Blank Sheet Telemetry PDF Template
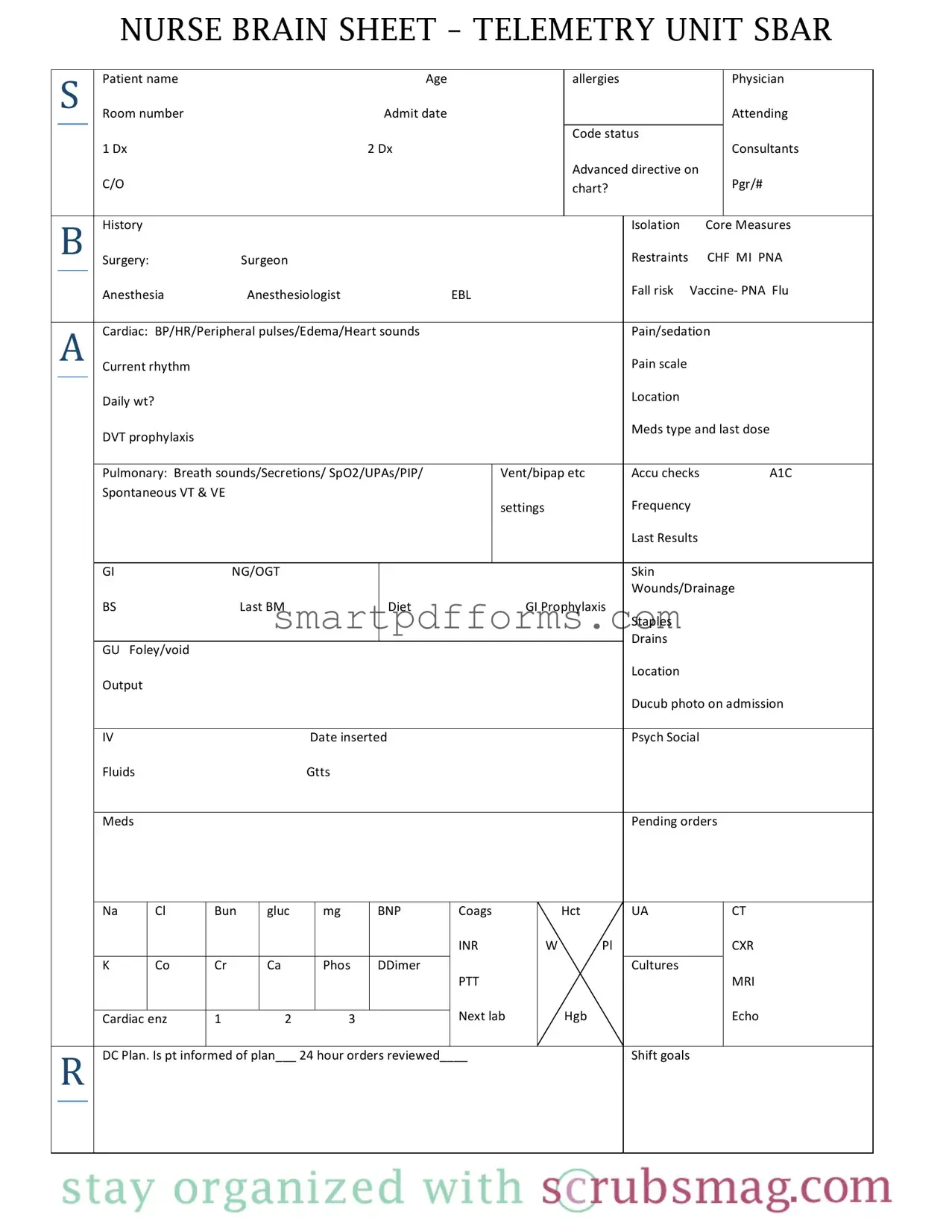
In the complex and fast-paced environment of a telemetry unit, healthcare professionals, particularly nurses, rely heavily on efficient communication and documentation tools to ensure high-quality patient care. Among these tools, the Nurse Brain Sheet for Telemetry Units stands out as a comprehensive form designed to streamline the management of patient information. This form, meticulously structured to cover a broad spectrum of patient data, aids nurses in tracking and sharing critical details. It encompasses sections for basic patient information such as name, age, allergies, attending physician, room number, and admit date, along with more specific medical data including diagnoses, consultants, advanced directives, and code status. The form further delves into core measures, surgical histories including details on surgeons and anesthesia, risk assessments for falls and other complications, medication schedules, and ongoing or necessary procedures. Essential to the monitoring aspect of telemetry nursing, it also includes sections for tracking cardiac and pulmonary statuses, as well as labs and imaging results, enabling a holistic view of the patient’s health. This thorough approach not only facilitates a more organized and efficient workflow for healthcare professionals but also underpins the delivery of patient-centered care by ensuring all relevant health information is systematically gathered and made accessible.
