Blank Treatment Plan PDF Template
The essence of a Treatment Plan form lies in its comprehensive approach to mapping out a course of action tailored to an individual's health needs, particularly in the realm of mental health. It isn't just a piece of paper; it represents a mutually agreed-upon route between a patient and their therapist towards achieving specific, beneficial changes. These changes are articulated through well-defined goals that are objective and measurable, ensuring clarity in the path to recovery. To facilitate a holistic approach, these plans include estimated timeframes for goal completion, bridging the gap between aspirations and reality. Central to the treatment plan is the patient's involvement—it is developed collaboratively, ensuring the patient's consent and commitment, symbolized by their signature. The document outlines a variety of treatment goals, such as reducing risk factors or symptoms, enhancing coping strategies, and maintaining symptom stabilization over the long term. Furthermore, it specifies planned interventions that range from assertiveness training and problem-solving skills to medication referral, all aligned with the treatment goals. Critical to its functionality is the education provided to the patient about their diagnosis, ensuring they are fully informed and actively participate in their treatment. In essence, the Treatment Plan form serves as a tactical roadmap designed to empower individuals on their journey to improved mental health, underscored by the collaboration between patient and therapist.
Preview - Treatment Plan Form
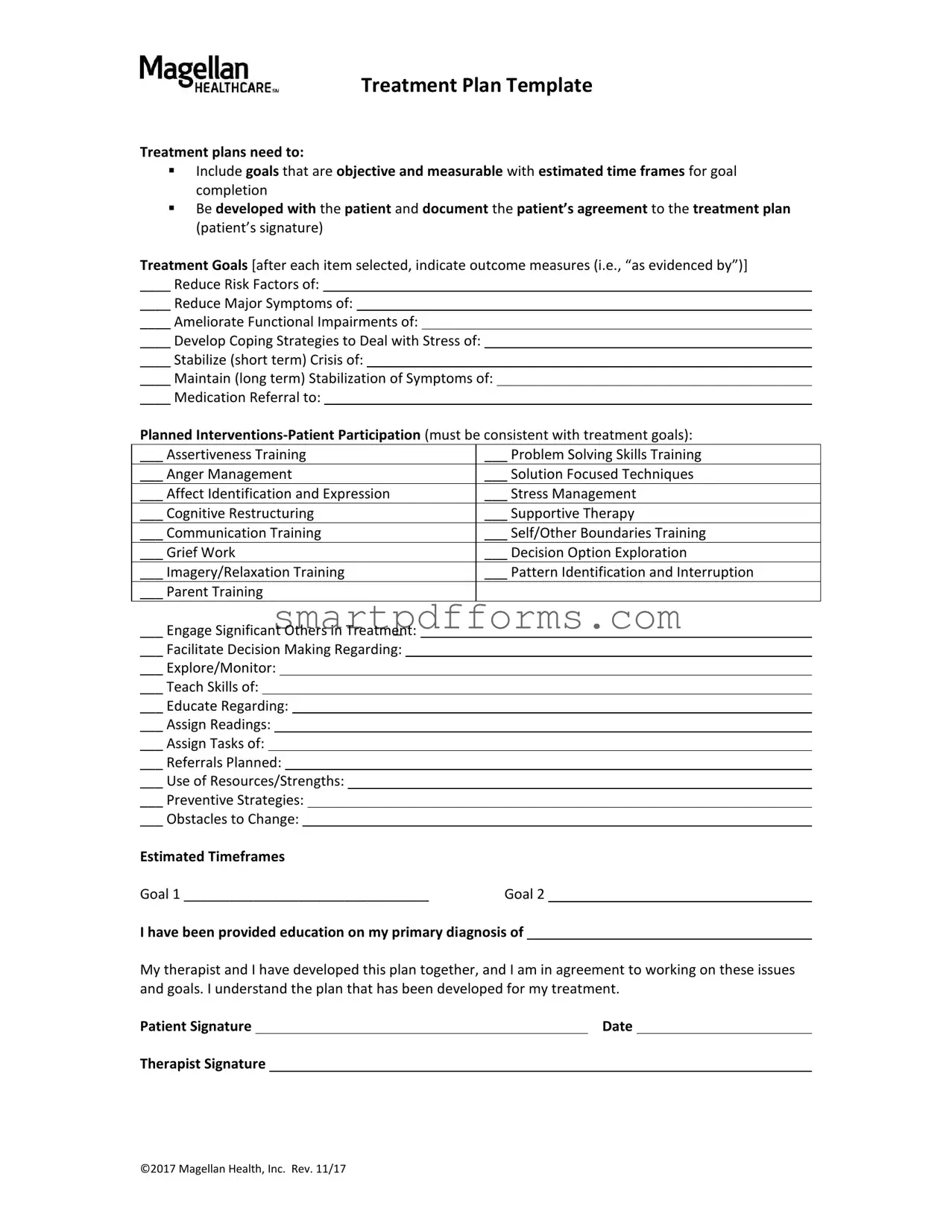
Treatment Plan Template
Treatment plans need to:
▪Include goals that are objective and measurable with estimated time frames for goal completion
▪Be developed with the patient and document the patient’s agreement to the treatment plan (patient’s signature)
Treatment Goals [after each item selected, indicate outcome measures (i.e., “as evidenced by”)]
____ Reduce Risk Factors of:
____ Reduce Major Symptoms of:
____ Ameliorate Functional Impairments of:
____ Develop Coping Strategies to Deal with Stress of:
____ Stabilize (short term) Crisis of:
____ Maintain (long term) Stabilization of Symptoms of:
____ Medication Referral to:
Planned
___ Assertiveness Training |
___ Problem Solving Skills Training |
|||||||||||||
___ Anger Management |
___ Solution Focused Techniques |
|||||||||||||
___ Affect Identification and Expression |
___ Stress Management |
|||||||||||||
___ Cognitive Restructuring |
___ Supportive Therapy |
|||||||||||||
___ Communication Training |
___ Self/Other Boundaries Training |
|||||||||||||
___ Grief Work |
___ Decision Option Exploration |
|||||||||||||
___ Imagery/Relaxation Training |
___ Pattern Identification and Interruption |
|||||||||||||
___ Parent Training |
|
|
|
|||||||||||
___ Engage Significant Others in Treatment: |
|
|
|
|
||||||||||
___ Facilitate Decision Making Regarding: |
|
|
|
|
||||||||||
___ Explore/Monitor: |
|
