Blank Cms 460 PDF Template
In the landscape of healthcare administration and Medicare services, the CMS-460 form plays a pivotal role by establishing a framework within which physicians, practitioners, and suppliers agree to accept Medicare assignment for all covered services. This agreement means that those professionals will request direct payment from Medicare for services provided, adhering to rates approved by the Medicare Administrative Contractor (MAC)/carrier as the full charge. The agreement highlights not only the act of entering into a partnership with the Medicare program but also delineates the obligations related to billing, specifically that participants cannot charge beneficiaries more than the applicable deductible and coinsurance for covered services. It is set to take effect once filed during the enrollment period, with a renewal process that prompts consideration at the close of each calendar year. Additionally, the agreement outlines conditions under which it can be ended, either by the participant through a notice to the MAC/carrier or by the Centers for Medicare & Medicaid Services (CMS) if the participant is found in substantial violation of the agreement's terms. This form is crucial for providers who decide to participate in Medicare, as it affects billing procedures and the financial relationship between providers, beneficiaries, and the Medicare program itself. Furthermore, the document guides on how to engage with or withdraw from Medicare participation status, elaborating on the rights and responsibilities bestowed upon participating members, and underscores the importance of understanding the consequences of opting out. As the form must be submitted to the appropriate MAC/carrier and not directly to CMS, knowing the procedural aspects of the CMS-460 form is essential for healthcare providers looking to navigate the Medicare system effectively.
Preview - Cms 460 Form
|
FORM APPROVED |
||
DEPARTMENT OF HEALTH AND HUMAN SERVICES |
OMB NO. |
||
EXPIRES 10/31/2022 |
|||
CENTERS FOR MEDICARE & MEDICAID SERVICES |
|||
|
|
||
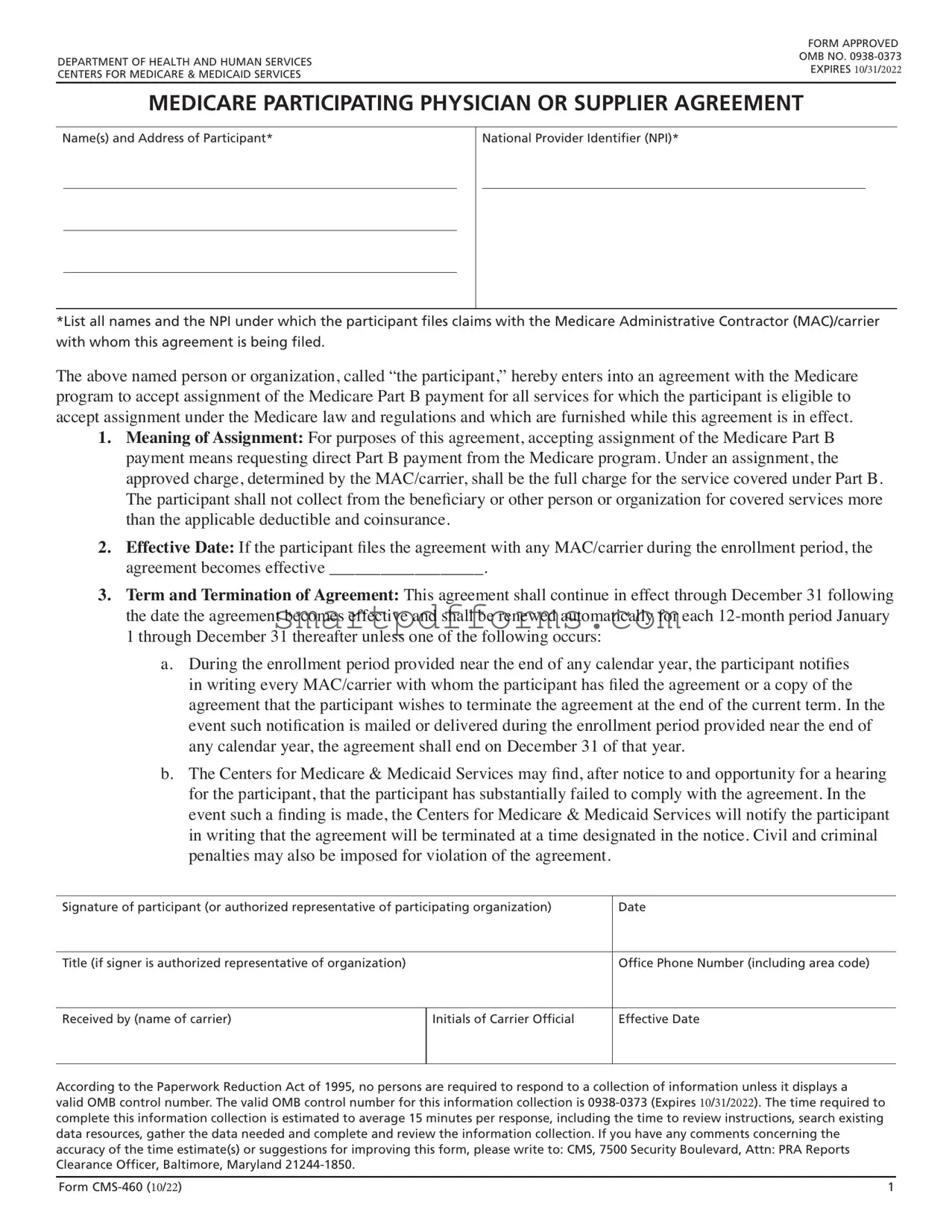
MEDICARE PARTICIPATING PHYSICIAN OR SUPPLIER AGREEMENT
Name(s) and Address of Participant*
National Provider Identifier (NPI)*
*List all names and the NPI under which the participant files claims with the Medicare Administrative Contractor (MAC)/carrier with whom this agreement is being filed.
The above named person or organization, called “the participant,” hereby enters into an agreement with the Medicare program to accept assignment of the Medicare Part B payment for all services for which the participant is eligible to accept assignment under the Medicare law and regulations and which are furnished while this agreement is in effect.