Preview - Sheet Telemetry Form
NURSE BRAIN SHEET – TELEMETRY UNIT SBAR
|
S |
Patient name Age |
|
allergies |
|
Physician |
|||
|
|
|
|
Room number Admit date |
|
|
|
Attending |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Code status |
|
|
|
|
|
|
1 Dx 2 Dx |
|
|
|
Consultants |
|
|
|
|
|
|
|
|
Advanced directive on |
|
|
|
|
|
|
C/O |
|
|
chart? |
|
Pgr/# |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B |
History |
|
|
|
Isolation Core Measures |
|||
|
|
|
|
Surgery: Surgeon |
|
|
Restraints CHF MI PNA |
||
|
|
|
|
Anesthesia Anesthesiologist EBL |
|
|
Fall risk Vaccine‐ PNA Flu |
||
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
||
|
A |
Cardiac: BP/HR/Peripheral pulses/Edema/Heart sounds |
|
|
Pain/sedation |
||||
|
|
|
|
Current rhythm |
|
|
|
Pain scale |
|
|
|
|
|
Daily wt? |
|
|
|
Location |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
DVT prophylaxis |
|
|
|
Meds type and last dose |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
Pulmonary: Breath sounds/Secretions/ SpO2/UPAs/PIP/ |
Vent/bipap etc |
Accu checks A1C |
|||
|
|
|
|
Spontaneous VT & VE |
|
|
|
|
|
|
|
|
|
|
|
settings |
Frequency |
||
|
|
|
|
|
|
|
|
Last Results |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
GI NG/OGT |
|
|
|
Skin |
|
|
|
|
|
|
|
|
|
Wounds/Drainage |
|
|
|
|
|
BS Last BM |
Diet GI Prophylaxis |
|
|
||
|
|
|
|
|
|
|
|
Staples |
|
|
|
|
|
|
|
|
|
Drains |
|
|
|
|
|
GU Foley/void |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Location |
|
|
|
|
|
Output |
|
|
|
|
|
|
|
|
|
|
|
|
|
Ducub photo on admission |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
IV Date inserted |
|
|
Psych Social |
||
|
|
|
|
Fluids Gtts |
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Meds |
|
|
|
Pending orders |
|
|
|
|
Na |
Cl |
Bun |
gluc |
mg |
BNP |
Coags |
|
UA |
CT |
|
|
|
|
|
|
|
|
|
|
INR |
|
|
CXR |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
K |
Co |
Cr |
Ca |
Phos |
DDimer |
|
|
Cultures |
|
|
||
|
|
|
|
|
|
PTT |
|
|
MRI |
||||
|
|
|
|
|
|
|
Next lab |
|
|
Echo |
|||
Cardiac enz |
1 2 3 |
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|||||
R DC Plan. Is pt informed of plan___ 24 hour orders reviewed____ |
|
Shift goals |
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Form Data
| Fact Name | Details |
|---|---|
| Form Purpose | Designed for use in telemetry units to organize and track patient information, focusing on cardiac monitoring. |
| Content Categories | Includes patient identification, medical history, core measures (including surgeries, CHF, MI, PNA), cardiac and pulmonary status, labs, and medication management along with plan of care. |
| SBAR Structure | Incorporates SBAR (Situation, Background, Assessment, Recommendation) for effective communication among healthcare professionals. |
| Advanced Directives and Code Status | Captures critical information regarding patient's advanced directives and code status, ensuring alignment with patient's wishes during care. |
| Governing Laws (For State-Specific Forms) | Governed by state laws regarding patient privacy, health information exchange, and medical record keeping. Specific laws vary by state. |
Instructions on Utilizing Sheet Telemetry
Filling out the Sheet Telemetry form requires attention to detail and organization. The form is utilized to document and monitor various patient details within a telemetry unit, including but not limited to patient identification, medical history, current treatment, and monitoring information. The purpose of correctly filling out this form is to ensure that all relevant patient information is succinctly recorded and easily accessible for healthcare providers, thereby facilitating efficient and effective patient care. Following these steps will guide you through the process of completing the form accurately.