|
|
|
||||||||||
___ Teach Skills of: |
|
|
|
|
||||||||||
___ Educate Regarding: |
|
|
|
|
||||||||||
___ Assign Readings: |
|
|
|
|
||||||||||
___ Assign Tasks of: |
|
|
|
|
||||||||||
___ Referrals Planned: |
|
|
|
|
||||||||||
___ Use of Resources/Strengths: |
|
|
|
|
||||||||||
___ Preventive Strategies: |
|
|
|
|
||||||||||
___ Obstacles to Change: |
|
|
|
|
||||||||||
Estimated Timeframes |
|
|
|
|||||||||||
Goal 1 ________________________________ |
Goal 2 |
|
|
|||||||||||
I have been provided education on my primary diagnosis of
My therapist and I have developed this plan together, and I am in agreement to working on these issues and goals. I understand the plan that has been developed for my treatment.
Patient Signature |
|
Date |
Therapist Signature
©2017 Magellan Health, Inc. Rev. 11/17
Form Data
| Fact Number | Fact Detail |
|---|---|
| 1 | Treatment plans are designed to include goals that are objective and measurable, incorporating estimated time frames for the completion of these goals. |
| 2 | Development of the treatment plan is a collaborative process involving both the patient and the therapist, ensuring the patient's agreement is documented through their signature. |
| 3 | The template specifies the need to reduce risk factors, major symptoms, and functional impairments, alongside developing coping strategies and maintaining symptom stabilization. |
| 4 | It outlines planned interventions that require patient participation, which should align with the established treatment goals. |
| 5 | Interventions include a wide array of therapeutic techniques and training such as assertiveness training, problem solving skills, anger management, and more, aimed at addressing specific patient needs. |
| 6 | The template prompts for the inclusion of medication referral if necessary, indicating a comprehensive approach to treatment. |
| 7 | It also provides sections for engaging significant others in the treatment process, exploring and monitoring specific issues, and facilitating decision making. |
| 8 | There are parts of the plan dedicated to educating the patient, assigning readings and tasks, and making external referrals, underlining the importance of an educative approach in treatment. |
| 9 | The document concludes with a section for patient and therapist signatures, emphasizing mutual understanding and agreement on the treatment plan devised. |
Instructions on Utilizing Treatment Plan
After deciding on a treatment strategy, it's crucial to detail the approach in a structured manner, ensuring clear objectives and methods are communicated between the patient and their healthcare provider. Filling out the Treatment Plan form is a methodical way to document these vital pieces of information. It not only outlines the targeted goals and planned interventions but also incorporates both the healthcare provider and the patient's commitment to the proposed treatment strategy. Here are steps to guide you through accurately completing the Treatment Plan form.