1.Meaning of Assignment: For purposes of this agreement, accepting assignment of the Medicare Part B payment means requesting direct Part B payment from the Medicare program. Under an assignment, the
approved charge, determined by the MAC/carrier, shall be the full charge for the service covered under Part B.
The participant shall not collect from the beneficiary or other person or organization for covered services more than the applicable deductible and coinsurance.
2.Effective Date: If the participant files the agreement with any MAC/carrier during the enrollment period, the agreement becomes effective __________________.
3.Term and Termination of Agreement: This agreement shall continue in effect through December 31 following the date the agreement becomes effective and shall be renewed automatically for each
1 through December 31 thereafter unless one of the following occurs:
a.During the enrollment period provided near the end of any calendar year, the participant notifies in writing every MAC/carrier with whom the participant has filed the agreement or a copy of the
agreement that the participant wishes to terminate the agreement at the end of the current term. In the event such notification is mailed or delivered during the enrollment period provided near the end of any calendar year, the agreement shall end on December 31 of that year.
b.The Centers for Medicare & Medicaid Services may find, after notice to and opportunity for a hearing
for the participant, that the participant has substantially failed to comply with the agreement. In the event such a finding is made, the Centers for Medicare & Medicaid Services will notify the participant in writing that the agreement will be terminated at a time designated in the notice. Civil and criminal penalties may also be imposed for violation of the agreement.
Signature of participant (or authorized representative of participating organization)
Date
Title (if signer is authorized representative of organization)
Office Phone Number (including area code)
Received by (name of carrier)
Initials of Carrier Official
Effective Date
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a
valid OMB control number. The valid OMB control number for this information collection is
Form |
1 |

DEPARTMENT OF HEALTH AND HUMAN SERVICES
CENTERS FOR MEDICARE & MEDICAID SERVICES
INSTRUCTIONS FOR THE MEDICARE PARTICIPATING PHYSICIAN
AND SUPPLIER AGREEMENT
To sign a participation agreement is to agree to accept assignment for all covered services that you provide to Medicare patients.
