Blank Vital Signs Flow Sheet PDF Template
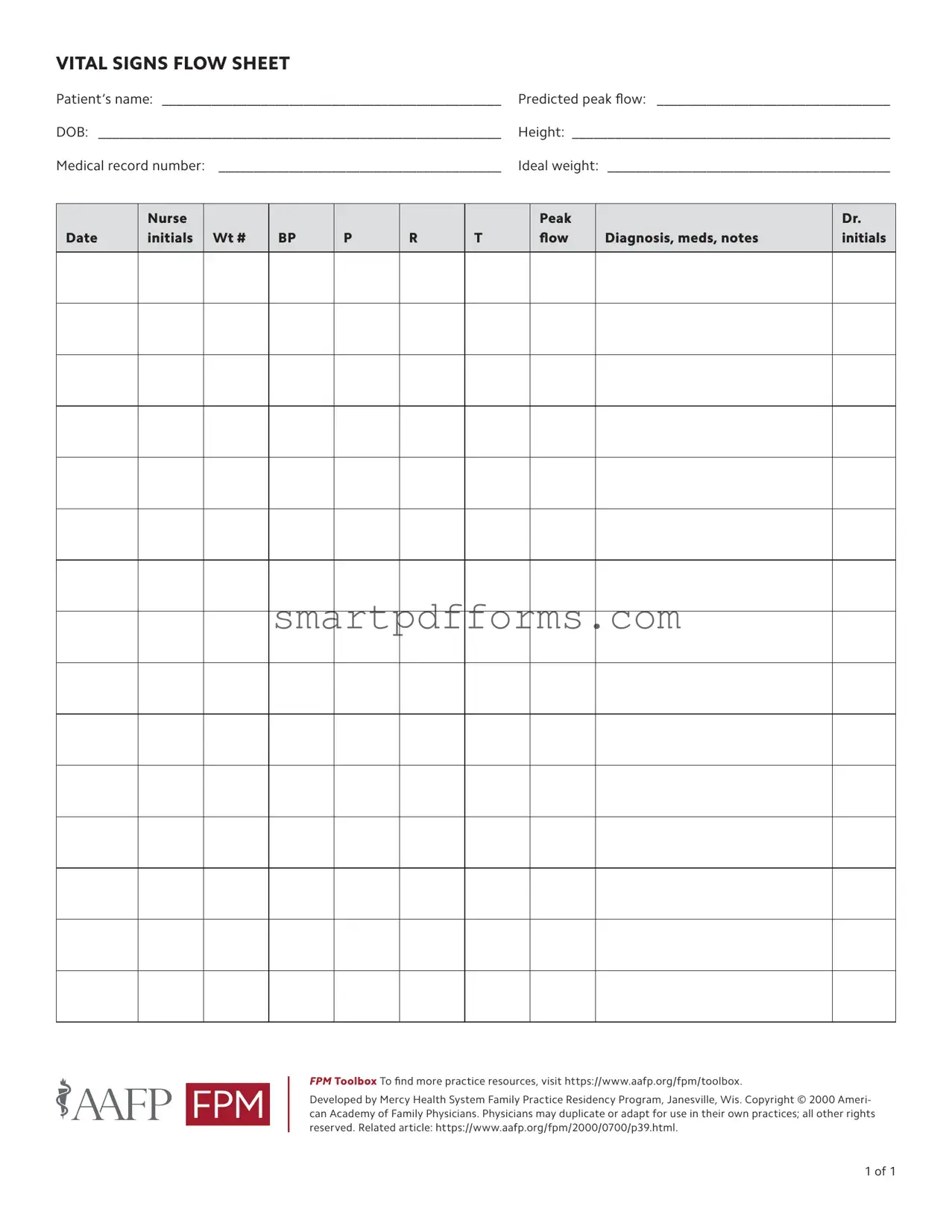
At the heart of patient care, especially within the domains of internal medicine and family practice, lies the critical document known as the Vital Signs Flow Sheet. This form serves as a comprehensive record, meticulously tracking a patient's vital signs across various time points, thereby offering healthcare providers a detailed view of the patient’s health status over time. It includes essential information such as the patient's name, date of birth (DOB), medical record number, predicted peak flow, height, and ideal weight, together paving the way for a personalized approach to healthcare. The form allows for the recording of vital signs such as weight, blood pressure (BP), pulse (P), respiration rate (R), temperature (T), and peak flow readings—a crucial measure for those with respiratory issues. Additionally, it provides space for documenting diagnoses, medications, and any pertinent notes, essential for ensuring a holistic understanding of a patient's health journey. Created by the Mercy Health System Family Practice Residency Program in collaboration with the American Academy of Family Physicians, this tool emphasizes the importance of continuous monitoring and is adaptable for use in various medical practices. It underscores the meticulous attention healthcare professionals must pay to tracking and interpreting these fundamental health indicators, making it an indispensable part of patient care management.