- Review the Treatment Plan Template: Begin by familiarizing yourself with the entire form to understand the information required.
- Identify Treatment Goals: Discuss with the patient and decide on specific, measurable goals. After each goal selected, specify the outcome measures by completing the section "as evidenced by".
- Document Goals Related to:
- Reducing risk factors
- Reducing major symptoms
- Ameliorating functional impairments
- Developing coping strategies for stress
- Stabilizing crisis (short term)
- Maintaining stabilization of symptoms (long term)
- Select Planned Interventions—Patient Participation: Choose interventions that align with the treatment goals. These should be activities the patient will actively participate in, such as Assertiveness Training, Anger Management, Stress Management, etc.
- Specify Planned Interventions: Fill in the planned interventions more specifically under each category, ensuring they directly relate to achieving the outlined treatment goals.
- Include Medication and Referrals: If medication is part of the treatment plan, include this information. Additionally, document any referrals to specialists or other healthcare providers.
- Plan Use of Resources/Strengths and Preventive Strategies: Outline any resources or strengths of the patient that will be utilized, along with strategies for preventing relapse or worsening of conditions.
- Note Obstacles to Change: Acknowledge any potential barriers that could impede progress towards the treatment goals.
- Estimate Timeframes for Each Goal: For every goal listed, provide an estimated timeframe for achieving it.
- Document Education and Agreement: Confirm that the patient has been educated about their primary diagnosis and document the patient's agreement to the treatment plan by having them sign the form.
- Include Therapist and Patient Signatures: Ensure both the therapist and the patient sign the form, validating the mutual agreement to undertake the treatment plan.
Completing the Treatment Plan form with careful attention to detail is crucial for a successful therapy outcome. It acts as a roadmap for both the patient and therapist, outlining clear goals, interventions, and timelines. Ensuring that both parties are informed and in agreement with the treatment plan fosters a collaborative environment conducive to healing and recovery.
Obtain Answers on Treatment Plan
-
What is a Treatment Plan form?
A Treatment Plan form is a document developed in collaboration between a patient and their therapist, detailing the objectives and goals of therapy. It outlines specific, measurable goals with estimated timeframes for achievement and includes interventions and patient participation activities consistent with these aims. It also documents the patient's agreement to the treatment through their signature.
-
Why is it necessary for goals to be objective and measurable?
Setting goals that are objective and measurable enables both the therapist and the patient to track progress in a clear, tangible way. This facilitates adjustments to the therapy if needed and helps in maintaining focus on the desired outcomes, ensuring that both parties can see the improvements and work efficiently towards goal completion.
-
How are goals included in the Treatment Plan developed?
Goals are developed collaboratively between the patient and their therapist, focusing on reducing risks, alleviating symptoms, addressing functional impairments, developing coping strategies, and maintaining symptom stabilization, among other things. The process ensures that the goals are personalized, taking into consideration the patient’s unique needs and circumstances.
-
What does patient participation mean in the context of the Treatment Plan?
Patient participation refers to the active involvement of the patient in their treatment process. It includes their engagement in planned interventions, such as assertiveness training, problem-solving skills, stress management, and other therapeutic activities that support the achievement of the treatment goals.
-
Can the Treatment Plan be modified?
Yes, the Treatment Plan can be modified. Since therapy is a dynamic process, adjustments may be necessary as the therapy progresses, new issues emerge, or goals are achieved. Any modifications should be made in collaboration with the patient, ensuring their needs and perspectives continue to be central to the treatment approach.
-
What is the significance of the patient signing the Treatment Plan?
The patient’s signature on the Treatment Plan signifies their understanding and agreement to the proposed therapy goals and interventions. It is an important step that promotes a sense of ownership and commitment towards the therapeutic process and the achievement of personal goals.
-
What are estimated timeframes in a Treatment Plan?