- Start with patient information: Enter the Patient name, Age, Allergies, Physician overseeing the care, and the Room number.
- Document the Admit date, including Attending physician's name, patient's Code status, and primary and secondary diagnoses (1 Dx and 2 Dx).
- Add consultants involved in the case, note if an Advanced directive is on the chart, and record the C/O (Complaints of) and Pgr/# (Page number).
- Under the History section, specify the patient's Isolation status and mark relevant Core Measures, including surgeries, surgeon details, anesthesia, and anesthesiologist information. Also, note any Restraints used and conditions like CHF, MI, or PNA.
- In the Cardiac section, input details about BP/HR/Peripheral pulses/Edema/Heart sounds, the patient's Current rhythm, and Pain scale.
- Under Pulmonary, record observations on Breath sounds, Secretions, SpO2, UPAs, PIP, and Vent/bipap settings, if applicable.
- For the GI (Gastrointestinal) section, detail information about NG/OGT, BS (Bowel Sounds), Last BM (Bowel Movement), patient's Diet, GI Prophylaxis, Staples, and Drains.
- In GU (Genitourinary) list down specifics about Foley/void, Location, Output, and if any Ducub photo on admission.
- Document IV details including Date inserted, Psych Social aspects, Fluids, and Gtts (Drips).
- Under the Meds section, review and include details of Pending orders.
- For lab results, accurately fill in values for Na, Cl, Bun, Gluc, Mg, BNP, Coags, UA, CT, INR, CXR, K, Co, Cr, Ca, Phos, DDimer, Cultures, PTT, MRI, and schedule for the Next lab.
- Finally, note any DC Plan, confirm if the patient is informed of the plan, ensure 24-hour orders are reviewed, and set specific Shift goals.
Completing the Sheet Telemetry form with accurate and current data ensures that all team members have the necessary information to make informed decisions about patient care. The form acts as a crucial tool in monitoring patient progress and adjusting treatment plans as needed.
Obtain Answers on Sheet Telemetry
What is the purpose of the Nurse Brain Sheet – Telemetry Unit SBAR?
The Nurse Brain Sheet – Telemetry Unit SBAR serves as a comprehensive tool for nurses to organize and track critical patient information. It is designed to facilitate effective communication among healthcare providers, ensuring that every member of the care team is up-to-date on the patient's status, needs, and treatment plan. This form helps in monitoring patients in the telemetry unit, focusing on vital signs, diagnoses, medications, and specific care needs.
How should the information on allergies and physician details be entered?
Allergies should be clearly listed with specific details on the type of allergy and the reactions observed. Physician details, including the name and contact, should be updated regularly to ensure any changes in attending healthcare providers are accurately reflected. This ensures the right person is contacted for decisions regarding the patient's care.
What does "Code Status" refer to, and why is it important?
"Code Status" refers to the specific medical interventions a patient has consented to or declined in the event of a major health crisis, such as cardiac arrest. It is crucial for guiding healthcare providers on how to proceed with treatment in emergency situations, respecting the patient’s wishes regarding life-saving measures.
How is the "Current rhythm" section utilized for patient monitoring?