WHY PARTICIPATE?
If you bill for physicians’ professional services, services and supplies provided incident to physicians’ professional services, outpatient physical and occupational therapy services, diagnostic tests, or radiology services, your Medicare fee schedule amounts are 5 percent higher if you participate. Also, providers receive direct and timely reimbursement from Medicare.
Regardless of the Medicare Part B services for which you are billing, participants have “one stop” billing for beneficiaries who have Medigap coverage not connected with their employment and who assign both their Medicare and Medigap payments to participants. After we have made payment, Medicare will send the claim on to the Medigap insurer for payment of all coinsurance and deductible amounts due under the Medigap policy. The Medigap insurer must pay the participant directly.
Currently, the large majority of physicians, practitioners and suppliers are billing under Medicare participation agreements.
DO YOU WANT TO OPT OUT OF MEDICARE?
Certain physicians and practitioners who do not want to engage with the Medicare program when treating Medicare beneficiaries may choose to “opt out” of Medicare. While Medicare does not pay for covered items or services provided by an
WARNING: YOU CANNOT USE THIS FORM TO OPT OUT!
WHEN THE DECISION TO PARTICIPATE CAN BE MADE:
•Toward the end of each calendar year, all MAC/carriers have an open enrollment period. The open enrollment period generally is from
Form |
2 |
•New physicians, practitioners, and suppliers can sign the participation agreement and become a Medicare participant at the time of their enrollment into the Medicare Program. The participation agreement will become effective on the date of filing; i.e., the date the participant mails
Contact your MAC/carrier to get the exact dates the participation agreement will be accepted, and to learn where to send the agreement.
WHAT TO DO DURING OPEN ENROLLMENT:
If you choose to be a participant:
•Do nothing if you are currently participating, or
•If you are not currently a Medicare participant, complete the blank agreement
If you decide not to participate:
•Do nothing if you are currently not participating, or
•If you are currently a participant, write to each carrier to which you submit claims, advising of your termination effective the first day of the next calendar year. This written notice must be postmarked prior to the end of the current calendar year.
WHAT TO DO IF YOU’RE A NEW PHYSICIAN, PRACTITIONER OR SUPPLIER:
If you choose to be a participant:
•Complete the blank agreement
•If you have already enrolled in the Medicare program, you have 90 days from when you are enrolled to decide if you want to participate. If you decide to participate within this
If you decide not to participate:
•Do nothing. All new physicians, practitioners, and suppliers that are newly enrolled are automatically
We hope you will decide to be a Medicare participant.
Please call the MAC/carrier in your jurisdiction if you have any questions or need further information on participation.
DO NOT SEND YOUR
To view updates and the latest information about Medicare, or to obtain telephone numbers of the various Medicare Administrative Contractor (MAC)/carrier contacts including the MAC/carrier medical directors, please visit the CMS web site at http://www.cms.gov/.
Form |
3 |
Form Data
| Fact Name | Detail |
|---|---|
| Purpose of Form CMS-460 | This form is an agreement for physicians or suppliers to accept assignment for all covered services under Medicare Part B, ensuring direct and timely reimbursement. |
| Effective Date and Duration | The agreement becomes effective upon filing with a Medicare Administrative Contractor (MAC) during the enrollment period and auto-renews annually, subject to termination conditions. |
| Condition for Termination | The agreement may be terminated if the participant notifies every MAC/carrier during the enrollment period, or CMS finds the participant has substantially failed to comply with the agreement. |
| Benefits of Participating | Participants receive a 5% higher Medicare fee schedule amount for services, direct reimbursement from Medicare, and streamlined billing for beneficiaries with Medigap coverage. |
Instructions on Utilizing Cms 460
Before commencing the process of filling out the CMS-460 form, it's important to understand that this step signifies your agreement to accept assignment for all covered services provided to Medicare patients. Filling out this form accurately and timely ensures that you receive direct and increased reimbursements for services rendered and allows for simplified billing processes, especially for patients with Medigap coverage. Below are the precise steps needed to complete this form. Note that this endeavor is crucial for your practice if you intend to participate in the Medicare program fully.
