Blank Texas Dwc069 PDF Template
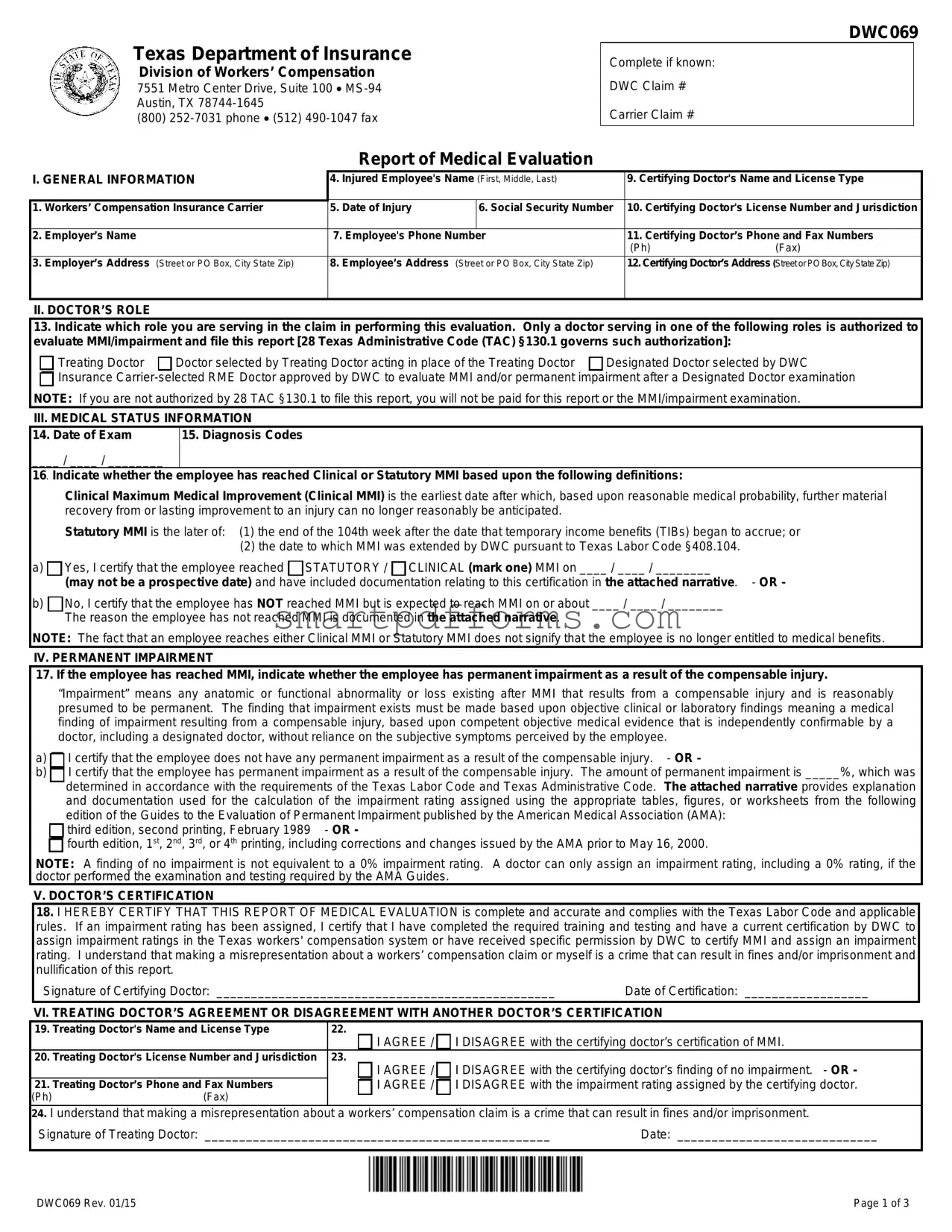
The Texas DWC069 form, officially titled "Report of Medical Evaluation," serves as a critical piece of documentation within the Texas workers' compensation system, a program overseen by the Texas Department of Insurance Division of Workers’ Compensation. This form is utilized for reporting a pivotal aspect of a worker's compensation claim: the medical evaluation concerning Maximum Medical Improvement (MMI) and potential permanent impairment. It requires completion by a select group of medical professionals, including the treating doctor, a doctor selected by the treating doctor, a designated doctor chosen by the Texas Department of Insurance, Division of Workers’ Compensation (DWC), or an insurance carrier-selected Required Medical Examination (RME) doctor, under specific circumstances outlined by the regulation. These professionals must certify whether an injured employee has reached MMI, the point at which no further recovery from or significant improvement to an injury is expected, and assess if there is any lasting impairment. The form further guides on the determination of clinical or statutory MMI and documents the extent of permanent impairment, should it exist, based on objective clinical findings in accordance with predefined criteria established by the Texas Labor Code and Texas Administrative Code. Furthermore, it outlines the necessary steps for filing the form, the importance of timely submission, and the detailed instructions for doctors completing this evaluation, signifying its role as a comprehensive tool for ensuring the accurate assessment and processing of workers' compensation claims in Texas.
