Blank Va 10 7959C PDF Template
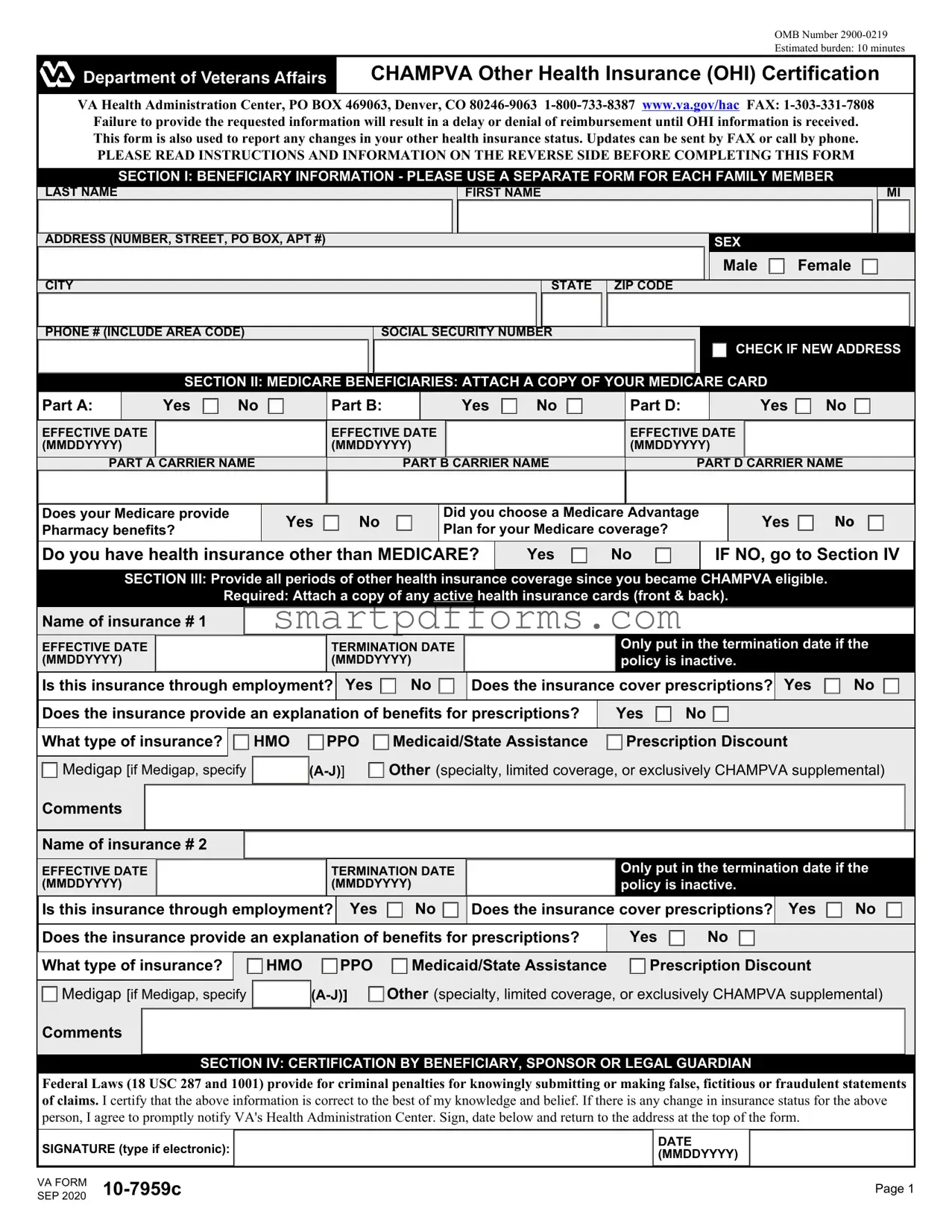
Ensuring that beneficiaries of the Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA) maintain their entitlements without unnecessary interruptions requires the accurate and timely reporting of any other health insurance (OHI) coverage they may have. The VA Form 10-7959C, designated for CHAMPVA Other Health Insurance Certification, emerges as a critical tool in this process. Required by the VA Health Administration Center, this form not only facilitates the coordination of benefits but also aims to prevent delays or denials in reimbursements due to undisclosed OHI information. Beneficiaries, including those who have Medicare, are tasked with providing comprehensive details regarding their other health insurance coverage. This form rigorously seeks information that spans beneficiary identification, detailed Medicare coverage, as well as periods and types of other existing health insurance. Furthermore, it emphasizes the necessity of attaching copies of Medicare and other health insurance cards to ensure clarity in coverage specifics. The form serves as a declaration by the beneficiary, sponsor, or legal guardian on the accuracy of the reported information, with a stern reminder of the legal ramifications for falsehoods. Embedded within its structure are instructions aimed at guiding the filling process, underscored by definitions that clarify the meaning of terms used within the form. Guided by the principles of the Privacy Act and the Paperwork Reduction Act, the VA Form 10-7959c embodies a crucial step for CHAMPVA beneficiaries in maintaining their health care benefits seamlessly alongside other health insurance programs.