Preview - Vital Signs Flow Sheet Form
VITAL SIGNS FLOW SHEET
Patient’s name: _________________________________________________ |
Predicted peak flow: __________________________________ |
DOB: __________________________________________________________ |
Height: _____________________________________________ |
Medical record number: _ ________________________________________ |
Ideal weight: _________________________________________ |
Date
Nurse initials
Wt #
BP
P
R
T
Peak flow
Diagnosis, meds, notes
Dr. initials
FPM Toolbox To find more practice resources, visit https://www.aafp.org/fpm/toolbox.
Developed by Mercy Health System Family Practice Residency Program, Janesville, Wis. Copyright © 2000 Ameri- can Academy of Family Physicians. Physicians may duplicate or adapt for use in their own practices; all other rights reserved. Related article: https://www.aafp.org/fpm/2000/0700/p39.html.
1 of 1
Form Data
| Fact | Description |
|---|---|
| Usage Purpose | The Vital Signs Flow Sheet is designed for continuous monitoring and recording of a patient's vital signs including weight, blood pressure, pulse, temperature, and peak flow. |
| Accessibility | Developed by Mercy Health System Family Practice Residency Program and copyrighted by the American Academy of Family Physicians, it is accessible for physicians to duplicate or adapt for use in their own practices. |
| Key Features | Includes fields for patient information, doctor and nurse initials, and sections for recording diagnosis, medications, and notes for each date of entry. |
| Intended Users | Though developed by a specific health system, it's made for use by physicians and healthcare professionals across various medical settings for patient care management. |
| Governing Law and Usage Rights | While the form itself is not governed by a specific law, its usage is protected under copyright law as stated by the American Academy of Family Physicians. Only physicians and healthcare providers are granted the right to duplicate or adapt the form for their practices; all other rights are reserved. |
Instructions on Utilizing Vital Signs Flow Sheet
Completing a Vital Signs Flow Sheet is important in monitoring a patient's critical health parameters over a period. This form helps in keeping track of various vital signs including weight, blood pressure (BP), pulse (P), respiration rate (R), temperature (T), and peak flow values. Additionally, it allows the recording of diagnoses, medications, notes, and doctor's initials, providing a comprehensive view of the patient's health status at each visit. Below are the steps necessary for accurately filling out the form.
- Start by entering the Patient’s name on the designated line.
- Fill in the DOB (Date of Birth) next to the patient’s name.
- Enter the Medical record number of the patient.
- Next, input the Predicted peak flow, if available, to help monitor the patient's lung function.
- Fill in the Height of the patient, which is necessary for assessing the predicted peak flow correctly.
- Document the Ideal weight of the patient to assist in evaluating nutritional and health status.
- Under the Date column, input the date when the vital signs are being measured.
- In the Nurse initials section, the nurse measuring the vital signs should put their initials as a record of who conducted the evaluation.
- Enter the patient’s Weight (Wt) on the day of the assessment.
- Document the Blood Pressure (BP) reading.
- Record the Pulse (P) rate, noting the beats per minute.
- Fill in the Respiration (R) rate, measuring breaths per minute.
- Note the Temperature (T) in the appropriate scale (Celsius or Fahrenheit).
- If a peak flow meter is used, document the Peak flow value obtained.
- In the section marked for Diagnosis, meds, notes, detail any relevant medical diagnoses, prescribed medications, and additional notes that could inform care.
- Lastly, ensure that the doctor who reviews the form or provides the diagnosis enters their Initials in the designated Dr. initials space.
After completing the Vital Signs Flow Sheet, the form should be reviewed for accuracy. Every recorded piece of information plays a critical role in providing the patient with the best possible care. It's important to ensure that all entries are readable and correct, reflecting the patient's current health status. This detailed record-keeping is essential for ongoing health monitoring and plays a critical role in medical care. The form, once filled out, becomes an integral part of the patient's medical record, used to make informed decisions about their health management.
Obtain Answers on Vital Signs Flow Sheet
What is the purpose of the Vital Signs Flow Sheet form?
