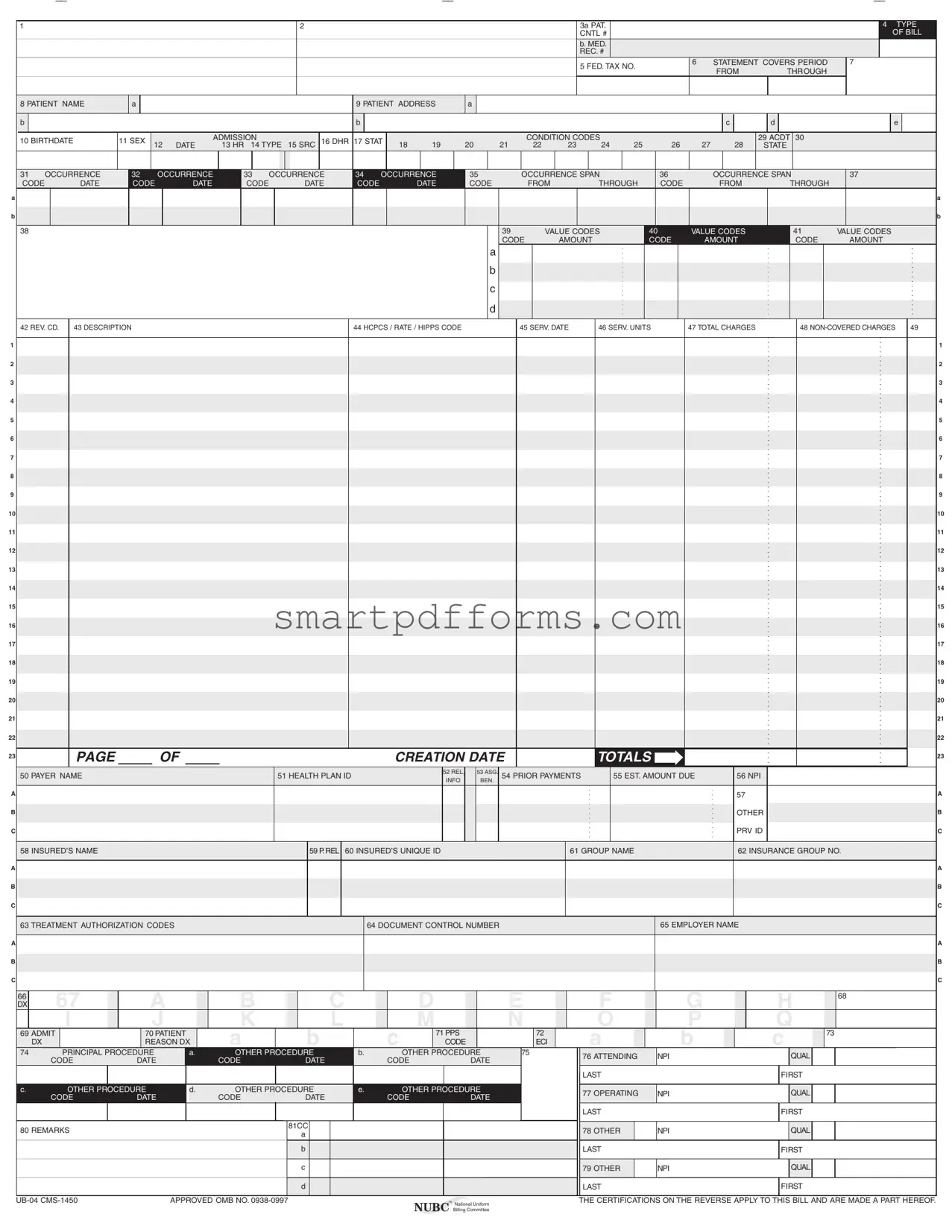
Blank Ub04 PDF Template
Navigating the complexities of healthcare billing and insurance claims is a task that often involves a deep dive into specialized forms, among which the UB-04 form stands out due to its comprehensive application across various healthcare facilities. This form, also known as CMS-1450, is integral for hospitals, nursing facilities, and other healthcare providers when submitting claims to Medicare and Medicaid as well as to private insurers. It meticulously captures a wide range of data, including patient information, diagnosis codes, the specifics of the treatment or services provided, and the financial aspects related to the billing and insurance. With boxes designated for everything from the patient's personal and insurance information to the details of each service provided—including service dates, charges, and the healthcare provider's National Provider Identifier (NPI)—the UB-04 form effectively acts as a bridge between the healthcare provider and the payer. Ensuring accurate and complete filling of this form is crucial; errors or omissions can lead to claim rejections or delays in payments. Further complicating its use, the form comes with a set of certifications on its reverse, underscoring the legal obligations tied to its submission, including adherence to federal and state laws concerning the accuracy of the submitted information and the implications of any misrepresentations.