- Start by providing the Name(s) and Address of the participant in the designated field. Ensure that all names under which the participant files Medicare claims are listed.
- Enter the National Provider Identifier (NPI) accurately. This identifier is crucial as it is used across the Medicare and Medicaid programs to identify health care providers in standard transactions.
- Read the section titled "Meaning of Assignment" thoroughly to understand what accepting assignment for Medicare Part B payment entails. This section defines the agreement's scope, including how the approved charge determined by your MAC/carrier is the full charge for the covered services under Part B.
- In the Effective Date blank, the date your agreement becomes effective will be filled out by the MAC/carrier once they process your form, based on when it is filed during the enrollment period.
- Review the Term and Termination of Agreement section to understand the duration of your agreement with Medicare, how it automatically renews, and under what conditions it can be terminated.
- Provide the required signature at the bottom of the form. If you're signing on behalf of a participating organization, include your title next to your signature.
- Enter your Office Phone Number, including the area code. This information is essential for any necessary follow-up or clarification.
- Upon submitting the form to your MAC/carrier, the Received by section, including the name of the carrier and the initials of the carrier official, along with the Effective Date, will be completed by the carrier itself.
After filling out and submitting your CMS-460 form, it will be processed by your Medicare Administrative Contractor (MAC)/carrier. This submission officially enrolls you as a participating provider, which entails agreeing to accept assignment for all Medicare-covered services. Remember, this agreement enhances your reimbursement rates and streamlines billing processes for Medigap beneficiaries. Be sure to keep a copy of the completed form for your records and await confirmation from your MAC/carrier of your effective participation date. It's imperative to stay informed about the participation window each year to maintain your status or make any necessary changes to your participation agreement.
Obtain Answers on Cms 460
-
What is a CMS-460 form and who needs to fill it out?
The CMS-460 form is a Medicare Participating Physician or Supplier Agreement. This form is used by physicians, practitioners, and suppliers to indicate that they agree to accept assignment for all Medicare-covered services they provide. Accepting assignment means they agree to request direct Part B payment from the Medicare program and not to charge more than the Medicare deductible and coinsurance amounts for covered services. It is intended for those currently enrolled in the Medicare Program or newly enrolling who wish to be identified as participating providers.
-
When can a physician or supplier decide to participate in Medicare?
Decision-making regarding participation in Medicare is specific to certain times of the year. Toward the end of each calendar year, an open enrollment period is held, generally from mid-November through December 31. During this window, enrolled providers have the opportunity to change their participation status effective January 1 of the following year. New physicians, practitioners, and suppliers can decide to participate at the time of their enrollment into Medicare, with a 90-day period to confirm their decision to participate after their enrollment is effective.
-
How is the CMS-460 form submitted?
If you decide to participate in Medicare, you should complete the CMS-460 form and submit it to each Medicare Administrative Contractor (MAC)/carrier with which you file Part B claims. It’s crucial to send this form directly to your MAC/carrier and not to CMS to avoid processing delays. The address and exact submission dates can be obtained from the MAC/carrier. Remember to list all names and National Provider Identifier (NPI) numbers under which you file claims on the form. For newly enrolling physicians, practitioners, and suppliers, the form can be submitted along with the Medicare enrollment application.
-
What happens if a physician or supplier chooses not to participate?
If a physician or supplier chooses not to participate in Medicare, they do not need to submit the CMS-460 form. Those who are not currently participating and decide to continue this status do not need to take any action. However, physicians or suppliers who are currently participating and wish to terminate their agreement need to notify each MAC/carrier in writing, with the notice being postmarked before the end of the current calendar year. This action will make their non-participation status effective from the first day of the next calendar year.