Preview - Va 10 7959C Form
OMB Number
Estimated burden: 10 minutes
CHAMPVA Other Health Insurance (OHI) Certification
VA Health Administration Center, PO BOX 469063, Denver, CO
PLEASE READ INSTRUCTIONS AND INFORMATION ON THE REVERSE SIDE BEFORE COMPLETING THIS FORM
SECTION I: BENEFICIARY INFORMATION - PLEASE USE A SEPARATE FORM FOR EACH FAMILY MEMBER
LAST NAME
FIRST NAME
MI
ADDRESS (NUMBER, STREET, PO BOX, APT #)
SEX
Male  Female
Female 
CITY |
STATE ZIP CODE |
PHONE # (INCLUDE AREA CODE) |
SOCIAL SECURITY NUMBER |
|
CHECK IF NEW ADDRESS |
SECTION II: MEDICARE BENEFICIARIES: ATTACH A COPY OF YOUR MEDICARE CARD
Part A: |
|
Yes |
|
No |
|
|
Part B: |
|
Yes |
|
No |
|
|
Part D: |
|
Yes |
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
EFFECTIVE DATE |
|
|
|
|
|
EFFECTIVE DATE |
|
|
|
|
|
EFFECTIVE DATE |
|
|
|
|
|
|||
(MMDDYYYY) |
|
|
|
|
|
(MMDDYYYY) |
|
|
|
|
|
(MMDDYYYY) |
|
|
|
|
|
|||
|
|
|
|
|
|
|||||||||||||||
PART A CARRIER NAME |
PART B CARRIER NAME |
PART D CARRIER NAME |
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Does your Medicare provide Pharmacy benefits?
Yes  No
No
Did you choose a Medicare Advantage Plan for your Medicare coverage?
Yes  NO
NO
Do you have health insurance other than MEDICARE?
Yes  No
No
IF NO, go to Section IV
SECTION III: Provide all periods of other health insurance coverage since you became CHAMPVA eligible.
Required: Attach a copy of any active health insurance cards (front & back).
Name of insurance # 1
|
EFFECTIVE DATE |
|
|
|
TERMINATION DATE |
|
|
|
Only put in the termination date if the |
|
||||||||||||||||||||||||
|
(MMDDYYYY) |
|
|
|
(MMDDYYYY) |
|
|
|
policy is inactive. |
|
|
|
|
|
|
|||||||||||||||||||
|
Is this insurance through employment? |
Yes |
|
|
|
No |
|
|
Does the insurance cover prescriptions? |
Yes |
|
No |
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Does the insurance provide an explanation of benefits for prescriptions? |
|
|
Yes |
|
No |
|
|
|
|
|
|
|
|
||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What type of insurance? |
|
|
HMO |
|
PPO |
|
|
|
Medicaid/State Assistance |
|
|
Prescription Discount |
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Medigap [if Medigap, specify |
|
|
|
Other (specialty, limited coverage, or exclusively CHAMPVA supplemental) |
|
|||||||||||||||||||||||||||
|
|
|
|
|
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Comments |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Name of insurance # 2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
EFFECTIVE DATE (MMDDYYYY)
TERMINATION DATE (MMDDYYYY)
Only put in the termination date if the policy is inactive.