The Vital Signs Flow Sheet form is designed to help healthcare providers efficiently track a patient's vital signs over time. This includes their weight, blood pressure, pulse, respiratory rate, temperature, and peak flow. By documenting these metrics regularly, the form allows for easy visualization of trends or changes in a patient's health, enabling timely interventions and adjustments to treatment plans. It's a crucial tool in monitoring the ongoing health of patients, particularly those with chronic conditions or those undergoing specific treatments.
How should the information on the Vital Signs Flow Sheet be filled out?
When completing the Vital Signs Flow Sheet, it's important to accurately and clearly record the patient's vital signs as per each visit or check-up. Start by filling in the patient's name, date of birth (DOB), medical record number, predicted peak flow, height, and ideal weight at the top of the form. On each subsequent visit, the nurse should record the date, their initials, the patient's weight (Wt), blood pressure (BP), pulse (P), respiratory rate (R), temperature (T), and peak flow readings. Any pertinent diagnosis, medications, or notes can be added in the designated area, along with the doctor's initials. This ensures a comprehensive and up-to-date record of the patient's health status.
Who can access and use the information on the Vital Signs Flow Sheet?
The information on the Vital Signs Flow Sheet is primarily for the use of healthcare professionals involved in the patient's care. This includes nurses, doctors, and specialists who are part of the patient's healthcare team. They use this information to make informed decisions about the patient's treatment and care plan. While the sheet is a professional document, patients have the right to access their own health information under the Health Insurance Portability and Accountability Act (HIPAA). They can request to view or obtain copies of their Vital Signs Flow Sheet to better understand their health status and treatment.
Can the Vital Signs Flow Sheet be modified or adapted for use?
Yes, the Vital Signs Flow Sheet can be duplicated or adapted for use in individual practices, as stated by its copyright notice provided by the American Academy of Family Physicians. This flexibility allows healthcare providers to possibly adjust or add sections to the form to better suit their practice's needs or specific patient requirements. However, it is important to note that any modifications should maintain the form's integrity as a tool for accurately tracking patient health data over time.
Where can more resources related to the use of the Vital Signs Flow Sheet be found?
More resources related to the use of the Vital Signs Flow Sheet, including best practices and guidelines, can be found on the American Academy of Family Physicians website. Specifically, healthcare providers can visit the provided link (https://www.aafp.org/fpm/toolbox) to access a toolbox of practice resources. Additionally, related articles, such as the one linked at https://www.aafp.org/fpm/2000/0700/p39.html, offer insights into maximizing the effectiveness of the Vital Signs Flow Sheet in patient care.
Common mistakes
When filling out the Vital Signs Flow Sheet, it's crucial to provide accurate and complete information to ensure proper monitoring and management of the patient's health status. Unfortunately, individuals often make mistakes in this process, which can lead to less effective care. Here are ten common errors:
Incomplete patient information: Forgetting to fill in sections such as the patient's name, date of birth (DOB), and medical record number can result in confusion and potential mix-ups with other patient records.
Not updating height and weight: Failing to regularly update this vital information can impact the accuracy of medical assessments, as changes can indicate shifts in health status.
Incorrect or outdated predicted peak flow values can lead to misunderstandings regarding a patient's respiratory status and the efficacy of treatments.
Misrecording vital signs: Errors in documenting vital signs, such as blood pressure (BP), pulse (P), respiration (R), temperature (T), and peak flow, can lead to inaccurate diagnoses or treatment plans.
Overlooking the Date and Nurse initials section: Neglecting to record the date and the nurse's initials can create issues in tracking the progress or changes in the patient's condition over time.
Failure to detail diagnosis, medications, and notes: Neglecting to include or update this information can hinder communication between healthcare providers and compromise patient care.
Lack of doctor's initials may lead to questions about the verification of the recorded information and its integration into the patient’s care plan.
Illegible handwriting: If healthcare providers cannot read the information, misunderstandings and errors in patient care can occur.
Using incorrect units of measurement for weight, height, or peak flow can lead to misinterpretation of the data and potentially to improper treatment strategies.
Forgetting to reference or adhere to the guidelines suggested in links provided by the precedent documentation, such as those found at the American Academy of Family Physicians (AAFP) website, can result in missing out on updated standards or practices in patient care management.
For a healthcare provider, taking the time to carefully and accurately complete the Vital Signs Flow Sheet is essential. It ensures that all members of the healthcare team have the data they need to offer the best care possible. Avoiding these common mistakes plays a critical role in enhancing patient outcomes.