Common mistakes
Filling out the CMS-460 form is a crucial step for healthcare providers who decide to participate in the Medicare program. However, errors can occur during this process, affecting the provider's ability to receive payments correctly. Here are eight common mistakes you should avoid:
Not listing all names and the National Provider Identifier (NPI) under which claims are filed. It’s essential to include all relevant names and NPIs to ensure that all your Medicare claims are correctly processed.
Omitting the signature of the participant or the authorized representative if the participant is an organization. This oversight can invalidate the whole agreement.
Forgetting to provide the title of the authorizing signer when the participant is an organization. This detail certifies the authority of the signer.
Failing to include a complete and accurate office phone number, including the area code, which is necessary for any follow-up communication.
Incorrectly assuming this form can be used to opt out of Medicare. Providers wishing to opt out need to follow a different process, and this form will not serve that purpose.
Submitting the form outside of the open enrollment period without realizing that timing is crucial for changing your participation status or becoming a new participant.
Sending the form directly to the Centers for Medicare & Medicaid Services (CMS) instead of the Medicare Administrative Contractor (MAC)/carrier. This common mistake delays processing.
Not utilizing the correct form version or not adhering to the latest instructions. Always check for the most current form and guidelines to ensure compliance.
To participate effectively in Medicare and ensure timely reimbursement, it's vital to fill out and submit the CMS-460 form correctly. Paying close attention to the details and requirements outlined can prevent unnecessary delays and complications in your Medicare participations and claims processing.
Documents used along the form
When professionals choose to participate in Medicare by using the CMS 460 form, their decision is often accompanied by other necessary forms and documents that ensure compliance and smooth operations within the Medicare program. These additional forms and documents play pivotal roles in various facets of Medicare participation, including enrollment, billing, and adherence to stipulated guidelines.
- CMS-855I: This form is the Medicare Enrollment Application for physicians and other providers. Its primary use is for individuals entering the Medicare system for the first time. It collects detailed information about the provider, including qualifications, practice locations, and the services they offer. This form is essential for providers looking to bill Medicare for their services.
- CMS-855R: Used by physicians or other eligible professionals to reassign Medicare benefits, the CMS-855R form enables the redirection of Medicare payments to an organization or other entity. This form is crucial for professionals working within groups or facilities, allowing the entity to receive payments directly from Medicare.
- CMS-588: The Electronic Funds Transfer (EFT) Authorization Agreement form, CMS-588, allows for the electronic transfer of Medicare payments directly to the provider's bank account. This method speeds up the payment process, reducing the reliance on paper checks and enhancing the efficiency of financial transactions within the Medicare framework.
- Advance Beneficiary Notice of Noncoverage (ABN): While not a form submitted to Medicare, the ABN is a critical document that providers use to inform Medicare patients about services Medicare is likely not to cover, indicating the patient may be responsible for payment. This document is vital for transparency and compliance, ensuring patients are adequately informed about their potential financial liabilities.
- Opt-Out Affidavit: For providers choosing not to participate in Medicare, the Opt-Out Affidavit formalizes this decision. By completing this document, a provider agrees not to bill Medicare for services provided to Medicare beneficiaries for a specified period. It's crucial for the provider-patient agreement process for those providers seeking to establish a direct billing relationship with their Medicare patients, outside of the Medicare system.
In summation, the CMS 460 form is part of a broader spectrum of documents that together facilitate a comprehensive and legally compliant interaction with the Medicare program. Whether a provider is enrolling for the first time, managing their billing and payment processes, or deciding to opt-out of Medicare, these documents ensure their compliance and operational effectiveness within the Medicare system. Each document plays a unique and essential role in the provider's Medicare participation journey, from initiation through to the delivery of services and the management of Medicare reimbursement.