Estimated timeframes refer to the tentative durations set for achieving each of the outlined goals in the Treatment Plan. These timeframes provide a rough timeline for therapy, offering both the therapist and the patient a schedule to work with while allowing for flexibility as required by the therapy’s progress.
-
How are the selected interventions related to the treatment goals?
Selected interventions are therapeutic activities and strategies that are directly aligned with achieving the specified treatment goals. They are chosen based on their relevance and efficacy in addressing the patient’s specific needs, symptoms, and objectives, ensuring a cohesive and targeted approach to treatment.
-
What role do obstacles to change play in the Treatment Plan?
Identifying obstacles to change within the Treatment Plan is crucial as it helps in foreseeing potential challenges that may hinder progress. Addressing these obstacles proactively allows for the development of strategies to overcome them, ensuring a smoother path towards achieving therapy goals.
-
Is patient education a part of the Treatment Plan?
Yes, patient education is an integral part of the Treatment Plan. It involves informing the patient about their primary diagnosis, the nature of their condition, and any relevant therapeutic techniques or concepts. Education empowers the patient by enhancing their understanding of the treatment process and fostering active engagement in their own therapy.
Common mistakes
Skipping goal-setting steps is a common mistake. It's crucial to list specific goals along with their measurable outcomes and estimated time frames for completion. Without clear objectives, it's difficult to track progress or know when the goals have been achieved.
Failing to involve the patient in the development of the treatment plan can undermine its effectiveness. The treatment plan should be a collaborative effort, capturing the patient’s agreement and signature to ensure their commitment and understanding.
Omitting outcome measures. After selecting treatment goals, it’s important to indicate how success will be measured (“as evidenced by”). This oversight can lead to ambiguity in assessing patient progress.
Not customizing the Planned Interventions-Patient Participation section to align with the established goals. Every selected intervention should directly support one or more of the patient’s goals to ensure a coherent treatment strategy.
Overlooking the patient’s strengths and available resources. Acknowledging these can empower the patient and make the treatment plan more attainable by leveraging existing supports.
Leaving the Estimated Timeframes for goals blank. Without a timeframe, it's challenging to maintain a sense of urgency and can lead to a lack of focus on achieving the goals.
Ignoring potential obstacles to change. It's important to preemptively address any foreseeable challenges that could impede progress, making the treatment plan more realistic and adaptable.
Forgetting to provide education on the patient’s primary diagnosis. Understanding their condition is crucial for patients to engage fully in their treatment plan and to empower them toward recovery.
Missing signatures. The patient and therapist’s signatures are vital, as they formalize the agreement and mutual commitment to the treatment plan. Without these, the document may not be considered valid or effective.
Documents used along the form
When caring for an individual's health, particularly in the mental health field, a Treatment Plan form is a cornerstone document that serves as a guide for both the patient and healthcare provider. However, this plan doesn't exist in isolation. Several other forms and documents often accompany it, each playing a vital role in ensuring a comprehensive and effective treatment process. Here's a look at some of these critical documents.
- Consent for Treatment Form: This document is crucial as it records the patient's agreement to receive treatment. It includes details about the nature of the treatment, possible risks, benefits, and alternative options. This informed consent ensures that the patient's autonomy and decision-making rights are respected.
- Initial Assessment Form: Before devising a treatment plan, a thorough initial assessment is necessary to understand the patient's current health status, medical history, and specific needs. This form captures all such relevant information, providing a foundation for tailored treatment strategies.
- Progress Notes: Throughout the treatment, healthcare providers maintain records of the patient's progress, any modifications to the plan, and observations during therapy sessions. These notes are essential for tracking the patient's journey, adjusting treatment as needed, and communicating with other care team members.
- Medication Management Forms: If medication is part of the treatment, these forms help in tracking the prescribed drugs, dosages, and schedules. They also monitor side effects and effectiveness of the medication, critical for assessing the treatment's impact and adjusting prescriptions when necessary.
- Release of Information Form: Treatment often involves collaboration between different healthcare professionals. This form allows for the sharing of relevant patient information among providers, ensuring a cohesive and comprehensive approach to care. It respects the patient's privacy by requiring their consent for information exchange.
In the realm of healthcare, especially within mental health services, paperwork might seem endless. Yet, each form and document has a distinct role in the treatment process. They collaborate to create a holistic framework that supports the patient's journey towards wellness. Understanding the function and importance of these documents enriches the treatment experience, ensuring both providers and patients are well-informed and actively engaged in the healing process.