Preview - Ub04 Form
A
B
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
A
B
C
A
B
C
A
B
C
1 |
2 |
3a PAT. |
|
|
|
|
|
4 TYPE |
|
|
CNTL # |
|
|
|
|
|
OF BILL |
|
|
b. MED. |
|
|
|
|
|
|
|
|
REC. # |
|
|
|
|
|
|
|
|
5 FED. TAX NO. |
6 |
STATEMENT COVERS PERIOD |
7 |
|
||
|
|
|
FROM |
THROUGH |
|
|
||
|
|
|
|
|
|
|
||
8 PATIENT NAME |
a |
|
|
|
|
9 PATIENT ADDRESS |
a |
|
|
|
|
|
|
|
|
|
|
||
b |
|
|
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
c |
d |
e |
10 BIRTHDATE |
11 SEX |
|
|
ADMISSION |
|
16 DHR 17 STAT |
|
|
|
|
CONDITION CODES |
|
|
|
|
|
29 ACDT 30 |
|
|
12 |
DATE |
13 HR 14 TYPE |
15 SRC |
18 |
19 |
20 |
21 |
22 |
23 |
24 |
25 |
26 |
27 |
28 |
STATE |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
31 OCCURRENCE |
32 |
|
OCCURRENCE |
33 |
OCCURRENCE |
34 |
OCCURRENCE |
35 |
|
|
|
OCCURRENCE SPAN |
|
36 |
|
|
|
OCCURRENCE SPAN |
|
37 |
|
|
|
||||||||||||||||||||||||||||||
CODE |
DATE |
CODE |
|
DATE |
CODE |
|
|
|
DATE |
CODE |
|
DATE |
CODE |
|
|
|
FROM |
THROUGH |
|
CODE |
|
|
FROM |
|
THROUGH |
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
38 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
39 |
|
|
VALUE CODES |
40 |
|
|
VALUE CODES |
|
41 |
|
VALUE CODES |
|
|
||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CODE |
|
AMOUNT |
|
|
|
CODE |
|
|
AMOUNT |
|
CODE |
|
AMOUNT |
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
a |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
c |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
d |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
42 REV. CD. |
43 DESCRIPTION |
|
|
|
|
|
|
|
|
|
|
|
|
|
44 HCPCS / RATE / HIPPS CODE |
|
|
|
|
45 SERV. DATE |
46 SERV. UNITS |
47 TOTAL CHARGES |
|
|
48 |
49 |
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
5 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
6 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
7 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
8 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
9 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
10 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
11 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
12 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
13 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
14 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
15 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
16 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
17 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
18 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
19 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
20 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
21 |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
22 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PAGE |
|
|
OF |
|
|
|
|
|
|
|
|
|
|
CREATION DATE |
|
|
|
|
|
|
|
TOTALS |
|
|
|
|
|
|
|
|
|
|
|
|
|
23 |
|||||||||||||||
50 PAYER NAME |
|
|
|
|
|
|
|
|
51 HEALTH PLAN ID |
|
|
|
|
52 REL. |
|
53 ASG. |
54 PRIOR PAYMENTS |
|
55 EST. AMOUNT DUE |
|
|
56 NPI |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
INFO |
|
BEN. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
57 |
|
|
|
|
|
|
|
|
A |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
OTHER |
|
|
|
|