Preview - Texas Dwc069 Form
Texas Department of Insurance
Division of Workers’ Compensation
7551 Metro Center Drive, Suite 100
(800)
Report of Medical Evaluation
DWC069
Complete if known:
DWC Claim #
Carrier Claim #
I. GENERAL INFORMATION |
4. Injured Employee's Name (First, Middle, Last) |
|||
|
|
|
|
|
1. |
Workers’ Compensation Insurance Carrier |
5. |
Date of Injury |
6. Social Security Number |
|
|
|
|
|
2. |
Employer’s Name |
7. Employee's Phone Number |
|
|
|
|
|
|
|
3. |
Employer’s Address (Street or PO Box, City State Zip) |
8. |
Employee’s Address (Street or PO Box, City State Zip) |
|
|
|
|
|
|
9.Certifying Doctor's Name and License Type
10.Certifying Doctor's License Number and Jurisdiction
11.Certifying Doctor’s Phone and Fax Numbers
(Ph)(Fax)
12.Certifying Doctor’s Address (Street or PO Box, City State Zip)
II. DOCTOR’S ROLE
13.Indicate which role you are serving in the claim in performing this evaluation. Only a doctor serving in one of the following roles is authorized to evaluate MMI/impairment and file this report [28 Texas Administrative Code (TAC) §130.1 governs such authorization]:
Treating Doctor |
Doctor selected by Treating Doctor acting in place of the Treating Doctor |
Designated Doctor selected by DWC |

 Insurance
Insurance
III. MEDICAL STATUS INFORMATION
14. Date of Exam |
15. Diagnosis Codes |
____ / ____ / ________ |
|
16. Indicate whether the |
employee has reached Clinical or Statutory MMI based upon the following definitions: |
Clinical Maximum Medical Improvement (Clinical MMI) is the earliest date after which, based upon reasonable medical probability, further material recovery from or lasting improvement to an injury can no longer reasonably be anticipated.
Statutory MMI is the later of: (1) the end of the 104th week after the date that temporary income benefits (TIBs) began to accrue; or
(2)the date to which MMI was extended by DWC pursuant to Texas Labor Code §408.104.
a) Yes, I certify that the employee reached
Yes, I certify that the employee reached  STATUTORY /
STATUTORY /  CLINICAL (mark one) MMI on ____ / ____ / ________
CLINICAL (mark one) MMI on ____ / ____ / ________
(may not be a prospective date) and have included documentation relating to this certification in the attached narrative. - OR -
b) No, I certify that the employee has NOT reached MMI but is expected to reach MMI on or about ____ / ____ / ________
No, I certify that the employee has NOT reached MMI but is expected to reach MMI on or about ____ / ____ / ________
The reason the employee has not reached MMI is documented in the attached narrative.
NOTE: The fact that an employee reaches either Clinical MMI or Statutory MMI does not signify that the employee is no longer entitled to medical benefits.
IV. PERMANENT IMPAIRMENT
17. If the employee has reached MMI, indicate whether the employee has permanent impairment as a result of the compensable injury.
“Impairment” means any anatomic or functional abnormality or loss existing after MMI that results from a compensable injury and is reasonably presumed to be permanent. The finding that impairment exists must be made based upon objective clinical or laboratory findings meaning a medical finding of impairment resulting from a compensable injury, based upon competent objective medical evidence that is independently confirmable by a doctor, including a designated doctor, without reliance on the subjective symptoms perceived by the employee.
