment, including current vital signs, relevant data from a nursing assessment of body systems, and lab values. Highlighting the trend of any abnormal clinical data (whether stable, increasing, or decreasing) is crucial. This paints a detailed picture of the patient's current health status and any changes that may be occurring.
- Document how you have advanced the plan of care and the patient's response. This illustrates the actions taken in response to the patient’s condition and how the patient has responded to these interventions, shedding light on the effectiveness of the current plan of care.
- Interpret the current clinical status of the patient (stable, unstable, worsening) based on the assessment and the patient’s response. This interpretation guides future care decisions by providing a succinct summary of the patient's current health trajectory.
- End with recommendations to advance the plan of care, offering specific suggestions for adjustments or continuations in the treatment regimen. This proactive approach ensures that the team is always looking ahead to the next steps in the patient's care pathway.
By adhering to these key points, healthcare professionals can utilize the SBAR form to enhance communication within the team, ensuring that all members have a clear, current understanding of the patient's status and care plan. This ultimately contributes to better patient outcomes by facilitating timely and appropriate interventions.
Popular PDF Forms
How to Fill Out Ohio Employee Withholding Exemption Certificate - Assists businesses in leveraging tax exemptions as a strategic tool for financial efficiency and operational growth.
Preschool Enrollment Form Template - Designed to capture detailed information on the child’s eating and allergic conditions to ensure health and safety within the preschool environment.