|
|
|
|
B |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
PRV ID |
|
|
|
|
|
|
|
|
C |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
58 INSURED’S NAME |
|
|
|
|
|
|
|
|
|
|
|
59 P. REL |
60 INSURED’S UNIQUE ID |
|
|
|
|
|
|
|
|
61 GROUP NAME |
|
|
|
|
|
|
|
62 INSURANCE GROUP NO. |
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
C |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
63 TREATMENT AUTHORIZATION CODES |
|
|
|
|
|
|
|
|
64 DOCUMENT CONTROL NUMBER |
|
|
|
|
|
|
|
|
|
|
|
|
65 EMPLOYER NAME |
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
A |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
B |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
C
66 |
67 |
A |
|
B |
|
C |
|
D |
|
E |
F |
G |
H |
68 |
DX |
|
|
|
|
|
|||||||||
|
I |
J |
|
K |
|
L |
|
M |
|
N |
O |
P |
Q |
|
69 ADMIT |
70 PATIENT |
|
A |
B |
|
C |
71 PPS |
|
72 |
A |
B |
C |
73 |
|
|
DX |
REASON DX |
|
CODE |
|
ECI |
|
|||||||
74 |
PRINCIPAL PROCEDURE |
a. |
OTHER PROCEDURE |
b. |
|
OTHER PROCEDURE |
75 |
76 ATTENDING |
NPI |
QUAL |
|
|||
|
CODE |
DATE |
|
CODE |
DATE |
|
CODE |
DATE |
|
|
||||
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
LAST |
|
FIRST |
|
c. |
OTHER PROCEDURE |
d. |
OTHER PROCEDURE |
e. |
|
OTHER PROCEDURE |
|
77 OPERATING |
NPI |
QUAL |
|
|||
|
CODE |
DATE |
|
CODE |
DATE |
|
CODE |
DATE |
|
|
||||
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
LAST |
|
FIRST |
|
80 REMARKS |
|
|
|
81CC |
|
|
|
|
|
78 OTHER |
NPI |
QUAL |
|
|
|
|
|
a |
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
b |
|
|
|
|
|
LAST |
|
FIRST |
|
|
|
|
|
|
c |
|
|
|
|
|
79 OTHER |
NPI |
QUAL |
|
|
|
|
|
|
d |
|
|
|
|
|
LAST |
|
FIRST |
|
APPROVED OMB NO. |
™ National Uniform |
THE CERTIFICATIONS ON THE REVERSE APPLY TO THIS BILL AND ARE MADE A PART HEREOF. |
|
|
|
NUBC Billing Committee |
|

Submission of this claim constitutes certification that the billing information as shown on the face hereof is true, accurate and complete. That the submitter did not knowingly or recklessly disregard or misrepresent or conceal material facts. The following certifications or verifications apply where pertinent to this Bill:
1.If third party benefits are indicated, the appropriate assignments by the insured /beneficiary and signature of the patient or parent or a legal guardian covering authorization to release information are on file. Determinations as to the release of medical and financial information should be guided by the patient or the patient’s legal representative.
2.If patient occupied a private room or required private nursing for medical necessity, any required certifications are on file.
3.Physician’s certifications and
4.For Religious
5.Signature of patient or his representative on certifications, authorization to release information, and payment request, as required by Federal Law and Regulations (42 USC 1935f, 42 CFR 424.36, 10 USC 1071 through 1086, 32 CFR 199) and any other applicable contract regulations, is on file.
6.The provider of care submitter acknowledges that the bill is in conformance with the Civil Rights Act of 1964 as amended. Records adequately describing services will be maintained and necessary information will be furnished to such governmental agencies as required by applicable law.