a) I certify that the employee does not have any permanent impairment as a result of the compensable injury. - OR -
I certify that the employee does not have any permanent impairment as a result of the compensable injury. - OR -
b) I certify that the employee has permanent impairment as a result of the compensable injury. The amount of permanent impairment is _____%, which was determined in accordance with the requirements of the Texas Labor Code and Texas Administrative Code. The attached narrative provides explanation and documentation used for the calculation of the impairment rating assigned using the appropriate tables, figures, or worksheets from the following
I certify that the employee has permanent impairment as a result of the compensable injury. The amount of permanent impairment is _____%, which was determined in accordance with the requirements of the Texas Labor Code and Texas Administrative Code. The attached narrative provides explanation and documentation used for the calculation of the impairment rating assigned using the appropriate tables, figures, or worksheets from the following
edition of the Guides to the Evaluation of Permanent Impairment published by the American Medical Association (AMA): 
 third edition, second printing, February 1989 - OR -
third edition, second printing, February 1989 - OR -

 fourth edition, 1st, 2nd, 3rd, or 4th printing, including corrections and changes issued by the AMA prior to May 16, 2000.
fourth edition, 1st, 2nd, 3rd, or 4th printing, including corrections and changes issued by the AMA prior to May 16, 2000.
NOTE: A finding of no impairment is not equivalent to a 0% impairment rating. A doctor can only assign an impairment rating, including a 0% rating, if the doctor performed the examination and testing required by the AMA Guides.
V. DOCTOR’S CERTIFICATION
18.I HEREBY CERTIFY THAT THIS REPORT OF MEDICAL EVALUATION is complete and accurate and complies with the Texas Labor Code and applicable rules. If an impairment rating has been assigned, I certify that I have completed the required training and testing and have a current certification by DWC to assign impairment ratings in the Texas workers' compensation system or have received specific permission by DWC to certify MMI and assign an impairment rating. I understand that making a misrepresentation about a workers’ compensation claim or myself is a crime that can result in fines and/or imprisonment and nullification of this report.
|
Signature of Certifying Doctor: _________________________________________________ |
Date of Certification: __________________ |
|||
|
VI. TREATING DOCTOR’S AGREEMENT OR DISAGREEMENT WITH ANOTHER DOCTOR’S CERTIFICATION |
||||
19. |
Treating Doctor's Name and License Type |
22. |
|
||
|
|
|
|
I AGREE / I DISAGREE with the certifying doctor’s certification of MMI. |
|
20. |
Treating Doctor's License Number and Jurisdiction |
|
23. |
|
|
|
|
|
|
I AGREE / I DISAGREE with the certifying doctor’s finding of no impairment. - OR - |
|
21. |
Treating Doctor’s Phone and Fax Numbers |
|
I AGREE / I DISAGREE with the impairment rating assigned by the certifying doctor. |
||
(Ph) |
(Fax) |
|
|
||
24.I understand that making a misrepresentation about a workers’ compensation claim is a crime that can result in fines and/or imprisonment.
Signature of Treating Doctor: __________________________________________________ |
Date: _____________________________ |
DWC069 Rev. 01/15 |
Page 1 of 3 |
DWC069
Frequently Asked Questions
Report of Medical Evaluation (DWC
INSTRUCTIONS FOR DOCTORS:
Who can file the DWC
Treating Doctor: Doctor chosen by the employee who is primarily responsible for employee's
Doctor Selected by Treating Doctor: Doctor selected by the treating doctor to evaluate permanent impairment and Maximum Medical Improvement (MMI). This doctor acts in the place of the treating doctor. Such a doctor must be selected if the treating doctor is not authorized to certify MMI or assign an impairment rating in those cases in which the employee has permanent impairment. An authorized treating doctor may also choose to select another doctor to perform the evaluation/certification.
Designated Doctor: Doctor selected by the Texas Department of Insurance, Division of Workers’ Compensation (DWC) to resolve a question over MMI or permanent impairment.
Insurance
AUTHORIZATION: In addition to the requirement of acting in an eligible role, 28 Texas Administrative Code §130.1 provides the following requirements:
Employee has permanent impairment: Only a doctor certified by DWC to assign impairment ratings or who receives specific
permission by exception granted by DWC is authorized to certify MMI and to assign an impairment rating.
Employee does not have permanent impairment: A doctor not certified or exempted from certification by DWC is only authorized to determine whether an employee has permanent impairment and, in the event that the employee has no impairment, certify MMI.
INVALID CERTIFICATION: Certification by a doctor who is not authorized is invalid.
Under what circumstances and when am I required to file the DWC
If the employee has reached MMI, you must file the DWC
Where do I file the form?