|
Is this insurance through employment? |
Yes |
|
|
|
No |
|
|
Does the insurance cover prescriptions? |
Yes |
|
No |
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Does the insurance provide an explanation of benefits for prescriptions? |
|
Yes |
|
No |
|
|
|
|
|
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
What type of insurance? |
|
|
|
HMO |
|
PPO |
|
|
|
Medicaid/State Assistance |
|
Prescription Discount |
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Medigap [if Medigap, specify |
|
|
|
|
Other (specialty, limited coverage, or exclusively CHAMPVA supplemental) |
||||||||||||||||||||||
|
|
|
|
|
|
||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Comments
SECTION IV: CERTIFICATION BY BENEFICIARY, SPONSOR OR LEGAL GUARDIAN
Federal Laws (18 USC 287 and 1001) provide for criminal penalties for knowingly submitting or making false, fictitious or fraudulent statements of claims. I certify that the above information is correct to the best of my knowledge and belief. If there is any change in insurance status for the above person, I agree to promptly notify VA's Health Administration Center. Sign, date below and return to the address at the top of the form.
SIGNATURE (type if electronic):
VA FORM
SEP 2020
DATE (MMDDYYYY)
Page 1
CHAMPVA OTHER HEALTH INSURANCE (OHI) CERTIFICATION
NOTES, DEFINITIONS, AND INSTRUCTIONS
INSTRUCTIONS
Failure to complete all applicable sections on the front can result in a delay or denial of benefits. Use this form to report any changes in your other health insurance.
•New beneficiaries - we need OHI information from the date your CHAMPVA eligibility became effective.
•
•To specify a medicare supplement plan A - J, refer to your policy cover sheet or your insurance membership card.
•If there are additional policies use plain bond paper and either type or legibly print your name, SSN, and the information for each item. Attach to this form. If submitting this form electronically add an attachment to the submission.
ITEMS TO RETURN WITH THIS COMPLETED OTHER HEALTH INSURANCE (OHI) CERTIFICATION
•A COPY of your Medicare card (do NOT send the original)
•A COPY of your other health insurance (OHI) member ID card (front and back).
•If your OHI does not issue EOBs, then attach a copy (card or document) of your schedule of benefits that lists your
DEFINITIONS
OHI: OHI refers to insurance or benefits you may have other than CHAMPVA called “Other Health Insurance”.
EOB: The abbreviation for an “explanation of benefits” form or letter that must accompany claims submitted to CHAMPVA. An EOB is a statement or “Remittance Advice” from an insurance carrier or benefit program that summarizes the action taken on a claim.
Note: If you have OHI primary to CHAMPVA you must submit EOB's for each primary insurance along with health care claims. If your OHI does not issue EOB's i.e. some HMO's and PPO's, you must submit a copy of your active
Carrier: Carrier is the insurance company that provides your medical benefits.
OHI primary to CHAMPVA: CHAMPVA by law is always supplemental or the secondary payer of health care benefits except for Medicaid, State Victims of Crimes Compensation Programs, and policies purchased exclusively to supplement CHAMPVA benefits.
Supplemental CHAMPVA policies: These are policies specifically purchased for the purpose of covering your cost share after CHAMPVA has completed adjudication of a claim.
Medicare supplemental policies: These are policies that are specifically for the purpose of covering your Medicare out of pocket expenses. These Medicare supplemental policies such as “Medigap” or Policies offered through employment are primary to CHAMPVA and must provide an EOB along with the Medicare EOB (two EOBs) for each claim submitted to CHAMPVA.
Indemnity: Plans that pay a flat fee or daily rate to supplement lost income while hospitalized are called Indemnity Plans.
Termination date: This is the date the policy ended or ceased to be active. The end date for a period shown on a card that will be reissued is not the termination date. Closing a policy will generate a true termination date.