7.For Medicare Purposes: If the patient has indicated that other health insurance or a state medical assistance agency will pay part of his/her medical expenses and he/she wants information about his/her claim released to them upon request, necessary authorization is on file. The patient’s signature on the provider’s request to bill Medicare medical and
8.For Medicaid purposes: The submitter understands that because payment and satisfaction of this claim will be from Federal and State funds, any false statements, documents, or concealment of a material fact are subject to prosecution under applicable Federal or State Laws.
9.For TRICARE Purposes:
(a)The information on the face of this claim is true, accurate and complete to the best of the submitter’s knowledge and belief, and services were medically necessary and appropriate for the health of the patient;
(b)The patient has represented that by a reported residential address outside a military medical treatment facility catchment area he or she does not live within the catchment area of a U.S. military medical treatment facility, or if the patient resides within a catchment area of such a facility, a copy of
(c)The patient or the patient’s parent or guardian has responded directly to the provider’s request to identify all health insurance coverage, and that all such coverage is identified on the face of the claim except that coverage which is exclusively supplemental payments to
(d)The amount billed to TRICARE has been billed after all such coverage have been billed and paid excluding Medicaid, and the amount billed to TRICARE is that remaining claimed against TRICARE benefits;
(e)The beneficiary’s cost share has not been waived by consent or failure to exercise generally accepted billing and collection efforts; and,
(f)Any
(g)Based on 42 United States Code 1395cc(a)(1)(j) all providers participating in Medicare must also participate in TRICARE for inpatient hospital services provided pursuant to admissions to hospitals occurring on or after January 1, 1987; and
(h)If TRICARE benefits are to be paid in a participating status, the submitter of this claim agrees to submit this claim to the appropriate TRICARE claims processor. The provider of care submitter also agrees to accept the TRICARE determined reasonable charge as the total charge for the medical services or supplies listed on the claim form. The provider of care will accept the
SEE http://www. nubc . org/ FOR MORE INFORMATION ON
Form Data
| Fact Name | Description |
|---|---|
| Form Identifier | The form is known as UB-04 or CMS-1450. |
| Governing Entity | The National Uniform Billing Committee (NUBC) is responsible for the form's creation and updates. |
| Purpose | It is used for hospital billing and claims processing for inpatient and outpatient services. |
| Legal Considerations | Submission implies certification that information is accurate and truthful, potentially leading to civil or criminal penalties for misrepresentation under federal and/or state law(s). |
Instructions on Utilizing Ub04
Filling out the UB-04 form is a critical step in the billing process for health care services. This form ensures that all necessary information is provided in a standardized manner, facilitating the reimbursement process from insurance companies, Medicare, or Medicaid. Accurate completion of the UB-04 form is essential to avoid delays or rejections of claims. Below are step-by-step instructions to guide you through each section of the form.
- Enter the provider's name, address, and telephone number in fields A and B, at the top of the form.
- In field 1, place the type of health insurance coverage relevant to the claim.
- In fields 2 through 4, provide the patient's personal information, including their name, address, and birthdate.
- Fill in the patient's medical record number and the federal tax number in fields 5 and 6.
- For fields 6 through 8, document the statement covers period, indicating the start and end dates of the service period.
- Enter the patient's name in field 8 and their address in field 9.
- In field 10, specify the patient's birthdate and sex in fields 11 and 12.
- Detail the admission and discharge information, including date, hour, type, and source in fields 12 through 15.
- For fields 16 through 31, identify condition codes, dates, and details relating to the patient’s treatment.
- List occurrence codes and dates relevant to the patient's condition in fields 32 through 35.
- Fields 36 and 37 require information on occurrence spans and related codes.
- In fields 38 through 41, enter value codes and amounts that apply to the patient's care.
- Fields 42 through 49 are designed for revenue codes, descriptions, and amounts charged for services.