The DWC
the insurance carrier;
the treating doctor (if a doctor other than the treating doctor files the report);
DWC;
injured employee; and
injured employee’s representative (if any).
The report must be filed by facsimile or electronic transmission unless an exception applies. The specific requirements are shown below. To file this form with DWC, fax to (512)
|
|
Insurance Carrier |
|
Treating Doctor |
|
|
|
DWC |
|
|
|
|
|
|
Designated Doctor |
fax or |
fax or |
||
|
|
|
|
|
Treating Doctor |
|
|
|
fax or |
Doctor Selected by Treating Doctor |
|
fax or |
not provided these numbers; then |
|
Insurance |
|
|
|
by other verifiable means |
Injured Employee
Injured Employee’s Representative
fax or
fax or
Do I have to maintain documentation regarding the examination and report?
The certifying doctor must maintain the original copy of the report and narrative and documentation of the following:
date of the examination;
date any medical records necessary to make the certification of MMI were received, and from whom the medical records were received; and
date, addresses, and means of delivery that required reports were transmitted or mailed by the certifying doctor.
Where can I find more information about the Report of Medical Evaluation?
See 28 TAC §130.1 through §130.4 and §130.6 for the complete requirements regarding the filing of this report, including required documentation. The complete text of these rules is available on the Texas Department of Insurance website at www.tdi.texas.gov/wc/rules/index.html. If you have additional questions, call
DWC069 Rev. 01/15 |
Page 2 of 3 |
DWC069
IMPORTANT INFORMATION FOR INJURED EMPLOYEES:
What if I disagree with the doctor's certification of Maximum Medical Improvement (MMI) and/or permanent impairment rating for my workers' compensation claim?
If this is the first evaluation of your MMI and/or permanent impairment, you or your representative may dispute:
the certification of MMI; and/or
the assigned impairment rating.
To file the dispute, contact your local DWC field office or call
the appointment of a designated doctor (DD), if one has not been appointed; or
a Benefit Review Conference (BRC).
Important Note: Your dispute must be filed within 90 days after the written notice is delivered to you or the certification of MMI and/or the assigned impairment rating may become final.
NOTE: With few exceptions, upon your request, you are entitled to be informed about the information DWC collects about you; receive and review the information (Government Code, §§552.021 and 552.023); and have DWC correct information that is incorrect (Government Code, §559.004).
DWC069 Rev. 01/15 |
Page 3 of 3 |
Form Data
| Fact | Detail |
|---|---|
| Form Name | Report of Medical Evaluation (DWC Form-069) |
| Issued By | Texas Department of Insurance, Division of Workers’ Compensation |
| Purpose | To report Maximum Medical Improvement (MMI) and/or Permanent Impairment |
| Who Can File | Treating Doctor, Doctor selected by Treating Doctor, Designated Doctor, Insurance Carrier-Selected RME Doctor |
| Governing Law(s) | 28 Texas Administrative Code §130.1, Texas Labor Code §408.104 |
| Filing Deadline | Within 7 working days after the certifying examination or receipt of all medical information necessary to certify MMI |
Instructions on Utilizing Texas Dwc069
Filling out the Texas DWC069 form is a critical step in the process of reporting medical evaluations related to workers' compensation claims. This form serves as an official document that captures important information about an employee's medical status, including details about any permanent impairments as a result of a workplace injury. The information provided through this form helps in making important determinations regarding the injured employee's workers' compensation benefits. Here are the step-by-step instructions to accurately complete the Texas DWC069 form:
- Begin with General Information. Fill in the required fields including the Workers’ Compensation Insurance Carrier, Employer’s Name, and Employer’s Address. These details are crucial for identifying the correct insurance policy covering the employee.
- Enter the Injured Employee's Name, Date of Injury, and Social Security Number. Ensure these details are accurate to avoid any issues with processing the claim.
- Provide the Employee's Phone Number and Address. This information is necessary for any follow-up communication.
- Under the Certifying Doctor's Information, include the Doctor's Name, License Type, License Number, Jurisdiction, Phone and Fax Numbers, and Address. This section is vital for verifying the credentials of the examining doctor.
- In the section labeled Doctor’s Role, mark the specific role you are serving in this claim. This helps clarify the capacity in which the medical evaluation is being conducted.
- Fill in the Date of Exam and Diagnosis Codes in the Medical Status Information section. This part provides insight into the medical evaluation date and the diagnosed conditions.