Similar forms
Case Management Plan: Like the Treatment Plan, a Case Management Plan is tailored around the individual's needs and targets specific goals. Both types of plans require participation from the individual, set measurable objectives, and involve planning interventions aimed at reaching those objectives. They are collaborative efforts that should include the person's agreement and documented consent.
Care Plan for Chronic Conditions: This document outlines strategies and interventions for managing chronic health conditions. Similar to a Treatment Plan, it contains objectives that are objective and measurable, involves the person in the planning process, and focuses on both short-term stabilization and long-term maintenance of health, including medication management and lifestyle adjustments.
Behavior Intervention Plan: Designed to address specific behaviors and how to manage them, both this and a Treatment Plan establish clear, objective, and measurable goals. They engage the individual in developing coping strategies and interventions, like anger management or stress management, and require their agreement to the proposed strategies.
Individualized Education Program (IEP): Though focused on educational goals, an IEP is akin to a Treatment Plan in its structure and purpose. It sets forth measurable goals, involves the individual (and often their guardians), in the planning process, and outlines specific interventions or educational strategies tailored to the individual’s needs. Both require regular monitoring and adjustments as needed.
Personal Development Plan: This plan focuses on an individual's growth and development in various aspects of life, including career and personal skills. Similar to Treatment Plans, they establish objectives that are measurable, involve the person’s active participation and consent, and outline strategies and activities aimed at achieving these goals.
Substance Abuse Treatment Plan: Focused on individuals dealing with substance abuse, these plans resemble Treatment Plans in their approach to setting clear, attainable goals, involving the person in the development process, getting their agreement, and designing specific interventions to address substance use, coping strategies, and relapse prevention.
Mental Health Crisis Plan: Similar to a Treatment Plan in its aim to stabilize and provide interventions during a crisis, these plans include specific strategies for crisis management, measurable goals for recovery, and the individual's input and agreement on the course of action to be taken during mental health emergencies.
Rehabilitation Plan: Aimed at recovery from injury or illness, Rehabilitation Plans share similarities with Treatment Plans through the establishment of measurable and objective goals, the involvement of the individual in creating the plan, and documenting the individual’s consent to the outlined interventions which may include physical therapy, occupational therapy, or other targeted treatments.
Dos and Don'ts
When filling out the Treatment Plan form, there are specific practices to follow to ensure the document is both effective and compliant. It is crucial to pay attention to these guidelines to foster a constructive therapeutic relationship and encourage patient involvement in their treatment journey.
Do:- Involve the patient in the treatment planning process. This ensures their perspectives and preferences are incorporated, making them more likely to engage with the treatment.
- Set objective and measurable goals. This clarifies the expected outcomes and provides clear benchmarks for progress.
- Include estimated time frames for goal completion. Time frames establish a timeline for evaluation and adjustment of the treatment plan as necessary.
- Document the patient’s agreement to the treatment plan. This is typically done through the patient's signature, which shows their consent and commitment to the treatment process.
- Ensure goals and interventions are clearly linked. Every planned intervention should directly contribute to achieving one or more of the treatment goals.
- Regularly review and adjust the treatment plan. As the patient progresses or encounters challenges, revisiting the plan ensures it remains relevant and effective.
- Set vague or non-measurable goals. Goals should be specific enough to be objectively assessed for progress.
- Develop the plan without patient input. The patient's perspectives on their own needs and goals are crucial for a beneficial treatment plan.
- Forget to include the patient’s signature. Omitting this can imply lack of consent or agreement, undermining the therapeutic process.
- Overlook the importance of detailed documentation. Every element of the treatment plan should be clearly documented, including interventions and the rationale behind them.
- Neglect to consider the patient’s strengths and resources. Utilizing the patient’s available resources can significantly enhance the effectiveness of the treatment.
- Assume the plan is static. Treatment plans are dynamic documents that should evolve as the patient's needs and circumstances change.
Misconceptions
When navigating the complexities of mental health care, understanding the components and intentions behind a treatment plan is crucial. However, there are common misconceptions about treatment plans that can hinder a patient's journey towards recovery. Let's address some of these misunderstandings:
Treatment plans are solely created by therapists. A common misconception is that therapists unilaterally decide what goes into a treatment plan. In reality, effective treatment plans are co-created with the patient, ensuring their needs, concerns, and goals are central. This collaborative approach ensures the patient's agreement and commitment to the proposed treatment strategy.