- Provide details of the payer(s) in fields 50 through 58, including the name, relationship, and identification numbers.
- In field 59, fill in the insured's name and relationship to the patient.
- Fields 60 through 72 require information relating to the insured's policy, including group numbers and treatment authorization codes.
- Document diagnosis and procedure codes relevant to the patient's treatment in fields 67 through 75.
- In fields 76 through 81, enter the NPI and qualifications of attending and other physicians involved in the care.
- Finally, in the remarks section, field 80, provide any additional information necessary for the processing of the claim.
Careful attention to detail and completeness when filling out the UB-04 form is paramount. This process ensures that all required information is conveyed accurately, making the reimbursement process as smooth as possible. Remember, the information provided on this form is the basis for billing insurance carriers, Medicaid, and Medicare, and thereby directly impacts the timely receipt of payments for services rendered.
Obtain Answers on Ub04
FAQs about the UB-04 Form
What is a UB-04 form?
The UB-04 form, also known as the CMS-1450 form, is a document used by hospitals and medical facilities to bill medical insurance providers for services provided to patients. It's recognized by Medicare, Medicaid, and most insurance companies.
Who needs to use the UB-04 form?
This form is primarily used by hospitals, nursing facilities, outpatient clinics, and other healthcare providers when submitting claims to Medicare or Medicaid and commercial insurers for reimbursement of medical services.
Are there specific requirements for filling out the UB-04 form?
Yes, there are detailed requirements for completing the UB-04 form which include accurately filling out patient information, provider details, services codes, dates of service, and charges. Accurate completion is crucial to ensure timely and accurate reimbursement.
Can the UB-04 form be submitted electronically?
Yes, while the UB-04 can be submitted in paper format, many institutions submit these forms electronically, known as Electronic Data Interchange (EDI), to speed up the claims process and reduce errors.
Where can I find a UB-04 form?
UB-04 forms can be acquired through the official National Uniform Billing Committee (NUBC) website, healthcare form vendors, or directly from some insurance carriers.
What information is required in the patient address section of the UB-04 form?
The patient address section requires the full address of the patient, including street name and number, city, state, and zip code, to ensure the patient can be correctly identified and communicated with by the insurer.
How is the patient's diagnosis reported on the UB-04 form?
Diagnoses are reported using ICD codes in the designated field. These codes provide a standardized way to represent the patient’s condition and the reason for the medical services provided.
What do the value codes in sections 39-41 represent?
Value codes in these sections are used to report various financial information related to the claim, such as insurance co-pay amounts, deductible amounts, or amounts paid by other insurers, which are crucial for calculating the final reimbursement.
How do I know if my UB-04 form has been accepted or rejected?
After submitting the UB-04 form, the insurance company or payer will process the claim and issue a response. This will typically be a payment for accepted claims or an explanation of benefits (EOB) statement detailing reasons for any denial or adjustments.
Common mistakes
When filling out the UB-04 form, a comprehensive document used for hospital billing, many tend to make mistakes. Below is an expanded list of ten common errors that present challenges for both the individual completing the form and the processing of their billing.
- Incomplete fields: Often, some sections are left blank. Every applicable field needs to be filled out for the form to be processed correctly.
- Incorrect patient information: Patient details such as name, address, and date of birth must match what’s on record. Discrepancies can lead to claim rejections.
- Misentered insurance information: Incorrect insurance ID numbers, payer names, or health plan IDs will direct the bill to the wrong company, causing delays.
- Errors in the provider section: The Provider’s National Provider Identifier (NPI) and Tax Identification Number (TIN) must be correctly entered. Mistakes here can misroute the claim.
- Service dates conflict: The admission and discharge dates need to reflect the actual period of service. Conflicting dates can raise questions about the services billed.
- Wrong codes for diagnoses and procedures: Diagnosis and procedure codes must be accurate and up-to-date according to ICD standards. Incorrect coding can lead to denied claims due to perceived inaccuracy in services rendered.