- Indicate whether the employee has reached either Clinical or Statutory MMI (Maximum Medical Improvement) and provide the date on which MMI was reached or is expected to be reached. Attach any narrative documentation supporting this certification.
- If the employee has reached MMI, indicate whether they have a permanent impairment as a result of the injury. Specify the percentage of permanent impairment, if applicable, and include any documentation used in determining this figure.
- Under Doctor’s Certification, the certifying doctor must sign and date the form, thereby certifying that the report is complete, accurate, and complies with relevant laws and rules.
- If another doctor, particularly the treating doctor, is involved, they must agree or disagree with the certifying doctor’s certification of MMI and the finding of impairment. They should provide their name, license information, and signature under Treating Doctor's Agreement or Disagreement.
Once all sections of the form are accurately filled out, ensure that the document, along with any necessary narratives or documentation, is submitted to the appropriate parties as outlined in the instructions. This includes the insurance carrier, DWC, the treating doctor (if different from the certifying doctor), the injured employee, and their representative (if applicable). Proper and timely submission of this form is essential in facilitating the workers' compensation process.
Obtain Answers on Texas Dwc069
Who can file the DWC Form-069?
The DWC Form-069 can be filed by various types of doctors involved in a workers’ compensation claim in Texas. These include the treating doctor who is primarily responsible for the employee's injury-related healthcare, a doctor selected by the treating doctor to evaluate permanent impairment and Maximum Medical Improvement (MMI), a designated doctor selected by the Texas Department of Insurance, Division of Workers’ Compensation (DWC) to resolve questions over MMI or permanent impairment, and an insurance carrier-selected RME Doctor approved specifically by DWC.
What are the authorization requirements for filing the DWC Form-069?
Doctors must meet certain requirements to be authorized to file the DWC Form-069. If the employee has permanent impairment, a doctor needs to be certified by DWC to assign impairment ratings or receive specific permission from DWC. If the employee does not have permanent impairment, a doctor not certified or exempted by DWC can certify MMI but only to determine the absence of permanent impairment.
When is a doctor required to file the DWC Form-069?
This form must be filed no later than the seventh working day after the later of the date of the certifying examination or receipt of all medical information necessary to certify MMI. This requirement specifically applies to a Designated Doctor if the employee has not reached MMI.
Where should the DWC Form-069 be filed?
The form and required narrative must be filed with the insurance carrier, the treating doctor (if relevant), DWC, the injured employee, and the employee’s representative, if any. Filing should be done via fax or electronic transmission, where feasible, using provided contacts or by other verifiable means if not.
Is a doctor required to maintain documentation related to the DWC Form-069?
Yes, the certifying doctor must keep the original report and narrative, including documentation of the examination date, when necessary medical records were received and from whom, and the dates, addresses, and means of delivery for the transmission or mailing of required reports.
Where can more information about the Report of Medical Evaluation be found?
Details about filing this report, including required documentation, can be found in sections 28 TAC §130.1 through §130.4 and §130.6 on the Texas Department of Insurance website. For additional questions, doctors can call a specific hotline.
What if an injured employee disagrees with the doctor's certification of MMI or the impairment rating?
If there's disagreement with the certification of MMI or the assigned impairment rating, the injured employee or their representative can dispute these assessments. They may contact their local DWC field office or call a dedicated number to request the appointment of a designated doctor or a Benefit Review Conference (BRC). It's crucial that disputes be filed within 90 days from when the written notice is delivered, or the certification and rating may become final.
What happens if a certification by a doctor is invalid?
Certifications made by doctors who are not authorized are considered invalid. It's important for doctors to ensure they meet the specific authorization requirements set by 28 Texas Administrative Code §130.1 to avoid invalid certifications.
Are employees entitled to access information collected by DWC about them?
Yes, with few exceptions, employees have the right to be informed about, receive and review the information DWC collects about them. They also have the right to have DWC correct any information that is incorrect, as per the Government Code, §§552.021, 552.023, and §559.004.
Common mistakes
Failing to complete all required fields: Individuals often overlook or intentionally leave blank certain parts of the form, such as the DWC Claim # or the Carrier Claim #. Every section that applies should be filled out to ensure the form is processed efficiently.
Incorrect or incomplete doctor information: The sections asking for the certifying doctor's name, license type, and contact information is crucial. If this information is not accurately provided, it could lead to delays or the outright rejection of the form. Specifically, filling out sections 9 to 12 requires attention to detail.