The "Current rhythm" section is crucial for tracking the patient’s heart rhythm, identifying any irregularities or changes that may indicate a need for intervention. Regular updates in this section allow for timely adjustments to treatment plans, ensuring the patient receives appropriate care for their cardiac condition.
What is the significance of including "Fall risk" and how is it assessed?
The inclusion of "Fall risk" is significant as it highlights patients who are at a higher risk of falling, enabling the care team to implement preventive measures. Assessment involves evaluating the patient's mobility, strength, medication side effects, and any history of falls, to tailor a prevention plan accordingly.
When and how should the "24 hour orders reviewed" checkbox be used?
The "24 hour orders reviewed" checkbox should be marked once the nurse has reviewed all orders for the patient within the last 24 hours. This ensures that all new orders, including medications, tests, and procedures, are acknowledged and acted upon promptly, maintaining the continuity and safety of patient care.
Common mistakes
Completing the Nurse Brain Sheet for a Teletry Unit requires accuracy and attention to detail. There are common mistakes that individuals often make when filling out this form. Recognizing and avoiding these mistakes can significantly improve patient care and communication between healthcare professionals.
Not double-checking the patient's information (e.g., name, age, room number) for accuracy. Such errors can lead to serious patient identification mistakes.
Omitting allergies or misunderstanding the severity of allergic reactions. This can pose significant health risks to the patient.
Forgetting to update or accurately record the patient's current medications, last doses, and any changes in their treatment plan. This can result in medication errors.
Overlooking code status or advanced directives on the chart, which are critical in emergency situations to respect the patient's wishes.
Not recording recent vital signs or changes in the patient's condition (e.g., blood pressure, heart rate, oxygen saturation) can lead to missed signs of deterioration.
Failure to list the admitting diagnosis and secondary diagnoses (Dx) correctly, leading to confusion about the patient's treatment and care priorities.
Ignoring or inaccurately marking the patient's pain scale, which is essential for proper pain management and overall care.
Missing updates or entries on patient-specific interventions, such as fall risk precautions, DVT prophylaxis, and dietary restrictions.
Inadequately documenting test results, pending orders, and future lab tests, creating gaps in the patient's medical records and possibly delaying treatment.
By being mindful of these errors and taking the time to accurately complete the Nurse Brain Sheet, healthcare professionals can ensure safer and more effective patient care. Attention to detail, careful review of patient information, and clear communication among the care team are vital components of completing this form correctly.
Documents used along the form
When utilizing the Nurse Brain Sheet – Telemetry Unit, healthcare professionals often incorporate several other critical forms and documents to ensure comprehensive patient care and monitoring. These documents, used in conjunction, provide a multifaceted view of the patient's condition, streamline communication among caregivers, and assist in the planning and execution of care strategies.
- Admission Orders: This document outlines the initial instructions for the patient's care upon admission to the unit. It includes medication orders, diet restrictions, diagnostic tests to be conducted, and any special instructions related to the patient's immediate medical care needs.
- Medication Administration Record (MAR): The MAR is crucial for documenting all medications administered to the patient, including the dosage, route, time, and the person who administered it. It is essential for tracking medication therapy and ensuring patient safety.
- Progress Notes: Maintained by physicians, nurses, and other healthcare professionals, progress notes provide a day-to-day account of the patient's condition, treatment responses, and significant events during their hospital stay. These notes are pivotal for communicating between team members and planning ongoing care.
- Discharge Summary: Upon a patient’s discharge, this document summarizes the patient's hospitalization, including the reason for admission, significant findings, procedures performed, treatment provided, the patient's condition at discharge, and specific instructions for continued care. It ensures a smooth transition from the hospital to the next phase of care.
These documents, when used alongside the Nurse Brain Sheet – Telemetry Unit, create a comprehensive toolkit for managing patient care effectively. They facilitate detailed documentation, support seamless communication among care team members, and ultimately contribute to enhanced patient outcomes.
Similar forms
Medical Admission Note: Both documents compile vital patient information upon admission. The Sheet Telemetry form and Medical Admission Note capture essential Health details like diagnoses (Dx), allergies, and attending physician, organizing critical patient data for healthcare providers.