- Missing signatures: If the form requires a signature for verification or authorization and it is not present, the form can be considered incomplete.
- Incorrect bill type codes: The bill type code indicates the setting of the service and the type of bill being submitted. An incorrect code can send the bill to the wrong department or even dismiss it as irrelevant.
- Failure to include condition codes: Condition codes provide additional information about the conditions under which a service was provided. Omitting these can leave out critical context for the bill.
- Overlooking the importance of sequence numbers: For facilities submitting multiple pages, sequence numbers ensure pages are processed in the right order. Out-of-order pages can confuse the billing process.
To ensure successful and timely processing of the UB-04 form, considerable attention must be given to completing it accurately. Common mistakes can be avoided by reviewing each section carefully, confirming that all applicable fields are filled out, and ensuring that all entries match the required documentation and current coding standards.
Documents used along the form
In healthcare, accurately billing for services rendered is crucial, and the UB-04 form plays a central role in this process for hospitals and other healthcare providers. However, the UB-04 is often just one piece of a much larger puzzle. Accompanying this essential form, there are several other documents and forms frequently utilized to ensure the comprehensive capture of patient care details, insurance information, and to meet various legal and regulatory requirements. Understanding these supplementary documents can help navigate the complex landscape of healthcare billing and administration.
- HIPAA Authorization Form - This document is used to ensure compliance with the Health Insurance Portability and Accountability Act, allowing the healthcare provider to share patient health information for billing purposes.
- Medical Records Release Form - This form is used when patient health information needs to be shared between different healthcare providers or institutions. It requires patient consent to release medical records.
- Assignment of Benefits (AOB) Form - The AOB form permits the healthcare provider to bill an insurance company directly and receive payment without going through the patient.
- Advance Beneficiary Notice of Noncoverage (ABN) - This form is given to Medicare patients when the provider believes Medicare may not pay for some services. It makes patients aware they may be responsible for the costs.
- Notice of Privacy Practices - This document outlines how a patient's personal health information will be used and disclosed by the healthcare provider. It also explains the patient's rights regarding their health information.
- Consent to Treat Form - Before receiving any medical treatment, patients are often required to sign a consent form acknowledging they understand the upcoming procedures and agree to them.
- Insurance Verification Form - This form is used to verify the patient’s insurance coverage and benefits before services are rendered, ensuring the provider and patient understand coverage extents.
- Coordination of Benefits (COB) Form - In situations where a patient has multiple insurance plans, the COB form helps determine the primary and secondary payers to streamline the billing process.
- Medicare Secondary Payer (MSP) Questionnaire - This questionnaire is necessary when a Medicare beneficiary has other insurance that may cover the services, helping determine which insurer pays first.
- Pharmacy Medication Prior Authorization Requests - These requests are necessary when a patient’s medication requires approval from the insurance company to ensure coverage before the prescription is filled.
Each of these documents serves a specific purpose, contributing to a thorough and lawful healthcare billing process. While the UB-04 form captures the bulk of service and billing information, these additional forms address consent, legal compliance, patient rights and responsibilities, and coordination among payers. Together, they allow for a transparent, efficient, and compliant healthcare delivery and billing system. Understanding their functions and how they interconnect with the UB-04 form can significantly aid any healthcare provider or billing specialist in navigating the challenges of healthcare administration.
Similar forms
The HCFA-1500 form, also known as the CMS-1500, is similar to the UB-04 form as both are used for billing insurance providers for healthcare services. While the UB-04 is predominantly used by hospitals and institutional facilities, the HCFA-1500 is primarily for non-institutional providers like physicians and therapists. Both forms collect patient demographics, insurance information, diagnosis codes, and charges for services provided.
The ANSI 837 Health Care Claim is an electronic version of the paper-based claims like UB-04, designed for the same purpose but in a format suitable for electronic data interchange (EDI). It allows healthcare providers to submit claims electronically to payers, including Medicare and Medicaid, ensuring faster processing and reduced errors compared to manual submission.