Misunderstanding the doctor’s role: Section 13 requires the doctor to indicate their role in the evaluation process. Mistakes are made when the wrong role is selected or when this section is left blank, signifying a lack of understanding of the doctor's proper role in the claim’s evaluation.
Incorrect MMI and permanent impairment details: Sections 16 and 17 are often incorrectly completed. The distinction between Clinical and Statutory MMI is crucial, as is accurately reporting whether the employee has any permanent impairment. Providing incorrect information or misinterpreting the terms can significantly impact the outcome for the employee.
Failure to include required attachments: The certification of MMI or impairment often needs to be accompanied by supporting documentation, as outlined in the attached narrative requirement. When this documentation is not attached, or if the narrative does not adequately explain the reasoning behind the MMI date or impairment rating, the form may not be considered valid.
Incorrect or missing doctor’s certification: The final section, Doctor’s Certification, is sometimes overlooked. The certifying doctor must sign and date the form, certifying the accuracy and completeness of the information. Failure to do so invalidates the entire form, as it lacks the official confirmation of the evaluating doctor’s findings.
In summary, individuals completing the Texas DWC069 form must be thorough, ensuring all sections are accurately filled out and that supporting documentation is attached. Understanding the specific requirements for each section and double-checking the information provided can help avoid these common mistakes.
Documents used along the form
When dealing with the aftermath of a work-related injury in Texas, the Texas Department of Insurance Division of Workers’ Compensation (DWC) requires various forms and documents to ensure the injured worker gets the proper care and compensation they are entitled to. One such document is the Texas DWC069 form, essential for reporting medical evaluations related to a workers' compensation claim. However, completing the DWC069 form is often just one step in a series of necessary actions. There are several other crucial documents that typically accompany or follow the filing of a DWC069 form, each serving a unique purpose in the workers' compensation process.
- DWC003 Employer’s Wage Statement: Provides information on the injured employee's earnings, which helps in calculating the rate of temporary or permanent income benefits.
- DWC045 Employer’s First Report of Injury or Illness: Filed by the employer to officially report an employee's work-related injury or illness to the insurance carrier and DWC.
- DWC032 Request for Paid Leave: Used by the injured employee to request the use of sick leave, vacation time, or other paid leave to cover time off due to a work-related injury.
- DWC041 Employee’s Claim for Compensation: Filed by the injured employee to officially claim workers’ compensation benefits for an injury or illness.
- DWC025 Request to Change Treating Doctor: Used by the injured worker to request a change of their current treating doctor to another doctor within the workers’ compensation network.
- DWC063 Work Status Report: Provides details about the injured employee's work capabilities, restrictions, and expected duration of the recovery period, filled out by the treating doctor.
- DWC022 Agreement to Compensate with Temporary Income Benefits: An agreement document between the employer or insurance carrier and the injured employee regarding the compensation of temporary income benefits.
- DWC024 Supplemental Report of Injury: Filed by the employer to update or provide additional information after the initial report of injury or illness.
- DWC056 Employee’s Request for a Designated Doctor Examination: Used by the employee to request an examination by a designated doctor to resolve disputes about the medical condition or impairment rating.
These documents play vital roles in the administration and resolution of workers' compensation claims in Texas. Each one contributes specific information or decisions required for processing a claim, managing benefits, or addressing disputes regarding an employee's injury or illness. Understanding the purpose of each form and when it needs to be filed can simplify navigating the often complex workers' compensation system, ensuring both the injured worker and the employer fulfill their respective obligations under Texas law.
Similar forms
The First Report of Injury (FROI) form is another document within the workers' compensation system that bears resemblance to the Texas DWC069 form. Much like the DWC069, which is used for reporting medical evaluations, the FROI is utilized to initially report the occurrence of a workplace injury to the relevant state department or workers' compensation board. Both forms are critical in the documentation and management of workers' compensation claims, though they serve different stages in the claim process. The FROI marks the beginning, while the DWC069 often comes into play when determining the extent of injury and any permanent impairment.
The Request for Paid Leave (RPL) form, while not directly related to workers' compensation, shares similarities with the DWC069 in the context of documenting conditions that may affect an employee’s ability to work. The RPL form is typically used within organizations to formally request time off due to medical reasons, much like how the DWC069 is used to document medical evaluations related to workplace injuries. Both are instrumental in providing official documentation for absence from work and potential benefits eligibility.