Privacy Act Information: The authority for collection of the requested information on this form is 38 USC 501 and 1781. The purpose of collecting this information is to determine payer status when other health insurance coverage exists. The information you provide may be verified by a computer matching program at any time. You are requested to provide your Social Security number as your VA record is filed and retrieved by this number. You do not have to provide the requested information on this form but if any or all of the requested information is not provided, it may delay or result in denial of your request for CHAMPVA benefits. Failure to furnish the requested information will have no adverse impact on any other VA benefit to which you may be entitled. The responses you submit are considered confidential and may be disclosed outside VA only if the disclosure is authorized under the Privacy Act, including the routine uses identified in the VA system of records number 54VA16, titled "Health Administration Center Civilian Health and Medical Program Records
Paperwork Reduction Act: This information collection is in accordance with the clearance requirements of Section 3507 of the Paperwork Reduction Act of 1995. Public reporting burden for this collection of information is estimated to average 10 minutes per response, including the time for reviewing instructions, searching existing data sources, gathering and maintaining the data needed, and completing and reviewing the collection of information. Comments regarding this burden estimate or any other aspect of this collection, including suggestions for reducing the burden, may be addressed by calling the CHAMPVA Help Line,
VA FORM |
Page 2 |
Form Data
| Fact Name | Detail |
|---|---|
| Form Purpose | The VA Form 10-7959c is used for CHAMPVA Other Health Insurance (OHI) Certification, to report changes in OHI status or provide initial information. |
| Submission Address | Submissions should be directed to the VA Health Administration Center, P.O. Box 469063, Denver, CO 80246-9063, with fax submissions to 1-303-331-7808. |
| OMB Number and Burden | The form has an OMB Number of 2900-0219 and an estimated completion time of 10 minutes. |
| Contact Information | For assistance, individuals can contact 1-800-733-8387 or visit www.va.gov/hac. |
| Penalty for False Statements | Under Federal Laws (18 USC 287 and 1001), knowingly submitting false, fictitious, or fraudulent statements or claims can lead to criminal penalties. |
Instructions on Utilizing Va 10 7959C
After completing the VA Form 10-7959c, an individual takes a vital step towards managing their benefits under the CHAMPVA program. This form, essential for those with other health insurance (OHI), enables the smooth processing of claims and ensures that reimbursements are handled correctly. It's crucial to update this form whenever there's a change in OHI status, preventing any unnecessary delays or denials in the receipt of benefits. Here's a step-by-step guide on how to fill out this form:
- Read the instructions carefully on the reverse side of the form to ensure a thorough understanding of the required information.
- In Section I: Beneficiary Information, enter the beneficiary's last name, first name, middle initial, and complete address, including the zip code. Specify the beneficiary's sex by checking the appropriate box. Provide the phone number with the area code and the Social Security Number. Check the box if it's a new address.
- For Medicare beneficiaries (Section II), indicate whether you have Part A, B, or D by checking 'Yes' or 'No'. Include the effective dates for each applicable part. Attach a copy of your Medicare card as instructed.
- If you have health insurance other than Medicare (Section III):
- List each insurance, including the effective and termination dates. Only include a termination date if the policy is inactive.
- Indicate whether the insurance is through employment and if it covers prescriptions.
- Specify the type of insurance (HMO, PPO, Medicaid/State Assistance, etc.) and add any relevant comments.
- Attach a copy of any active health insurance card(s) (front and back) for each listed insurance.
- Section IV: Certification requires the signature of the beneficiary, sponsor, or legal guardian, certifying the accuracy of the information provided. Also, include the date next to the signature.
- Review the form to ensure all information is correct and complete. Attach any additional required documents as listed in the instructions, such as copies of Medicare and other health insurance cards.
- Return the completed form and all attachments to the provided address, or send by fax if preferred. Keep a copy of everything for your records.
Once this form is submitted, it will be reviewed by the VA Health Administration Center. They may reach out if further information is needed or to update you on the status of your reimbursement or benefits. Remember, timely updates to your OHI information using this form are crucial to receiving your benefits without delay.
Obtain Answers on Va 10 7959C
Welcome to the FAQ section about the VA Form 10-7959c, commonly referred to as the CHAMPVA Other Health Insurance (OHI) Certification. This form plays an essential role for beneficiaries of the Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA) who have other health insurance coverage. Below are answers to some of the most commonly asked questions regarding this form.
What is the purpose of VA Form 10-7959c?
This form is used by CHAMPVA beneficiaries to report other health insurance (OHI) information to the VA. It helps ensure that CHAMPVA can properly coordinate benefits. This coordination is necessary when a beneficiary has health insurance in addition to CHAMPVA, including Medicare, allowing for the correct processing and reimbursement of healthcare claims.
When do I need to complete and submit this form?
There are several instances when you need to submit this form:
- When you first become eligible for CHAMPVA benefits and have another health insurance coverage.
- Anytime there is a change in your OHI status, such as acquiring new insurance, changes in existing coverage, or losing coverage.
How can I submit VA Form 10-7959c?