Similar forms
The CMS-855I form, which is the Medicare Enrollment Application for Physicians and Non-Physician Practitioners, shares similarities with the CMS-460 form in that both are essential for providers to establish their billing and participation status with Medicare. Specifically, both forms are integral to a provider's ability to bill Medicare for services rendered to Medicare beneficiaries and to define the terms of their participation or non-participation in Medicare programs.
The CMS-855B form, which is the Medicare Enrollment Application for Clinics/Group Practices and Certain Other Suppliers, is similar to the CMS-460 form because it also relates to the Medicare enrollment process. While the CMS-855B focuses on group practices and clinics, the CMS-460 form is about the agreement to accept Medicare's assigned rates. Both forms collectively ensure that the entity or provider is recognized by Medicare for billing purposes.
The CMS-855R form, which is used for Reassignment of Medicare Benefits, has similarities with the CMS-460 form in terms of establishing payment arrangements with Medicare. The CMS-855R allows a provider to reassign their Medicare payments to an organization, which parallels the CMS-460’s role in setting up how a provider will be paid by Medicare by agreeing to accept assignment for all services.
The Opt-Out Affidavit, necessary for providers deciding to opt-out of Medicare, can be considered in conjunction with the CMS-460 form, which is an agreement to participate. While the Opt-Out Affidavit is for those not engaging in Medicare’s assignment system, the CMS-460 defines the acceptance of this system. Both documents define the relationship parameters between the provider and Medicare.
The CMS-588 form, Electronic Funds Transfer (EFT) Authorization Agreement, shares its operational sphere with the CMS-460 form since both need to be in place for a streamlined financial transaction between Medicare and the provider. The CMS-588 facilitates the direct deposit of Medicare payments, reinforcing the CMS-460’s agreement on the payment terms.
The Advance Beneficiary Notice of Noncoverage (ABN) form, while not a provider enrollment document, intersects with the CMS-460 form in practice, as providers who participate in Medicare as outlined in the CMS-460 must understand when an ABN is necessary. This form is used to notify patients when Medicare is unlikely to cover a service, thereby linking back to the provider’s understanding and agreement of Medicare’s payment terms as stated in the CMS-460.
Dos and Don'ts
When filling out the CMS 460 form to participate as a Medicare provider, there are specific dos and don'ts that will help streamline the process and ensure compliance. Following these can help avoid any misunderstandings or potential issues with your Medicare participation status.
Do:- Read the entire form and accompanying instructions carefully before starting. Understanding each section can prevent mistakes.
- Ensure all information is accurate, especially your Name(s) and National Provider Identifier (NPI). This information should match exactly what is on your Medicare records.
- Sign and date the form where required. An unsigned form is not valid and will not be processed.
- Keep a copy of the completed form for your records. This is crucial for future reference or if any disputes arise.
- Submit the form to the correct Medicare Administrative Contractor (MAC) that serves your area. Sending it to the wrong MAC can delay the process.
- Consider consulting with a legal or financial advisor if you have questions about participating in Medicare or the implications for your practice.
- Be mindful of the open enrollment period dates. Timing your submission correctly is crucial for your participation status for the upcoming year.
- Use the most current version of the form to ensure compliance with any new regulations or changes.
- Verify that every section of the form has been filled out to prevent delays in processing.
- Contact your MAC with any questions or uncertainties about the process.
- Leave any required fields blank. Incomplete forms may be returned or rejected.
- Misplace your copy of the filled form. Keeping a copy is important for your own records and future references.
- Forget to check the expiration date on the form to ensure it's still valid.
- Ignore the instructions provided with the form. They are designed to help you fill out the form correctly.
- Assume that participation is the best option for you without considering the specifics of your practice and patient base.
- Submit the form without reviewing it for errors. Double-checking can save you time and hassle.
- Wait until the last minute to decide on your participation status. Procrastination can lead to rushed decisions or missed deadlines.
- Use outdated forms. Always check for the most recent version of the CMS 460 form.
- Attempt to use this form to opt out of Medicare. This form is strictly for participating providers.