Worker's Compensation Claim Form is closely related to the DWC069. This form is the initial step for employees to notify their employer and the insurance carrier about a workplace injury or illness, seeking workers’ compensation benefits. Like the DWC069, which provides detailed medical evaluation information about the injury's impact and permanent impairment, the claim form initiates the process these evaluations eventually contribute to. Both documents are pivotal in the workers' compensation system, facilitating the assessment and compensation for workplace injuries.
The Maximum Medical Improvement (MMI) and Impairment Rating Report, similar to sections within the DWC069, is explicitly designed to document an injured worker’s recovery status and any permanent impairment. The DWC069 form, through its medical evaluation report, accomplishes a similar purpose by documenting when an employee reaches MMI and the percentage of permanent impairment, if any, using the AMA Guides. Both documents are fundamental in determining the compensation and benefits an injured worker is entitled to under workers' compensation laws.
Employee's Claim for Workers' Compensation Benefits form is an essential step for workers who have sustained injuries on the job and are seeking compensation. This form and the DWC069 serve complementary roles in the claim process. While the employee's claim form initiates the claim by outlining the injury and the request for benefits, the DWC069 provides the medical basis for those claims, detailing the medical evaluation, MMI, and any impairment rating.
The Permanent Partial Disability (PPD) Award Agreement form, which outlines the compensation agreement for an employee who has sustained a permanent partial disability due to a workplace injury, parallels the DWC069 in its focus on long-term impact assessments. While the DWC069 provides a medical evaluation that may conclude with a permanent impairment rating, the PPD Award Agreement uses this information to formalize the compensation terms for the impairment, underscoring the financial aspect of the injury's outcome.
Dos and Don'ts
Filling out legal documents can be a daunting task, but it's crucial to approach them with attention to detail and accuracy. The Texas DWC069 form is a significant document within the realm of workers' compensation, and properly completing it ensures a smoother process for all parties involved. This guide highlights the do's and don'ts when handling this specific form.
Do:Verify authorization: Ensure that the doctor completing the form is authorized under the 28 Texas Administrative Code §130.1. This is crucial as the form will be invalid if filled out by an unauthorized practitioner.
Include all necessary information: Fill in every section of the form with accurate and up-to-date information. Missing or incorrect information can lead to unnecessary delays or the outright rejection of the form.
Submit in a timely manner: Adhere to the submission deadlines. The form must be filed no later than the seventh working day after the employee has reached Maximum Medical Improvement (MMI) or after all medical information necessary to certify MMI has been received.
Maintain documentation: The certifying doctor should keep the original copy of the report and narrative, along with documentation of the examination date, the dates any necessary medical records were received, and the means and dates of transmission to the required parties.
Assume eligibility: Not every doctor is eligible to fill this form. Before proceeding, confirm that the doctor is either a treating doctor, selected by the treating doctor, a designated doctor, or an insurance carrier-selected RME doctor, and specifically authorized by DWC.
Overlook companion documentation: The DWC069 form often requires additional narratives or documentation to support the findings. Failing to attach these supplemental documents can result in the form being considered incomplete.
Forget to file with all parties: This form must be shared with the insurance carrier, the treating doctor (if another doctor fills out the report), DWC, the injured employee, and their representative if they have one. Missing any of these filings can lead to complications.
Use non-verified communication methods: Unless an exception applies, the report must be filed either by facsimile or electronic transmission. Using unverified or prohibited methods of communication can lead to processing delays.
While navigating the complexities of workers' compensation documentation, remember that accuracy, timeliness, and following the specific guidelines set forth by the Texas Department of Insurance, Division of Workers’ Compensation, are key to a successful and efficient filing process.
Misconceptions
Understanding the Texas DWC069 form is crucial for injured employees navigating the workers' compensation system. However, there are several misconceptions about this form and its implications. Here are ten common misunderstandings and clarifications to help demystify the process:
- Misconception 1: The DWC069 form is the only document required for processing a workers' compensation claim.
Clarification: This form, which reports on Maximum Medical Improvement (MMI) and impairment rating, is indeed important but is just one aspect of a comprehensive process that includes claims forms, medical records, and possibly other documentation for a complete evaluation.
- Misconception 2: Any doctor can complete and sign the DWC069 form.
Clarification: Only doctors authorized by the Division of Workers' Compensation (DWC) or those specifically given permission to certify MMI and assign an impairment rating are eligible to complete this form.