Patient Care Plan: This document shares similarities with the Sheet Telemetry form by outlining specific patient care requirements, including medication schedules, surgical histories, and any advanced directives present on the chart. Both serve as comprehensive guides for the ongoing care and treatment of patients.
Medication Administration Record (MAR): The Sheet Telemetry form and MAR both track medication types, dosages, and last administered times. This ensures accuracy in medication delivery and enhances patient safety by recording and monitoring pharmaceutical interventions.
Daily Progress Note: Similar to the Sheet Telemetry form, Daily Progress Notes monitor and document patient progress, including response to treatments, changes in condition, and any procedural outcomes. Both are essential for the continuous evaluation and planning of patient care.
Fall Risk Assessment: The Sheet Telemetry form includes fall risk considerations, akin to dedicated Fall Risk Assessments. These documents help identify patients at risk of falls, enabling healthcare providers to implement preventative measures and ensure patient safety.
Advanced Directive Form: Indicating whether an advanced directive is on file within the Sheet Telemetry form echoes the function of a standalone Advanced Directive Form. Both documents identify patient wishes regarding end-of-life care and critical medical interventions.
Laboratory Orders and Results Form: Lab tests, including blood panels and diagnostic imaging orders, are integral to both the Sheet Telemetry form and Laboratory Orders and Results Forms. They assist in diagnosing and monitoring patient conditions, influencing treatment decisions.
Nursing Shift Assessment Form: The comprehensiveness of the Sheet Telemetry form regarding patient observations during a specific shift parallels Nursing Shift Assessment Forms. Nurse-to-nurse communication is facilitated by documenting significant patient data, including vital signs, pain management, and overall status changes.
Dos and Don'ts
When filling out the Nurse Brain Sheet for the telemetry unit, accuracy and clarity are paramount. The information captured on this form is crucial for patient care, communication among healthcare professionals, and ensures consistency in the treatment plan. Below are some guidelines to follow, along with mistakes to avoid, to ensure the form is completed effectively.
Do:- Verify patient information. Double-check the patient's name, room number, and age to prevent any mix-ups in patient care.
- Be precise. When noting diagnoses (Dx), make sure they are current and accurately written.
- Update regularly. Information such as vital signs, medication doses, and lab results change frequently. Keep them updated for the most accurate patient status representation.
- Clarify directives. Ensure that any advanced directives or code status is clearly noted and visible for quick reference during emergencies.
- Detail consultations. List any consultants involved in the patient's care, including their contact information if necessary.
- Record changes. Any changes in the patient's condition or treatment plan should be immediately noted on the form.
- Use legible handwriting. If the form is filled out by hand, write clearly to prevent any misunderstandings or errors in patient care.
- Check for completeness. Before considering the form as finalized, review all sections to ensure no information is missing.
- Follow privacy rules. Handle and store the form in compliance with patient privacy and confidentiality laws.
- Report abnormalities. Any unusual findings or measurements should be flagged for immediate attention from medical staff.
- Rely on memory. Always refer to the patient's medical records or digital system entries to fill in information to avoid errors.
- Skip sections. Even if something seems non-applicable, mark it as such instead of leaving it blank to confirm it was reviewed.
- Use medical jargon. Write in clear, understandable terms to ensure that anyone reading the form, regardless of their medical background, can understand it.
- Ignore discrepancies. If information found in the patient's chart differs from what’s known, investigate the discrepancy and correct it.
- Forget to date the form. Always put the date when the form was filled out or updated, as this can be critical in patient care timelines.
- Avoid communication. If there's something you're unsure about, ask a colleague or supervisor instead of making assumptions.
- Leave out details. When documenting, more information is usually better than less. Do not omit details that could be important.
- Use correction fluid. Mistakes should be crossed out with a single line so the original entry is still readable, and then initialed and dated.
- Delay updates. As soon as new information is received or a change in the patient’s condition occurs, update the form promptly.
- Discard old forms. Keep previous versions of the telemetry form for a set period, as they may be needed for audits or reviews.