Documents used along the form
In the realm of healthcare, accurately monitoring and maintaining patient records is pivotal for ensuring effective treatment and care. Among these records, the Vital Signs Flow Sheet form is a fundamental tool. It meticulously tracks a patient's vital signs, like blood pressure, pulse, temperature, and respiratory rate, providing a clear chronological perspective of the patient's health status. Yet, to weave together a comprehensive patient narrative, healthcare providers often supplement this form with additional documents, each serving its unique purpose in patient care management. Let’s explore some of these critical documents.
- Medication Administration Record (MAR): This document tracks all the medications prescribed to a patient, including the dosage, time, and method of administration. It's essential for managing the patient’s medication schedule and ensuring adherence to treatment plans.
- Patient Admission Form: Includes vital information collected during the admission process—such as medical history, allergies, and current medications—which is crucial for initial assessment and ongoing care.
- Medical History Form: Provides a detailed account of the patient’s past medical history, surgeries, illnesses, and family health history, helping doctors to make informed decisions regarding the patient’s treatment.
- Consent Forms: Legal documents that patients sign to acknowledge the receipt of information regarding their procedures and treatments and to grant permission for those procedures and treatments to be performed.
- Treatment Plan Form: Outlines the plan of care designed for the patient, including goals, type of treatments, and expected outcomes. It keeps both the patient and healthcare team focused on the objectives of care.
- Progress Notes: Written by healthcare professionals to document a patient's clinical status during a hospital stay or out-patient visit. These notes include observations, treatments administered, and the patient's response to treatment.
- Laboratory Test Orders and Results: Critical for diagnosing and monitoring conditions. These documents include orders for blood tests, imaging studies, and other exams, along with their results.
- Discharge Summary: A comprehensive summary prepared at the end of a hospital stay or treatment course, detailing the patient’s diagnosis, treatments received, response to treatment, and follow-up instructions.
- Advance Directive Form: A legal document where patients can specify their wishes regarding medical treatment and life-sustaining measures in the event they are unable to communicate their decisions in the future.
Each of these documents plays a vital role in painting a complete picture of a patient's health journey alongside the Vital Signs Flow Sheet. They work in tandem to ensure that every healthcare provider involved in a patient's care has access to thorough and accurate information, facilitating better communication, more accurate diagnoses, and more effective treatment plans. Taken together, these forms and documents create a comprehensive framework that supports the delivery of high-quality healthcare.
Similar forms
Medication Administration Record (MAR): Similar to the Vital Signs Flow Sheet, a MAR tracks a patient's medication schedules, including dosages and times administered. It ensures medication accuracy and safety, much like the Vital Signs Flow Sheet monitors critical physiological parameters over time.
Patient Intake Form: This document collects initial patient information, such as name, date of birth, medical history, and presenting symptoms, akin to the demographic and baseline health data at the top of the Vital Signs Flow Sheet.
Treatment Plan: A Treatment Plan outlines a patient’s diagnosis, goals, and strategies for therapy or intervention. It resembles the section of the Vital Signs Flow Sheet that records diagnoses, medications, and notes, providing a structured approach to healthcare.
Progress Notes: These are detailed records of a patient's clinical status, therapeutic interventions, and progress over time. The way progress notes document ongoing patient care mirrors the Vital Signs Flow Sheet’s tracking of vital signs and treatments across multiple dates.
Immunization Record: This log tracks a patient’s vaccinations over time. While its focus is different, the structure for recording a specific aspect of patient care over various intervals is similar to the method used in the Vital Signs Flow Sheet for monitoring vitals.
Nutritional Assessment Form: Used to evaluate a patient's dietary habits and nutritional status, this form often includes measurements similar to those found in the Vital Signs Flow Sheet, such as weight and height. Both forms contribute to a comprehensive understanding of a patient's health.
Emergency Contact Form: Though primarily for contact information, this form also has sections that can include important health information, reminiscent of the Vital Signs Flow Sheet’s gathering of essential patient data for reference in critical situations.
Dos and Don'ts
When completing the Vital Signs Flow Sheet, accuracy and thoroughness are essential for ensuring effective patient monitoring and care coordination. Below are crucial dos and don'ts to follow:
- Do ensure all patient information is accurate and fully filled out, including the patient’s name, date of birth (DOB), medical record number, height, and ideal weight. This foundational data is critical for personalized care.