- Misconception 3: Filing a DWC069 form means an employee will no longer receive medical benefits.
Clarification: Reaching MMI does not signify the end of medical benefits. It simply means that from a medical standpoint, no significant improvement or recovery from the injury is anticipated, but necessary treatment may continue.
- Misconception 4: The impairment rating given is subjective and open to interpretation.
Clarification: Impairment ratings are determined based on objective clinical or laboratory findings and must be calculated using the American Medical Association (AMA) Guides to the Evaluation of Permanent Impairment.
- Misconception 5: Once MMI is certified, the impairment rating is final and cannot be disputed.
Clarification: If an employee disagrees with the certified MMI or impairment rating, they have the right to dispute the findings and seek a re-evaluation from a designated doctor or request a Benefit Review Conference (BRC).
- Misconception 6: The DWC069 form must be filed with the DWC only.
Clarification: This form, along with the required narrative, should be filed with the insurance carrier, the treating doctor (if different from the one filing the report), the DWC, the injured employee, and the employee’s representative if applicable.
- Misconception 7: Any doctor evaluating an employee for MMI or impairment can select themselves as the treating doctor on the DWC069 form.
Clarification: Only the treating doctor, a doctor elected by the treating doctor, or a DWC-appointed designated doctor can evaluate and certify MMI and permanent impairment.
- Misconception 8: The DWC069 form is a mandatory submission for all workplace injuries.
Clarification: This form is necessary only when an employee is deemed to have reached MMI and there is a determination of permanent impairment to be documented.
- Misconception 9: Filing the DWC069 form is the responsibility of the employee.
Clarification: It is the responsibility of the certifying doctor to complete and file this form appropriately within the mandated timeframe, ensuring all pertinent parties receive copies.
- Misconception 10: A finding of no impairment is equivalent to a 0% impairment rating.
Clarification: A determination of no impairment indicates that no permanent anatomical or functional abnormalities or losses have been identified post-MMI. However, a 0% impairment rating can be assigned and indicates that despite identifying such impairments, they do not result in any impairment according to the AMA Guides.
Clearing up these misconceptions is essential for accurately navigating the complex landscape of workers' compensation claims in Texas. Both employees and employers benefit from understanding the specifics of the DWC069 form and the broader claims process.
Key takeaways
Filling out and utilizing the Texas DWC069 form, officially known as the Report of Medical Evaluation, is pivotal in the workers' compensation process. This document plays a crucial role in determining the extent of an employee's injury, the compensation, and the benefits they are entitled to. Here are six key takeaways to understand when dealing with this form:
- The DWC069 form is used to report the Maximum Medical Improvement (MMI) and Permanent Impairment (if any) of an injured worker. These determinations are essential in concluding the amount of benefits an injured worker can receive.
- Only certain medical professionals are authorized to complete this form, including the treating doctor, a doctor selected by the treating doctor, a designated doctor selected by the Division of Workers’ Compensation (DWC), or an insurance carrier-selected Required Medical Examination (RME) doctor, provided they have received specific approval by DWC.
- It's imperative to note that the certification by a doctor who isn't authorized by the appropriate section of the Texas Administrative Code (28 TAC §130.1) is considered invalid, highlighting the need for strict adherence to the guidelines.
- The form must be filed no later than the seventh working day after the certifying examination or after receiving all necessary medical information to certify MMI. This timely filing is critical for the processing of a worker's compensation claim.
- All filed DWC069 forms along with the required narrative should be submitted to multiple parties, including the insurance carrier, the treating doctor (if the report is filed by a doctor other than the treating doctor), DWC, the injured employee, and any representative of the injured employee. This ensures all involved parties are informed.
- If an injured worker disagrees with the MMI and/or permanent impairment rating determined, they have the right to dispute these findings. They must file their dispute within 90 days after notice of the certification has been provided to them to avoid the certification becoming final.
Understanding and accurately completing the DWC069 form is crucial for both the injured employee's rights and the obligations of the treating medical professional. Ensuring compliance with the detailed requirements set forth by the Texas Department of Insurance, Division of Workers' Compensation, is necessary for the smooth execution of workers' compensation claims and disputes.
Popular PDF Forms
Va Form 26 1880 - Upon approval, the Certificate of Eligibility issued will outline the applicant’s entitlement amount and conditions.
What Is an S-8 - Special sections of Form F8 address additional expenses, like child care or educational costs, which can impact support calculations.