Goals are vague and non-measurable. Some might believe that treatment goals are abstract and difficult to measure. Contrary to this belief, treatment plans are designed to include goals that are objective, measurable, and include estimated time frames for goal completion. This helps in monitoring progress and making necessary adjustments.
A signature is not necessary. The importance of documenting a patient's agreement through their signature is often underestimated. This signature is not a mere formality; it signifies the patient's understanding and active commitment to their treatment plan.
Treatment plans are fixed and inflexible. It's a common misunderstanding that once a treatment plan is created, it cannot be changed. Treatment plans are dynamic documents that are reviewed and revised according to the patient's progress and changing needs.
All treatment plans are the same. Each individual's struggles, strengths, and life circumstances are unique. Consequently, treatment plans are highly individualized, tailored to align with the specific goals and needs of each patient.
Treatment plans only address immediate issues. While short-term stabilization might be a focus, treatment plans also encompass long-term goals such as maintaining symptom stabilization and developing coping strategies, ensuring a comprehensive approach to mental health care.
Only conventional therapy methods are included. Treatment plans can include a variety of interventions beyond traditional talk therapy, such as medication referrals, stress management techniques, problem-solving skills training, and more, to cater to the diverse needs of patients.
There's no need to engage significant others. Involving family or significant others is often overlooked but can be a crucial component of a treatment plan. Engaging them can provide additional support and facilitate better outcomes for the patient.
Estimating time frames for goals is unnecessary. Some may think that setting estimated time frames for achieving goals is not essential. However, these time frames serve as benchmarks that can motivate both the patient and therapist, providing clear targets to work towards.
Unraveling these misconceptions about treatment plans can empower patients, ensuring they understand and actively participate in their journey towards healing. Remember, a well-crafted treatment plan is a roadmap to recovery, tailored to meet individual needs, preferences, and circumstances.
Key takeaways
When dealing with a Treatment Plan form, it's crucial to absorb several key takeaways to ensure it's filled out correctly and serves its intended purpose effectively. These points guide both the professional preparing the form and the patient it concerns.
- Goals should be objective and measurable: It’s important that the treatment goals listed on the form are not vague. They need to be specific, objective, and measurable, which means they should describe the desired outcome in a way that can be clearly evaluated.
- Include estimated time frames: For each goal listed in the treatment plan, an estimated timeframe for achieving the goal should be provided. This helps in creating a timeline for the patient's progress and ensures that the goals are time-bound.
- Develop plans with patient involvement: The treatment plan should be developed in collaboration with the patient. This ensures that the patient is actively involved in their own care and agrees to the proposed interventions and goals.
- Document patient agreement: The form should include a section where the patient can sign to indicate their agreement to the treatment plan. This is a critical aspect as it confirms the patient’s consent and understanding of the plan.
- Detail treatment goals: Under the treatment goals section, there should be clear documentation regarding what is aimed to be achieved through the treatment. This could include reducing risk factors or symptoms, improving functional impairments, and developing coping strategies, among others.
- Plan interventions consistent with goals: The planned interventions outlined in the form should directly correlate with the established treatment goals. This alignment is crucial to ensure that the selected interventions will effectively contribute to achieving the goals.
- Include a variety of interventions: The form offers a wide range of potential interventions such as assertiveness training, problem-solving skills training, cognitive restructuring, and more. Tailoring these interventions to the patient’s specific needs is crucial for the plan’s success.
- Plan for patient participation: It's essential to include strategies for engaging the patient in the treatment process. This might involve teaching new skills, educational activities, or assigning specific tasks for the patient to complete.
- Understand estimated timeframes: Recognize the importance of the estimated timeframes for achieving the goals. They provide a structured timeline that can be used to monitor progress and make adjustments as necessary.
In conclusion, a Treatment Plan form is a comprehensive tool that requires careful consideration and collaboration between the therapist and the patient. Understanding these key takeaways can significantly enhance the effectiveness of the treatment planning process.
Popular PDF Forms
How to Renew Your Cna License in Texas - The Texas Nurse Aide Registry uses information from the form to update the public and employers about a nurse aide’s certification status.
Lic38 - The form requests information about any company associated with the applicant's electrician’s license that has unpaid fees, promoting financial accountability.