You have a couple of options for submitting the form:
- Mail: Send the completed form to the VA Health Administration Center at PO BOX 469063, Denver, CO 80246-9063.
- Fax: Fax the form to 1-303-331-7808.
What information do I need to complete the form?
You need to provide detailed beneficiary information, including Social Security Number, and details about your Medicare coverage (if applicable) and any other health insurance coverage you have besides Medicare. This includes the insurance company's name, the effective and termination dates of your coverage, and whether your insurance includes prescription coverage.
Do I need to attach anything with the form?
Yes. If applicable, you should attach:
- A copy of your Medicare card.
- Copies of your OHI member ID card(s), front and back.
What happens if I fail to provide the requested information?
Failure to fill out the form completely or accurately can result in delays or denials of reimbursements from CHAMPVA until the correct OHI information is received. Ensuring all information provided is accurate and up to date is essential for the seamless processing of your healthcare benefits.
Where can I find more information about CHAMPVA benefits and eligibility?
For more detailed information about CHAMPVA and your benefits, you can visit the official VA website at www.va.gov/hac or call the CHAMPVA Help Line at 1-800-733-8387. These resources can provide guidance and help answer any further questions you may have about your coverage and the VA Form 10-7959c.
Common mistakes
-
One common error people make is failing to attach necessary documents, such as a copy of Medicare and other health insurance (OHI) member ID cards (front and back), when submitting the form. Without these documents, the Veterans Affairs (VA) Health Administration Center cannot verify the coverage information provided, leading to delays or denials in the processing of claims. Attachments are crucial for a comprehensive review and should include not just the ID cards but also any schedules of benefits that list co-payments, especially if the OHI does not issue Explanation of Benefits (EOBs).
-
Another mistake often encountered is incorrect or incomplete information in the beneficiary details section. This includes errors in personal information such as the Social Security Number, address, or contact details. Accuracy in filling out these fields is vital as it ensures the VA can communicate effectively with beneficiaries regarding their coverage status and any changes that may affect their benefits.
-
Not updating the VA Health Administration Center promptly when there is a change in insurance status is a significant oversight. The form is not only for initial submission but also for reporting any changes in OHI coverage. Fast response to changes in OHI status, such as new effective dates of coverage or termination of a policy, helps maintain accurate records, ensuring beneficiaries receive the correct benefits without lapse.
-
Lastly, some individuals overlook the certification section at the bottom of the form, failing to sign or date it. This oversight can be more pronounced with electronic submissions where typed signatures are acceptable. Regardless of the submission method, the certification by the beneficiary, sponsor, or legal guardian is a legal attestation that the information provided is accurate to the best of their knowledge. Failure to properly certify the form can result in delays or the need for resubmission.
Remember, the VA Form 10-7959c, is more than just paperwork; it's a crucial piece of communication between beneficiaries and the VA Health Administration Center. Ensuring its accurate and complete submission is key to maintaining uninterrupted coverage and benefits.
Documents used along the form
When dealing with the complexities of healthcare coverage for veterans and their families, several forms and documents play crucial roles alongside the VA Form 10-7959c, CHAMPVA Other Health Insurance (OHI) Certification. This certification is pivotal for individuals under the Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA), as it ensures that the program can coordinate benefits efficiently when other health insurances are in effect. Identifying and understanding ancillary documentation can streamline the process, ensuring that claims and coverage are handled promptly and accurately.
- VA Form 10-10EZ - Application for Health Benefits: This form is the starting point for veterans, service members, and their families to apply for medical benefits through the VA, setting the foundation for all subsequent healthcare-related interactions and claims.
- VA Form 10-10EZR - Health Benefits Update Form: Utilized for updating personal information such as marital status, dependents, insurance changes, or financial information. It is often submitted in conjunction with the VA Form 10-7959c when there are changes to health insurance coverage.
- Medicare Card - Indicates enrollment in Medicare Parts A, B, and D, essential for beneficiaries also covered under CHAMPVA, as it affects the coordination of benefits and which plan is considered primary or secondary coverage.
- Proof of Other Health Insurance - Copies of health insurance cards (front and back): Necessary to validate the existence of additional health coverage outside of CHAMPVA and Medicare, detailed in VA Form 10-7959c for proper benefits coordination.
- Explanation of Benefits (EOB) - A document from private insurance companies after receiving medical services that explains what treatments were covered and any payment responsibilities. CHAMPVA requires this to coordinate benefits effectively and determine what costs, if any, they will cover.