- Do verify the predicted peak flow value is entered correctly, as it is vital for assessing respiratory function, especially for patients with asthma or other respiratory issues.
- Do routinely update the weight (Wt), blood pressure (BP), pulse (P), respiration (R), temperature (T), and peak flow readings to keep track of the patient's vital signs over time, offering a comprehensive view of their health status.
- Don’t leave any fields blank. If a measurement is not applicable or available at the time of documentation, indicate this clearly with a notation such as “N/A” to avoid any potential confusion or misinterpretation.
- Don’t forget to include nurse and doctor's initials next to the respective entries to ensure accountability and facilitate clear communication among healthcare providers.
- Don’t overlook adding any relevant diagnostic findings, medications, or notes in the designated area. This section enriches the flow sheet with critical clinical information, enabling a holistic view of the patient's care journey.
Treating the Vital Signs Flow Sheet with diligence not only enhances patient care but also supports medical providers in delivering optimized treatment strategies. For further resources or templates, the American Academy of Family Physicians (AAFP) website serves as a comprehensive guide.
Misconceptions
Understanding the Vital Signs Flow Sheet form is important for both healthcare professionals and patients. However, there are several misconceptions about it that need to be addressed:
- Misconception 1: The form is only for doctors' use.
- Misconception 2: Only the patient’s current vital signs matter.
- Misconception 3: The form is comprehensive in assessing a patient's health.
- Misconception 4: All sections of the form must be filled out for every patient.
While it's true that healthcare professionals primarily use the Vital Signs Flow Sheet to monitor and record a patient's vital statistics over time, it's also important for patients and caregivers. Being informed about the details on the form can empower individuals to understand their health status better and facilitate more informed discussions with their healthcare providers.
This form does more than just record a single instance of vital signs. It tracks these over time, providing a clear picture of the patient's health trends. This long-term data is crucial for making accurate diagnoses and tailoring treatment plans to the patient's specific needs.
Although the Vital Signs Flow Sheet is a valuable tool for monitoring key indicators of a patient’s health, such as blood pressure, pulse, and temperature, it doesn't capture the full spectrum of health assessments. Other diagnostic tools and evaluations are often necessary to get a complete understanding of a patient's health status.
While most of the details on the form are essential for effective monitoring, some sections may not apply to every patient. Healthcare providers use their judgment to determine which parts of the form are relevant to each patient's care, based on their individual health needs and circumstances.
Clearing up these misconceptions can lead to a better understanding of the Vital Signs Flow Sheet form's purpose and use, ultimately enhancing the quality of care provided to patients.
Key takeaways
When it comes to managing one's health, accurately filling out and utilizing the Vital Signs Flow Sheet is crucial. This document, developed by the Mercy Health System Family Practice Residency Program and endorsed by the American Academy of Family Physicians, helps both patients and healthcare providers track vital health metrics over time. Below are four key takeaways to ensure this form is used effectively:
- Complete all patient information accurately: The top section of the Vital Signs Flow Sheet requires detailed patient information, including name, date of birth (DOB), predicted peak flow, height, ideal weight, and medical record number. Ensuring this information is filled out accurately is vital for personalized patient care and for tracking health trends over time.
- Regular documentation is essential: The form is designed to record vital signs such as weight (Wt), blood pressure (BP), pulse (P), respiration (R), temperature (T), and peak flow readings. These should be updated regularly to monitor the patient's health status, detect any abnormalities early, and adjust care plans accordingly.
- Medication and notes section is critical for comprehensive care: There is a designated area to document diagnosis, medications, notes, and doctor's initials. This section is crucial for providing a holistic view of the patient's health care plan, including any changes in medication or treatment strategies, making it easier for all healthcare providers involved to stay informed.
- Use the form as a communication tool: Besides monitoring vital signs, the Vital Signs Flow Sheet serves as an important communication tool among healthcare professionals. Regularly updated forms ensure that every member of the healthcare team is aware of the patient's current condition, facilitating coordinated care and decision-making.
Remember, this form is not just a record but a tool that aids in the effective management of a patient's health. Its proper use is pivotal in early detection of potential health issues, ensuring that accurate and timely interventions can be made.
Popular PDF Forms
Motion for Contempt Colorado - Acts as a formal request for judicial oversight in instances where court orders are disregarded in Colorado.
State of Georgia Workers Compensation - Demonstrates an employer's commitment to accommodating workers' limitations while adhering to legal standards.