- Send your CMS 460 form to CMS directly, as it will delay the processing. Always send it to your designated MAC/carrier.
Misconceptions
Understanding the CMS-460 form can often lead to confusion, partially due to misconceptions about its purpose and implications. The CMS-460 form is integral for healthcare providers within the Medicare system. Here are six common misconceptions about the CMS-460 form and the truths behind them:
- Misconception #1: The CMS-460 form is optional for all healthcare providers.
Truth: The CMS-460 form is critical for providers who choose to participate fully in Medicare by accepting assignment for all Medicare-covered services. This decision directly affects reimbursement rates and the billing process, making it far from optional for those committed to being Medicare participating providers. - Misconception #2: Signing the CMS-460 locks you into participation permanently.
Truth: While signing the CMS-460 does denote agreement to participate in Medicare, this agreement is not permanent. Providers can opt out of their participant status annually during the enrollment period, offering a level of flexibility. - Misconception #3: The CMS-460 form affects only Medicare payments.
Truth: In addition to impacting Medicare fee schedules—where participating providers receive a 5% higher reimbursement—the form also streamlines billing for patients with Medigap insurance, allowing for direct payment of deductibles and coinsurance by these policies to the provider. - Misconception #4: Any provider can use the CMS-460 form to opt out of Medicare.
Truth: The CMS-460 is specifically for those wishing to participate in Medicare. Providers looking to opt out must follow a different process, as outlined by Medicare, which involves submitting an "opt-out" affidavit, not the CMS-460 form. - Misconception #5: The CMS-460 form only needs to be filed once with a single MAC/carrier.
Truth: Providers must submit the CMS-460 form to each Medicare Administrative Contractor with whom they file Part B claims. This ensures that their participation status is recognized across the different jurisdictions where they practice. - Misconception #6: New providers must decide to participate in Medicare immediately.
Truth: New providers have a 90-day window from the date of their Medicare enrollment to decide whether they will participate and submit the CMS-460 form. This grace period allows new enrollees ample time to consider their options and seek guidance.
Understanding these truths can help providers navigate Medicare participation more effectively, ensuring they make informed decisions about their role within the system and their relationship with patients covered by Medicare.
Key takeaways
- The CMS 460 form is an agreement that clinicians fill out to become Medicare participating physicians or suppliers, agreeing to accept assignment for all services provided to Medicare patients.
- By signing this agreement, providers are agreeing to request direct Part B payment from Medicare and cannot charge more than the Medicare approved charge, except for applicable deductibles and coinsurance.
- The agreement becomes effective upon filing with any Medicare Administrative Contractor (MAC) or carrier during the enrollment period, and it automatically renews annually unless terminated.
- Termination of the agreement can occur if the participant notifies each MAC/carrier in writing during the enrollment period near the end of any calendar year or if the Centers for Medicare & Medicaid Services (CMS) finds substantial non-compliance by the participant.
- Participants in this program receive a 5% higher fee schedule amount for services and enjoy direct, timely reimbursement from Medicare.
- Medicare participants can benefit from simplified billing for beneficiaries who have Medigap insurance, as Medicare will forward claims for the coinsurance and deductible amounts to the Medigap insurer, who must pay the participant directly.
- The form stresses that participation allows for "one stop" billing for services provided, facilitating easier and more efficient payment processes for services covered by both Medicare and Medigap policies.
- Providers looking to opt out of Medicare cannot use the CMS 460 form for that purpose; opting out requires a different process that allows physicians and practitioners to set their payment terms with Medicare beneficiaries through private contracts.
Popular PDF Forms
Da 3955 - This form is vital for paratroopers, ensuring their jumps are officially recorded for awards and qualifications.
Vehicle Inspection Forms - Guide thorough inspection of the heating, defrost, and air conditioning systems, ensuring comfort and visibility in all conditions.
Commercial Invoice - The payment terms, such as advance payment or net 30, are outlined, ensuring both parties are clear on the financial agreement.