- VA Form 21-4142 - Authorization and Consent to Release Information to the Department of Veterans Affairs: Allows the VA to obtain medical records from private healthcare providers, crucial for processing claims and determining eligibility for CHAMPVA benefits.
- Prescription Drug Coverage Proof - Documents or cards showing prescription drug coverage under a separate plan, particularly if not covered under Medicare Part D, to inform CHAMPVA of all existing coverages for accurate benefits coordination.
Correctly utilizing and submitting these forms in conjunction with the VA Form 10-7959c is essential for the efficient management of CHAMPVA benefits. These documents help in establishing the beneficiary's eligibility, the extent of coverage under different plans, and ensuring that benefits are correctly coordinated between CHAMPVA and other health insurances. Prompt and accurate submission not only facilitates timely access to healthcare services but also maximizes the benefits available to veterans and their families, ultimately contributing to their health and well-being.
Similar forms
The VA Form 10-7959c, designed for CHAMPVA Other Health Insurance (OHI) Certification, shares similarities with other forms and documents that are utilized within healthcare and insurance sectors. These documents, while unique in their specific purpose, echo the shared goal of ensuring accurate insurance information and coverage details for beneficiaries. The forms similar to the VA Form 10-7959c typically serve to collect or update personal insurance information, verify coverage status, or assist in the coordination of benefits among various health insurance providers.
- Medicare Enrollment Application (CMS-855I) - This form is similar as it collects detailed personal and insurance information, specifically from individuals applying for enrollment or changing their Medicare status. Both forms share the purpose of maintaining current records to ensure proper health coverage.
- Health Insurance Claim Form (CMS-1500) - Utilized by healthcare providers to bill Medicare and other health insurance companies, it overlaps with VA Form 10-7959c in its use for insurance claims processing. Both require detailed insurance information to facilitate benefits and reimbursements.
- Medicaid Application Form - Similar to the VA form in that it gathers extensive personal and insurance details for individuals seeking Medicaid benefits. Both documents play a crucial role in determining eligibility and coordinating secondary insurance benefits.
- Private Health Insurance Application Forms - Private insurers utilize these forms to collect applicants' health, personal, and existing insurance information, much like the VA form. Their core similarity lies in ensuring that all pertinent coverage information is up-to-date for policy administration.
- Employment-Based Health Benefits Enrollment Forms - Similar to VA Form 10-7959c, these forms are used by employees to provide or update their health insurance information through employers, often including details about other existing health insurance coverage.
- State Children's Health Insurance Program (SCHIP) Application Forms - These forms, designed for state-specific health programs for children, require comprehensive family income and insurance information, reflecting the VA form's emphasis on current and accurate health coverage details.
- Explanation of Benefits (EOB) Forms - Although primarily a statement rather than an application form, EOBs are closely connected to the VA Form 10-7959c as they provide detailed accounts of insurance claims processed, which is crucial for the management of supplemental insurance like CHAMPVA.
- TRICARE Enrollment Forms - Used for enrolling in the TRICARE health program for military personnel and their families, these forms, like the VA Form 10-7959c, require detailed other health insurance information to prevent overpayment and coordinate benefits effectively.
Each document, while intended for different programs or purposes, fundamentally seeks to capture accurate insurance information to ensure that benefits are correctly coordinated and provided, mirroring the goal of the VA Form 10-7959c in assisting beneficiaries with their CHAMPVA eligibility and coverage details.
Dos and Don'ts
When completing the VA Form 10-7959C, CHAMPVA Other Health Insurance (OHI) Certification, individuals should take certain steps and avoid others to ensure accurate processing of their form. Below are essential do's and don'ts to follow:
- Do thoroughly read the instructions and information on the back of the form before starting.
- Do use black or blue ink if filling out the form by hand to ensure readability.
- Do complete all applicable sections accurately to prevent delays or denials in benefits.
- Do attach copies of your Medicare card and any other health insurance member ID cards (front and back), as required.
- Do include copies of explanation of benefits (EOBs) or your co-payment schedule if your OHI does not issue EOBs.
- Do provide detailed information about all periods of other health insurance coverage since you became eligible for CHAMPVA.
- Do promptly notify the VA Health Administration Center of any changes in your insurance status.