The ADA Dental Claim Form shares similarities with the UB-04 form in that it is used for billing purposes but is specifically designed for dental services. Like the UB-04, it collects information on the provider, patient, and services performed but focuses on dental procedures, diagnoses, and related costs.
The Durable Medical Equipment (DME) Claim Form is parallel in function to the UB-04 form, tailored for suppliers of medical equipment to bill Medicare, Medicaid, or private insurances. It captures provider and beneficiary information, details of the equipment provided, and the cost, similar to how the UB-04 documents hospital services and charges.
The Superbill is comparable to the UB-04 as it provides a comprehensive summary of care provided during a patient's visit, including personal, insurance, and service details. Unlike the UB-04, a superbill is often used in outpatient settings and directly handed to patients for them to submit for insurance reimbursement.
The Pharmacy Claim Form is used by pharmacists to bill third-party payers for medications dispensed to insured patients. It shares the billing and insurance functionalities of the UB-04 form but is specifically focused on pharmaceutical transactions, including drug codes, quantities, and costs.
The Home Health Care Claim Form is utilized by home health agencies to bill for services provided in a patient's home, similar to how hospitals use the UB-04 for facility-based services. Both forms collect data on service dates, provider details, patient information, and charges but cater to their respective healthcare service settings.
The SNF (Skilled Nursing Facility) Claim Form is similar to the UB-04 form as it is used by long-term care facilities to submit charges for patient care to Medicare, Medicaid, and other insurers. It includes patient demographics, service details, diagnosis codes, and procedural codes akin to those found on the UB-04, but within the context of a skilled nursing environment.
Dos and Don'ts
When filling out the UB-04 form, accuracy and attention to detail are paramount. Here are some tips on what you should and shouldn't do to ensure the process goes smoothly:
Things You Should Do:
- Double-check patient information, including name, address, and birthdate, for accuracy.
- Ensure that the Federal Tax Number is correctly entered, as it is critical for billing purposes.
- Be precise with dates, such as admission and discharge dates, to avoid any confusion or delays.
- Verify that the diagnosis and procedure codes are current and correctly reflect the patient's condition and the services provided.
- Enter the correct NPI (National Provider Identifier) numbers for the attending, operating, and other providers involved in the care.
- Review the form for completeness and correctness before submission, including checking that all necessary fields are filled out.
Things You Shouldn't Do:
- Avoid leaving mandatory fields empty; missing information can lead to claim rejections.
- Do not use outdated or incorrect diagnosis or procedure codes; this can lead to delayed or denied payments.
- Refrain from guessing on codes or dates; if unsure, verify the information first.
- Avoid entering personal opinions or unverified information in the remarks section; stick to factual and relevant details.
- Do not rush through the form; taking your time can prevent errors and omissions.
- Do not forget to keep a copy of the submitted form for your records; documentation is key should any issues arise.
Misconceptions
Many individuals working in healthcare or insurance might think they fully understand the UB-04 form, also known as the CMS-1450 form. However, there are several misconceptions about it that can lead to confusion or errors. Here are ten common misconceptions and the truths behind them.
- Misconception 1: The UB-04 form is only for hospital billing.
- Misconception 2: Every field on the UB-04 form must be completed.
- Misconception 3: The UB-04 form can be submitted manually for all insurance types.
- Misconception 4: All diagnosis codes fit within the UB-04 form.
- Misconception 5: The form number (UB-04) never changes.
- Misconception 6: The UB-04 form is identical across all states.
- Misconception 7: The term "UB" in UB-04 stands for "Universal Billing."
- Misconception 8: You can use the UB-04 form for outpatient services only.
- Misconception 9: The use of the UB-04 form is optional.
- Misconception 10: Understanding and completing the UB-04 form requires no special training.
This is not accurate. While the UB-04 form is primarily used in hospital billing, it is also utilized by nursing facilities, home health agencies, and other providers of healthcare services for institutional billing purposes.