Misconceptions
When it comes to medical forms and documentation, it's easy to overlook or misunderstand their complexity and the purpose behind their design. One such critical document in healthcare settings, especially in telemetry units, is the Nurse Brain Sheet – Telemetry Unit. However, there are misconceptions about the Sheet Telemetry form that need clarification:
It's just another form to fill out. This is not just another piece of paperwork. The telemetry form is a crucial tool for nurses, providing a snapshot of the patient's condition, treatments, and needs, which helps in delivering quality care.
It's only for nurses. While primarily used by nurses, the information on the form is vital for the entire healthcare team, including physicians, specialists, and therapists, facilitating a comprehensive approach to patient care.
It's too complicated to be useful. Though detailed, the form's complexity is necessary to capture all relevant data for patients in a telemetry unit, where conditions can change rapidly. Proper training can help staff efficiently use this tool.
Electronic versions are always better. While electronic health records (EHRs) have their advantages, paper forms like the telemetry sheet can be more accessible and quicker to reference in some situations, highlighting the importance of flexibility in documentation methods.
It's only about patient data. Beyond clinical data, the form includes sections for planning care, coordinating with the team, and patient education, emphasizing the holistic approach to patient health.
Only current data matters. Historical information, such as past diagnoses and surgeries, can significantly impact patient care decisions and outcomes, which is why it is included in the form.
All sections must be filled for every patient. While comprehensive, not every section of the form will apply to all patients. Clinicians need to use their judgement to fill out the relevant parts based on each patient’s specific condition and needs.
It replaces verbal communication between staff. While the telemetry sheet is an important tool, it does not replace the need for direct communication among healthcare providers. It is a supplement to ensure all team members are informed.
It is only for initial assessment. The form is designed for continuous use and updating throughout the patient's stay in the telemetry unit, not just at admission, ensuring ongoing accurate monitoring and treatment adjustments.
Less important sections can be skipped. Every section of the form has been designed with a purpose, including seemingly minor details like patient allergies or last bowel movement, which can have significant implications for care and treatment plans.
Understanding and addressing these misconceptions about the Sheet Telemetry form can improve the effectiveness of patient care in telemetry units by ensuring that the form is used as intended – as a comprehensive and dynamic tool for patient management.
Key takeaways
Filling out and using the Nurse Brain Sheet for a telemetry unit requires attention to detail and clear communication. Here are key takeaways to ensure its effectiveness:
- Accuracy is crucial: Make sure all patient information, including name, age, allergies, and physician, is accurately recorded. This sets the foundation for personalized care.
- Maintain up-to-date records: Updating the form with the most recent admit date, attending, code status, and diagnoses helps keep the healthcare team informed about the patient's current state and medical history.
- Don't overlook the Advanced Directive status and Code Status: These are vital in making informed decisions in critical situations.
- Include a comprehensive medication review, detailing meds type and last dose, to prevent drug interactions and ensure timely dosing.
- Regularly assess and document the patient's core measures, including surgical history, and pertinent health metrics such as BP/HR and current rhythm, to monitor changes in condition.
- Risk assessments for falls, DVT, and other conditions should be completed and updated to minimize patient risks.
- Note lab results and pending orders clearly to ensure all team members are up to date with the patient's condition and know what actions are needed next.
- Communication with the patient and their family about the DC Plan and ensuring the patient is informed about their care plan supports patient-centered care.
By diligently maintaining the Nurse Brain Sheet for patients in a telemetry unit, healthcare providers ensure the highest level of care through consistent tracking and assessment of patient needs and responses to treatment. This structured approach to documentation aids in efficient care coordination and enhances patient safety.
Popular PDF Forms
Ks Dept of Corrections - Includes special provisions for managing visitation rights of inmates identified as sex offenders, aligning with broader security measures.
Police Vehicle Inspection Form Template - Addressing both minor and significant vehicle components, this checklist ensures a holistic inspection is conducted, maintaining high operational standards.
Cms Website - Information regarding any criminal offenses related to program involvement by owners or managers must be disclosed.