- Do ensure that your signature and the date are on the form before submission.
- Don't leave any required fields blank; incomplete information can lead to processing delays or denial of reimbursement.
- Don't send original documents unless specifically requested; always send copies.
Adhering to these guidelines ensures that your VA Form 10-7959C is filled out completely and accurately, facilitating a smoother processing experience. It's important to keep in mind that providing false information can lead to criminal penalties. In case of doubts or questions, it's advisable to contact the VA Health Administration Center directly for assistance.
Misconceptions
Understanding the CHAMPVA Other Health Insurance (OHI) Certification form, VA Form 10-7959C, can be complex. Misconceptions about this form can lead to confusion and potential delays in reimbursement or coverage. Here are four common misconceptions explained:
Myth 1: Submission of VA Form 10-7959C is only for new CHAMPVA beneficiaries. In reality, both new and existing beneficiaries need to submit this form not only at the beginning of their CHAMPVA coverage but also any time there is a change in their other health insurance status. This ensures that the CHAMPVA program has current information to accurately coordinate benefits.
Myth 2: If you don't have Other Health Insurance (OHI), you don't need to fill out this form. While it might seem unnecessary to submit a form confirming the absence of other coverage, it is actually required. For those without any other health insurance, completing the form helps verify their status and ensures that CHAMPVA can process claims without delay, looking for other potential primary coverages.
Myth 3: The form is only necessary for prescription coverage. This misconception overlooks the comprehensive nature of the form. It is designed to gather information about all types of health insurance coverage you have that is not CHAMPVA, including Medicare, private health insurance, and Medicaid, among others. This information is crucial for CHAMPVA to determine how it will coordinate benefits, not just for prescription drugs but for all covered services.
Myth 4: Once you complete the form, you don't have to worry about it again. Keeping your information updated is crucial. Beneficiaries are required to inform CHAMPVA of any changes in their other health insurance status as soon as they occur. Failure to do so can result in delayed reimbursement or denial of benefits, highlighting the importance of promptly submitting an updated VA Form 10-7959C whenever there is a change in your other health insurance coverage.
In conclusion, accurately completing and updating the VA Form 10-7959C is crucial for the processing of CHAMPVA benefits. Understanding these common misconceptions helps ensure that beneficiaries take the necessary steps to maintain their coverage and receive the benefits to which they are entitled without unnecessary interruption.
Key takeaways
- When filling out the VA Form 10-7959c, it is crucial to provide all requested information accurately to avoid delays or denial of benefits. This form is essential for individuals receiving the Civilian Health and Medical Program of the Department of Veterans Affairs (CHAMPVA) benefits who have other health insurance (OHI).
- Updating your insurance information is necessary whenever there are changes to your OHI coverage. This includes adding new policies or reporting changes in existing ones. The form must be submitted for each family member separately if they are also beneficiaries.
- Medicare beneficiaries are required to attach a copy of their Medicare card with the VA Form 10-7959c. This helps in identifying Part A, B, and D coverage and ensures that your records are updated accurately.
- For those with insurance policies other than Medicare, including details of the insurance like carrier name, effective date, and whether the policy includes prescription coverage, is necessary. This information helps in managing how CHAMPVA benefits coordinate with your OHI.
- If your OHI changes, promptly notifying the VA's Health Administration Center is crucial. This prompt notification ensures that your CHAMPVA benefits are correctly managed and any reimbursement issues can be avoided.
- Completing the certification section at the end of the form is mandatory. By signing this section, you are confirming that the information provided is accurate to the best of your knowledge. This step is crucial for the processing of your form.
- It is important to remember that failing to furnish the requested information might not only delay the processing of your benefits but could result in a denial of your request for CHAMPVA benefits. It’s important to review all sections carefully and ensure completeness before submission.
- Submission of this form can be done electronically or via fax, making it convenient to provide updates or changes in your OHI status promptly. Always keep a copy of the completed form for your records.
Popular PDF Forms
Split Sheet - Allows songwriters to officially register their contributions and related details with performance societies, such as ASCAP or BMI.
Bill of Sale Dmv Pdf - Apart from serving as a purchase record, this document can play a critical role in disputes or insurance claims related to the sold item.
Da Form 3439 - Job knowledge, managerial skills, and supervision capabilities can be marked if applicable to the applicant's desired position.