Not every field on the UB-04 form is required for every submission. The necessity of specific fields depends on the payer's requirements and the type of claim being submitted. It's crucial to understand the instructions for each field to determine if completion is necessary for your specific situation.
While the UB-04 can be manually completed, not all insurers accept physical forms. Many require electronic submission through specific platforms or services, especially in the case of Medicare and Medicaid.
The UB-04 form has limits on the number of diagnosis codes that can be reported. Providers need to prioritize the primary diagnosis and the most pertinent additional diagnoses, considering the form only allows for a specific number of codes.
The name "UB-04" refers to the current version of the form. Just as the UB-92 form was replaced by the UB-04, future updates or revisions could result in a form with a different name or number. It's important to stay current with the most recent version to ensure compliance.
While the UB-04 form is standardized, certain states or payers might have specific requirements or use state-specific fields. Always verify with the payer or consult state regulations to ensure compliance.
Actually, "UB" refers to "Uniform Billing." The form aims to standardize institutional provider billing and facilitate the processing and settlement of claims.
Incorrect. The UB-04 form is designed for both inpatient and outpatient billing, covering a wide range of healthcare services provided by institutions.
For institutional providers billing Medicare and most Medicaid plans, using the UB-04 form is not optional but a requirement. Many private insurers also mandate its use for certain types of claims.
Given the complexity and specific billing codes and requirements, proper completion of the UB-04 form often requires specialized knowledge and training. Misunderstandings or errors can lead to claim denials or delays in payment.
Clearing up these misconceptions is essential for efficient and accurate billing in the healthcare field. Familiarizing oneself with the instructions for the UB-04 form and staying updated with changes are crucial steps in the billing process.
Key takeaways
Filling out the UB-04 form, officially known as the CMS-1450 form, is a critical process for healthcare providers seeking reimbursement from insurance companies, including Medicare and Medicaid. This form requires precise and accurate input of data to ensure that claims are processed efficiently and correctly. Below are five key takeaways to consider when dealing with the UB-04 form:
- Accuracy is paramount: Every field on the UB-04 form must be filled out with the most current and accurate information. This includes patient information, hospital services provided, and specific billing codes. Errors or omissions can lead to claim rejections or delays in payment.
- Understand billing codes: The form requires detailed coding, including Revenue Codes (Field 42), HCPCS/Rates/HIPPS Code (Field 44), and diagnosis and procedure codes. Familiarity with these codes and how they apply to the treatment provided is essential for correct billing.
- Documentation and certification: Submission of the UB-04 form certifies that all information is true and accurate and that the provider has complied with federal and state regulations regarding billing practices. It's crucial to have all required documentation, such as physician certifications and treatment authorizations, on file and readily available if requested by the payer.
- Understanding payer requirements: Different insurance providers might have specific instructions or requirements for submitting a UB-04 form. It's essential to be aware of these nuances to ensure that the form is completed in accordance with the payer's expectations, thus minimizing the risk of claim denial.
- Stay updated: Healthcare billing regulations and requirements can change. Providers must stay informed about updates to billing codes, form fields, and regulatory requirements to ensure compliance and to facilitate the prompt and accurate processing of claims.
In summary, the successful use of the UB-04 form hinges on attention to detail, a deep understanding of billing codes and payer requirements, and a commitment to maintaining accurate and up-to-date patient records and documentation. By diligently applying these principles, healthcare providers can streamline their billing processes, reduce the incidence of claim denials, and ensure timely reimbursement for services rendered.
Popular PDF Forms
Reg 256 Ca Dmv - Includes mechanisms for verifying applicant claims, such as the requirement to attach reports from medical professionals for vision conditions.
Buyers Financial Information Form - The form requires disclosure of the buyer's employment details, contributing to a comprehensive financial assessment.
Form It38 - Calculate any interest due on unpaid tax by referring to the daily interest rates provided on the Revenue's website.